A comparative study on functional outcome of intertrochanteric femur fractures in elderly treated with bipolar hemiarthroplasty or dynamic hip screw
Received: 15-Jun-2022, Manuscript No. jotsrr-22-66667; Editor assigned: 17-Jun-2022, Pre QC No. jotsrr-22-66667(PQ); Accepted Date: Jul 04, 2022 ; Reviewed: 31-Jul-2022 QC No. jotsrr-22-66667(Q); Revised: 02-Jul-2022, Manuscript No. jotsrr-22-66667(R); Published: 06-Jul-2022, DOI: 10.37532/1897- 2276.2022.17(6).72
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Intertrochanteric (IT) femur fractures comprise approximately ½ of all hip fractures caused by a low-energy mechanism such as a fall from a standing height. These fragility hip fractures occur in a characteristic population with risk factors including increasing age, female gender, osteoporosis, a history of falls, and gait abnormalities. The incidence of intertrochanteric fracture is rising because of an increasing number of senior citizens with osteoporosis. By 2040 the incidence is estimated to be doubled.
Keywords
femurfractures,Intertrochanteric,Intravenousfluids,antibody
Introduction
Intertrochanteric (IT) femur fractures comprise approximately ½ of all hip fractures caused by a low-energy mechanism such as a fall from a standing height. These fragility hip fractures occur in a characteristic population with risk factors including increasing age, female gender, osteoporosis, a history of falls, and gait abnormalities. The incidence of intertrochanteric fracture is rising because of an increasing number of senior citizens with osteoporosis. By 2040 the incidence is estimated to be doubled [1].
In India the figures may be much more problems of these fractures are associated with substantial morbidity and mortality malunion implant failure, cut-out of the head, and penetration into the hip [1-4]. The great financial burden to the family is associated with medical problems like diabetes and hypertension [2,3,5].
Surgery is almost always the recommended treatment as the morbidity and mortality associated with nonoperative treatment historically have been high. Patients often have pre-existing comorbidities that dictate the ultimate outcome [4].
Reduction of intertrochanteric fractures poses great problems and challenges for orthopaedic surgeons due to the special blood supply system of the femoral neck, its anatomic structure and its functional and biomechanical characteristics. The increasing incidence of such challenging injuries makes it absolutely necessary to use an effective and appropriate treatment modality for such patients [5].
There are certain factors which are beyond the control of surgeon for successful treatment: • fracture geometry and stability, • bone quality, • Comminution Factors under the control of the surgeon are: • good reduction, • proper choice of implant, • proper surgical technique, and • Availability of modern operation rooms, the entire set of implants, instrumentation and image intensifier. The factors most significant for instability and fixation failure are: • loss of posteromedial support, • severe comminution, • sub trochanteric extension of the fracture, • reverse oblique fracture • shattered lateral wall • extension into femoral neck area and • poor bone quality [6].
Osteoporosis is particularly important in the fixation of proximal femoral fractures. This can be measured by Singh’s index and bone densitometry.
One of the major problems with these fractures is the rate of patients’ return to their preoperative period level of activity and independence in carrying out daily routines. After suffering one of these fractures, 50% of these patients require assistance in their daily living activities and 25% should receive long-term care [7].
Most of these patients are elderly and with pre-existing comorbidities, and hence can’t be undergoing repeated surgeries. This study will help us acquire data; tailor the treatment to the patient’s needs, and assess which technique is likely to yield a better outcome in which case.
Generally, the aims and treatment modalities of intertrochanteric fracture reductions are different in young and elderly patients. These fractures usually occur as a result of high-energy traumas in young individuals and are associated with severe traumas to other organs. However, such fractures occur in the elderly due to low-energy traumas and poor bone quality. Moreover, there is no consensus in relation to the use of hemiarthroplasty and internal fixation in elderly patients with background medical conditions. Treatment should be defined on an individual basis, depending on fracture pattern, dislocation, activity prior to fracture, level of independence in personal daily activities and the general health status of each patient [8].
Therefore, the present study was undertaken to compare outcomes of reduction of intertrochanteric fractures using internal fixation with the use of Dynamic Hip Screws (DHS) versus bipolar hemiarthroplasty in elderly patients with background medical conditions – with a view to aid the decision-making process.
Materials and Methods
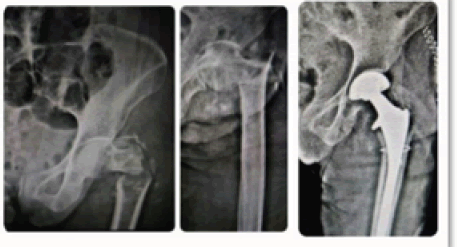
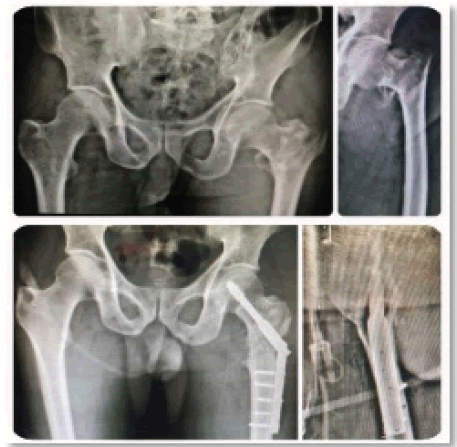
This study was conducted in MGM Medical College and Hospital, Kamothe, Navi Mumbai, Raigad District, Maharashtra between December 2019 to May 2021. A total of 50 patients of age more than or equal to 55 years of age sustaining unstable intertrochanteric fractures according to the Evan’s classification were included in the study. Approval from the Institutional Ethics Committee was obtained and a detailed written informed consent in the language best understood by the patients was taken. These patients were divided into two equal groups of 25 patients, by simple randomization technique, group A patients were treated with Bipolar hemiarthroplasty and Group B patients were treated with Dynamic hip screw fixation (Figure 1 and 2).
The patients included in the study were those aged more than 55 years, patients diagnosed with unstable intertrochanteric femur fractures according to the Evan’s classification and grossly osteoporotic fractures. While patients aged less than 55 years or diagnosed with stable, undisplaced intertrochanteric femur fractures according to the Evan’s classification and patients diagnosed with intertrochanteric fractures with subtrochanteric extension, those diagnosed with pathological fractures and patients with associated other lower limb fractures were excluded from the study. Patients presenting to the casualty of MGM Medical College and Hospital with a history of trauma to the hip joint, were examined clinically and radiologically. They were subjected to Xray of pelvis with both the hip joints and a lateral view of the involved hip joint and were diagnosed with intertrochanteric femur fracture which was classified according to the Jensen and Michaelsen’s classification, Evan’s classification and AO-OTA Classification and all the patients with unstable intertrochanteric fracture were included in the study.
Preoperative evaluation was carried out with blood investigation: CBC, blood group, prothrombin time and INR, renal function test, liver function test, serum electrolytes, chest X ray, electrocardiography and 2D Echocardiography. These investigations were reviewed by anesthesiologists in view of the patients’ general fitness for surgery. Patients were informed regarding the mode of injury, diagnosis, the need for surgery and associated complications and were taken up for the surgery after a written informed consent signed by the patients, one of the patients’ relatives as a witness and a doctor from the team managing the patient.
Preoperatively prophylactic intravenous antibiotics in the form of 1.5 gm Cefuroxime after a test dose was administered 30 mins prior to the incision.
All these patients were operated under regional anesthesia in the form of Spinal + Epidural anesthesia.
The patients belonging to the Group A were placed in true lateral position with the affected limb upper most. The bony prominences, that are the lateral malleolus and the neck of fibula of the lower most leg, were protected with padding as most of these patients have a delicate skin [ 9,10)]. Those who belonged to Group B were placed in supine position with both the legs supported on a fracture table. The non-operative limb was flexed and abducted to allow room for image intensifier for intraoperative radiographs. The operative lower limb was kept in extension and reduction of the fracture was attempted prior to scrubbing and draping and checked under the image intensifier, and were treated with Bipolar hemiarthroplasty and Dynamic hip screw fixation respectively with or without trochanteric fixation with tension band wiring.
Post-operatively Intravenous fluids with IV antibiotics, that is, Inj. Cefuroxime 1.5 gm IV BD for 3 days and Inj. Amikacin 500 mg IV BD for 2 days and subcutaneous Enoxaparin 0.6 mg SC OD for 3 days and IV analgesics were given post operatively. This was followed by oral antibiotics Tab. Cefuroxime 500mg PO BD for 5 days and Tab. Aspirin 150 mg PO OD for 1 month for DVT Prophylaxis. The epidural catheter was kept in situ for 48 hours and topped up every 12-hourly while monitoring the patient’s vital parameters. Patients were allowed a liquid to semi-solid oral diet 4 hours post-operatively. The abduction bar was given to patients of Group.
A where the posterior approach was used to keep the limbs in 20 degrees -30 degrees of abduction. The patient was mobilized on postoperative day one with bedside sitting and toe and ankle movements with calf pumps were started. The catheter was removed after 24 hours postoperatively. On the second postoperative day, patients of Group A were ambulated with weight bearing as tolerated with the help of a physiotherapist. Whereas the patients of Group B were ambulated, non-weight bearing on the second postoperative day with the help of a Zimmer frame and gradually progressed to partial weight bearing walking and then full weight bearing walking depending upon the quality of bone fixation. The dressing was done on the third and eighth post-op days. Suture removal was done on the fourteenth postoperative day. The patients were discharged after the course of intravenous antibiotics and subcutaneous enoxaparin was completed and satisfactory ambulation was achieved for them.
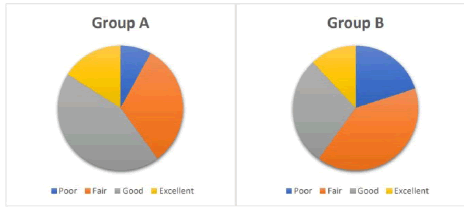
These patients were followed up postoperatively for a minimum of 1 year and assessed on the basis of Harris Hip Score at 3 weeks, 6 weeks, 6 months and 1 year postoperatively and scored according to the scoring system as follows: Poor: <70 Fair <70 Fair: 70-79 Good: 80-89 Excellent: >90.
Result
The mean age of the patients included in the study was 75.88 +/- 8.57 years in the Group A and 67.76 +/- 9.18 years in Group B. The male:female ratio being 72:28% in Group A and 64:36% in Group B which was statistically insignificant with a P-value of 0.544.
The most common mechanism of injury was found to be a trivial slip and fall at home while a few cases of road traffic accident were also reported (Table 1).
Table 1: The two groups were compared on the basis of the following parameters enumerated in the table below.
| Group | Shapiro-Wilk | |||
|---|---|---|---|---|
| Statistic | df | Sig. | ||
| Operative time (in hours) | Bipolar hemiarthroplasty | 0.764 | 25 | 0 |
| DHS | 0.838 | 25 | 0.001 | |
| Intraoperative blood loss (in ml) | Bipolar hemiarthroplasty | 0.889 | 25 | 0.011 |
| DHS | 0.734 | 25 | 0 | |
| Duration of Hospital Stay Post operatively | Bipolar hemiarthroplasty | 0.363 | 25 | 0 |
| DHS | 0.54 | 25 | 0 | |
| Time to full weight bearing walking (in days) | Bipolar hemiarthroplasty | 0.519 | 25 | 0 |
| DHS | 0.408 | 25 | 0 | |
| Harris Hip Score 3 Weeks | Bipolar hemiarthroplasty | 0.944 | 25 | 0.179 |
| DHS | 0.683 | 25 | 0 | |
| Harris Hip Score 6 Weeks | Bipolar hemiarthroplasty | 0.907 | 25 | 0.026 |
| DHS | 0.701 | 25 | 0 | |
| Harris Hip Score 6 Months | Bipolar hemiarthroplasty | 0.619 | 25 | 0 |
| DHS | 0.588 | 25 | 0 | |
| Harris Hip Score 1 Year | Bipolar hemiarthroplasty | 0.593 | 25 | 0 |
| DHS | 0.658 | 25 | 0 | |
The average operative time and intraoperative blood loss was significantly lesser in the dynamic hip screw fixation group as compared to the hemiarthroplasty group. The length of hospital stay postoperatively is shorter in patients treated with bipolar hemiarthroplasty at an average of 7.56 days as compared to 10.68 days in the dynamic hip screw fixation group; however, this difference is statistically insignificant.
The mean number of days required for patients to start full weight bearing walking was 6.12 +/- 2.42 days and 61.28 +/- 10.05 days in the hemiarthroplasty and the dynamic hip screw fixation groups, and this difference was found to be statistically significant.
The final functional outcome was assessed in terms of rate of complication and Harris hip score at the final follow-up after one year.
An overall complication rate of 20% was seen in the hemiarthroplasty group out of which deep infection forcing implant removal was seen in 4%, dislocation of the bipolar prosthesis in 4%, one case (4%) of deep vein thrombosis was noted and 8% cases of limb length discrepancies were reported and 28% in the Dynamic hip screw fixation group, amongst these 8% cases of deep infection, 4% (one) case of deep vein thrombosis, 8% cases of pressure sores and one (4%) case of periprosthetic fracture were observed.
The average Harris hip score was found to be 84.12 +/- 14.01 in the hemiarthroplasty group and 76.52 +/- 17.73 in the dynamic hip screw fixation group at 1-year postoperative follow-up. However, this difference was not statistically significant.
Discussion
A hip fracture in elderly patients represents a disturbing and potentially ominous landmark in their personal health history. For the health care system and society in general, intertrochanteric fractures and other hip fractures represent an epidemic disease. The standard treatment for intertrochanteric fractures is operative as it is associated with less deformity, shorter length of stay in the hospital and quicker rehabilitation. The mortality rate amongst patients with intertrochanteric fractures treated conservatively is significantly higher as compared to patients treated with a surgical line of management.
In our study, we have compared two surgical options for the treatment of intertrochanteric fractures, namely, Bipolar hemiarthroplasty and Internal fixation with Dynamic hip screw.
The observations of our study were compared with the following studies and the outcomes deduced are discussed as follows.
1. Jaswinder Singh Walia et al [11]. 2. Gashi YN et al [12]. 3. Dong-peng Tu et al [13]. 4. Jin-Woo Kim et al [14].
The average time to operate in the studies included in the systematic review done by Dongpeng et al was found to be 1.43 hours for hemiarthroplasty and 1.05 hours for the dynamic hip screw fixation group [13]. Jim-Woo Kim et al observed in their study that the average operative time required for hemiarthroplasty was 1.31 hours and 1.22 hours in the dynamic hip screw fixation group [14]. In our study, the mean operative time was 1.9 hours and 1.36 hours for hemiarthroplasty and dynamic hip screw fixation respectively.
On the basis of the Mann-Whitney U test, we calculated the p-value to be less than 0.05 indicating that the operative time in the hemiarthroplasty group is significantly less than in the dynamic hip screw fixation group
Jim-Woo Kim et al in their study observed that the intraoperative blood loss was 228.4 ml in the dynamic hip screw fixation group while 296.3 ml in the hemiarthroplasty group [14]. In the meta-analysis and systematic review done by Dong-peng et al, it was observed that the average blood loss was 306 ml in the hemiarthroplasty group and 118 ml in the dynamic hip screw fixation group [13].
In our study, it was observed that the average blood loss was 376.2 ml in the hemiarthroplasty group while 313.4 ml in the dynamic hip screw fixation group. The p-value calculated by Mann
Whitney U test was found to be less than 0.05 and an inference was drawn that the mean blood loss is significantly less in the dynamic hip screw fixation group as compared to the hemiarthroplasty group.
In the study conducted by Walia et al, the patients were allowed to start full weight bearing walking after 35 days that is 4 weeks to 6 weeks in the hemiarthroplasty group and after 96 days that is about 12 weeks to 16 weeks in the internal fixation with dynamic hip screw fixation group [11].
In the study conducted by Gashi YN et al, the mean time required for patients to start full weight bearing walking was 7 days and 60 days for the hemiarthroplasty and dynamic hp screw fixation groups respectively [12].
In the meta-analysis and systematic review done by Dong-peng et al, there were 5 studies that described that the overall time required for patients to start full weight bearing walking was much lesser as compared to the internal fixation with the dynamic hp screw group [13].
In our study, it was observed that the mean number of days required for patients to start full weight bearing walking was 6.12 +/- 2.42 days and 61.28 +/- 10.05 days in the hemiarthroplasty and the dynamic hip screw fixation groups, and this difference was found to be significant as the p-value calculated as per the Mann-Whitney U test of significance was less than 0.05. The average duration of stay in the hospital postoperatively was found to be 6.9 days in the hemiarthroplasty group and 11 days in the dynamic hip screw fixation group in the studies included in Dongpeng et al’s meta-analysis [13]. In the study conducted by Jim-Woo Kim et al, the post-operative duration of hospital stay was observed to be 14.4 days and 13.3 days in the hemiarthroplasty and dynamic hip screw fixation groups respectively [14].
In our study, the postoperative duration of stay in the hospital was found to be 7.56 and 10.68 in the hemiarthroplasty and dynamic hip screw fixation group respectively, this difference was statistically insignificant.
In the study conducted by Walia et al, the overall complication rate was observed to be 12.75% in the hemiarthroplasty group and 28% in the dynamic hip screw fixation group. Out of these patients, there was one case of superficial infection, one case of deep vein thrombosis and one case of postoperative pulmonary infection observed in the hemiarthroplasty group. Complications like bed sores seen in two cases, deep vein thrombosis in one case, three cases of superficial infection and two cases of implant cut-out were seen in the dynamic hip screw fixation group [11].
Gashi YN et al described complications like dislocation in two cases, deep vein thrombosis in 4 cases, two cases of superficial infection and 4 cases of deep infection forcing implant removal and 9 cases of bed sore postoperatively, leading to an overall 16.6% infection rate in the hemiarthroplasty group. Whereas, 11 cases of implant cut-out or periprosthetic fractures, 3 cases of deep vein thrombosis, 8 cases of bed sore, infection were seen in 8 patients out of which a deep infection requiring implant removal was seen in 5 cases, with an overall complication rate of 26.6% in the dynamic hip screw fixation group [12]. In the meta-analysis and systematic review conducted by Dongpeng et al, they described an overall infection rate of 19.65% in the hemiarthroplasty group and 25.68% in the dynamic hip screw fixation group. Amongst the studies included in the meta-analysis 6 studies described post-operative infections in the form of need for reoperation in 4.88% of patients and 7.49% of patients treated with hemiarthroplasty and internal fixation with dynamic hip screw, etc respectively. Implantrelated complications were seen in 3.08% and 11.15% of patients, deep vein thrombosis was seen in 4.47% and 4.59 patients and superficial infection was seen in 4.87% and 4.51% patients of the hemiarthroplasty and dynamic hip screw fixation groups respectively. 10 out of the 224 patients that are 4.46%, treated with dynamic hip screw fixation were found to develop non-union of intertrochanteric femur fracture. The overall mortality rate at 1-year follow-up was found to be 11.85% of patients and 10.52% of patients treated with hemiarthroplasty and dynamic hip screw fixation. While at the end of 2 years, the mortality was 15.2% and 15.27% of patients in the hemiarthroplasty and dynamic hip screw fixation groups respectively [13].
The study conducted by Jim-Woo Kim et al focussed on the reoperation rates and mortality indicating an overall complication rate of 10.75% in the hemiarthroplasty group and 12.1% in the dynamic hip screw fixation group in terms of infection need for reoperation and other systemic complications. Out of these, 3.4% of patients needed reoperation in the dynamic hip screw fixation group while no cases needing reoperation were observed in the hemiarthroplasty group. An overall mortality of 27.5% was seen at the end of 24 months in the hemiarthroplasty group while 13.7% in the dynamic hip screw fixation group [14].
In our study, the overall complication rate of 20% and 24% was observed in the hemiarthroplasty and dynamic hip screw fixation groups respectively. In the hemiarthroplasty group, the following postoperative complications were observed, 3 cases of superficial infection, 1 case of deep infection forcing multiple wound wash and debridement and finally implant removal, one case of dislocation of the bipolar prosthesis was seen at 4 months postoperatively and one case of pulmonary thromboembolism was reported, which was managed in the ICU with intravenous Enoxaparin and supportive therapy, after which the patient recovered. Two patients suffered from limb length discrepancies, one with 3cm of shortening and another with 2.5 cm of lengthening. In the dynamic hip screw fixation group, 6 cases of postoperative superficial infection were noted out of which 2 cases were of deep infection leading to implant removal, and one case of deep vein thrombosis was reported and managed with subcutaneous Enoxaparin. Two cases with post-operative bed sores were reported and one case of peri-prosthetic fracture was reported 6 weeks after the surgery. The p-value calculated by tests for statistical significance was more than 0.05 indicating that there is no statistical significance in the difference in the rate of complication between the two groups compared in our study.
In the study conducted by Walia et al, the Harris Hip score at final follow-up after 4 months post-operatively was found to be 83.2 and 8-0.4 in the hemiarthroplasty and the dynamic hip screw fixation groups respectively [11].
In the study by Gashi YN et al, it was observed that the Harris Hip score at the final follow-up after 24 months was 91.14 +/- 5.7 and 74.11 +/- 13.8 in the hemiarthroplasty and the dynamic hip screw fixation groups respectively [12].
In the systematic review and meta-analysis of randomized control trials done by Dong-peng et al, four studies described the outcome on the basis of Harris Hip score and it was observed that there was no statistical significance in the difference between Harris hip scores on the final follow-up amongst the two groups evaluated [13]. In our study the patients were followed up on four occasions post-operatively, that is at 3 weeks, 6 weeks, 6 months and 1 year. It was observed that the Harris hip score of patients in the hemiarthroplasty group was found to be significantly better than the dynamic hip screw fixation group on follow-up at 6 weeks post-operatively. However, at the final followup at 6 months, the average Harris Hip score of the patients in the hemiarthroplasty group was found to be 84.12 with a standard deviation of 14.01 and in the dynamic hip screw fixation group was 76.52 with a standard deviation of 17.73. This difference was found to be statistically insignificant as the p-value calculated by the Mann-Whitney U test was > 0.05.
Functional Outcome in Group A- bipolar hemiarthroplasty and Group B- dynamic hip screw fixation is illustrated in the e form of a pie chart as follows (Figure 3).
Conclusion
Our study suggests that dynamic hip screw fixation needed lesser operative time and was associated with lesser intra-operative blood loss. While bipolar hemiarthroplasty provided faster mobilization and rehabilitation, with lesser immobility-related complications and a shorter duration of postoperative hospital stay. However, the final functional outcome and overall complication rate was found to be similar in both the groups. A study with a larger sample size and a longer duration of follow-up will be needed to warrant one surgical procedure superior to the other in the treatment of unstable intertrochanteric fractures in elderly patients.
References
- Reindl R, et al.: Intramedullary versus extramedullary fixation for unstable intertrochanteric fractures: a prospective randomized controlled trial. J Bone Joint Surg Am. 2015;97(23): 1905-12[CrossRef][Google Scholar]
- Kyle RF, et al.: Fractures of the proximal part of the femur. J Bone Joint Surg Am. 1994;76(6): 924-50[CrossRef] [Google Scholar]
- Haynes RC, et al.: Failure of femoral head fixation: a cadaveric analysis of lag screw cut-out with the gamma locking nail and AO dynamic hip screw. Injury. 1997; 28(5-6): 337-41. [CrossRef] [Google Scholar]
- Wolfgang GL, et al.: Treatment of intertrochanteric fracture of the femur using sliding screw plate fixation. Clin Orthop Relat Res. 1982;163:148-58[CrossRef][Google Scholar]
- Court-Brown CM, Caesar B.: Epidemiology of adult fractures: a review Injury. 2006;37(8):691-7.[CrossRef] [Google Scholar]
- Lavelle DG et al.: Fractures of hip. In: Cambell operative orthopaedics. 10th ed. Philadelphia: 2003;2875-9.[CrossRef] [Google Scholar]
- Dimon JH, Hughston JC.: Unstable intertrochanteric fractures of the hip. J Bone Joint Surg Am. 1967;49:440-50.[CrossRef] [Google Scholar]
- Bridle SH, et al.: Fixation of intertrochanteric fractures of the femur. A randomised prospective comparison of the gamma nail and the dynamic hip screw. J Bone Joint Surg Br. 1991;73:330-34[CrossRef] [Google Scholar]
- Gibson A; Posterior exposure of the hip joint. J Bone Joint Surg Br. 1950;32-B:183-6[CrossRef] [Google Scholar]
- Hardinge K; The direct lateral approach to the hip. J Bone Joint Surg Br. 1982; 64:17-9[CrossRef] [Google Scholar]
- Walia, J.P, et al.: Comparative study between standard dynamic hip screw (DHS) and cemented bipolar arthroplasty in trochanteric fracture of femur in elderly patients. 2018;1:3[CrossRef] [Google Scholar]
- Gashi YN, et al.: Outcome of Primary Cemented Bipolar Hemiarthroplasty compared with Dynamic Hip Screw in
Elderly Patients with Unstable Intertrochanteric Fracture. Malays Orthop J. 2018;12(1):36-41.[CrossRef] [Google Scholar] - Tu DP, et al.: Internal Fixation versus Hemiarthroplasty in the Treatment of Unstable Intertrochanteric Fractures in the Elderly: A Systematic Review and Meta-Analysis. Orthop Surg. 2020 Aug;12(4):1053-64.[CrossRef] [Google Scholar]
- Kim JW, et al.: Reoperation rate, mortality and ambulatory ability after internal fixation versus hemiarthroplasty for unstable intertrochanteric fractures in elderly patients: a study on Korean Hip Fracture Registry. Arch Orthop Trauma Surg. 2020 Nov;140(11):1611-18.[CrossRef] [Google Scholar]



 Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.
Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.