Can we predict functional outcomes following tibial plateau fractures? The Plateau Fracture Indicator Variables Predicting Outcomes of Treatment (PIVOT) score
2 Department of Orthopedic Surgery, Medisys Health Network, Jamaica Hospital Medical Center, Queens, New York, United States, Email: abc@gmail.com
Received: 02-Aug-2020 Accepted Date: Aug 21, 2020 ; Published: 07-Sep-2020
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Objective: This study seeks to establish a score that may be used to identify patients at risk of poor functional outcome after tibial plateau fracture, in order to direct additional resources to that population.
Methods: Demographics, injury information, surgical management, and functional outcomes on the SMFA were prospectively collected from 423 tibial plateau fracture patients. Stepwise forward logistic regression was performed to generate a model predictive of patients’ likelihood of progressing to poor long-term clinical outcome.
Results: Of the 423 patients, 275 had operative intervention and complete data with minimum 12 months followup. Significant predictors of poor outcome were residual depression, general anesthesia, worker’s compensation, tobacco smoking, CCI, racial minority status, and alcohol abstinence. Applied to the validation cohort, it predicted outcomes with 75.9% sensitivity and 69.6% specificity. When functional status at 3 months was taken into account, significant predictors were 3-month SMFA, worker’s compensation, general anesthesia, CCI, and male gender. Applied to the validation cohort, it predicted outcomes with a 90.0% sensitivity and 68.4% specificity. Both models were significant, explaining 24.9% and 24.6% of variance in outcome with an AUC of 0.752 and 0.769, respectively.
Conclusion: The PIVOT model is a good predictor of poor functional outcome following operative repair of tibial plateau fracture.
Design: Prospective, observational study
Setting: Level 1 Trauma Center
Level of Evidence: Level III.
Keywords
Tibial plateau, outcomes predictor, tibial plateau fracture, traumatic fracture
Abbreviations
AUC: Area Under the Curve; CCI: Charlson Comorbidity Index; KOOS: Knee injury and Osteoarthritis Outcome Score; ORIF: Open Reduction Internal Fixation; PIVOT: Plateau Fracture Indicator Variables predicting Outcomes of Treatment; ROC: Receiver Operative Curve; ROM: Range Of Motion; SF-36: Short Form-36S; MFA: Short Musculoskeletal Function Assessment; VAS: Visual Analog Score
Introduction
Tibial plateau fractures account for 1% of all fractures treated in the United States, within incidence of 10.3 per 100,000 annually [1,2]. Open Reduction Internal Fixation (ORIF) with reconstruction of the articular surface remains the mainstay treatment for the majority of patients. While posttraumatic osteoarthritis is a concern in the long term [3,4], many patients return to normal activities by 6-12 months after surgery [5].
The most commonly evaluated outcome assessed in the literature has been functional outcome [6] as evaluated by validated questionnaires such as the Short Musculoskeletal Function Assessment (SMFA), Knee injury and Osteoarthritis Outcome Score (KOOS), and SF-36 scores. Poor functional outcomes in the SMFA questionnaire have been linked to poor clinical outcomes and vice-versa, with a 10-point difference correlating to measurable differences in walking speed and capability [7-9]. Other measures of interest include continued postoperative pain [6], radiographic malalignment or failure of fixation, intraoperative complications [10], development of posttraumatic arthrosis [11], and unplanned reoperation [12].
Many studies have evaluated functional outcome following operative treatment of tibial plateau fractures and found risk factors associated with poor functional outcome. Common risk factors among these studies include but are not limited to advanced age, malalignment of the mechanical axis of the tibia, fracture classification, and reduction quality among other factors [13-16]. The ability to detect risk factors for poor functional outcome is vital to the management of patients with this injury as it may allow the surgeon to initiate aggressive and specialized physical therapy for those at high risk of poor overall outcome. In this study, we sought to develop an internally validated risk assessment capable of identifying patients’ high risk for having a poor outcome following ORIF of tibial plateau fracture, the “Plateau fracture Indicator Variables predicting Outcomes of Treatment (PIVOT) model.”
Materials and Methods
Between 2005-2017, 423 tibial plateau fractures treated by three surgeons at a single institution was prospectively followed with data recorded contemporaneously in an IRB approved registry. Demographics, injury information (including Schatzker, Moore and AO/OTA classification) [17,18], surgical management, pre and postoperative radiographic parameters, postoperative knee Range of Motion (ROM) as well as follow-up Short Functional Musculoskeletal Assessment (SMFA) scores were collected. Data collected was purely observational as treatment of all patients, including operative planning, was entirely at the discretion of the attending surgeon [7-9].
Eligibility criteria for this study included patients at least 18 years of age who underwent operative treatment for tibial plateau fracture, and possessing a minimum of 12 months follow-up. Patients treated nonoperatively (66) and those with less than 1 year follow up (82) were excluded.
All patients participated in a structured physical therapy program starting at 2 weeks postoperatively which consisted of active and graduated passive knee range of motion, graduated quadriceps and hamstring strengthening, and weight bearing initiated at 10-12 weeks post-operatively based on radiographic healing. Poor functional outcome was defined as any patient with a functional SMFA>10 points above the median at most recent follow-up visit, provided that most recent follow up was at least 12 months following operation (>21.4). SMFA scores at this level have been shown to be one standard deviation above the mean in normative data and associated with worse clinical outcomes and capabilities.
Of these 275 patients, two-thirds were randomly selected to build the predictive model, while the remaining one-third was used to validate the generated model. Patient population characteristics are defined in Table 1. Stepwise forward logistic regression was used to build the predictive formulae for long-term SMFA after injury. Two predictive models were generated in this manner, one utilizing only information available upon initial hospitalization and a second incorporating the patient’s 3-month SMFA score. This was done in order to simulate the ability of the physician to refine their assessment of a patient as their clinical course progresses.
| Characteristic | Number | Percentage |
|---|---|---|
| Total | 275 | 100.0 |
| Sex | ||
| Male | 146 | 53.1 |
| Female | 129 | 46.9 |
| Minority status | ||
| Yes | 169 | 61.5 |
| No | 106 | 38.5 |
| Charlson Comorbidity Index | ||
| 0 | 214 | 77.8 |
| 1 | 45 | 16.4 |
| 2 | 11 | 4.0 |
| 3 | 4 | 1.5 |
| 7 | 1 | 0.4 |
| Psychiatric illness | ||
| Yes | 264 | 96.0 |
| No | 11 | 4.0 |
| Tobacco smoker | ||
| Yes | 220 | 80.0 |
| No | 55 | 20.0 |
| Alcohol use | ||
| Yes | 173 | 62.9 |
| No | 102 | 37.1 |
| Illicit substance use | ||
| Yes | 15 | 5.5 |
| No | 260 | 94.5 |
| Worker's compensation | ||
| Yes | 263 | 95.6 |
| No | 12 | 4.4 |
| Injury mechanism | ||
| High energy | 203 | 73.8 |
| Low energy | 72 | 26.2 |
| Additional fracture | ||
| Yes | 186 | 67.6 |
| No | 89 | 32.4 |
| Compartment syndrome | ||
| Yes | 6 | 2.2 |
| No | 269 | 97.8 |
| Vascular injury | ||
| Yes | 3 | 1.1 |
| No | 272 | 98.9 |
| Nerve injury | ||
| Yes | 4 | 1.5 |
| No | 271 | 98.5 |
| Open fracture | ||
| Yes | 11 | 4.0 |
| No | 264 | 96.0 |
| Tibial spine involvement | ||
| Yes | 108 | 39.3 |
| No | 163 | 59.3 |
| Schatzker class | ||
| Class i | 4 | 1.5 |
| Class ii | 138 | 50.2 |
| Class iii | 7 | 2.5 |
| Class iv | 31 | 11.3 |
| Class v | 22 | 8.0 |
| Class vi | 73 | 26.5 |
| OTA class | ||
| OTA B | 182 | 66.2 |
| OTA C | 93 | 33.8 |
| Spinal anesthesia | ||
| Yes | 60 | 21.8 |
| No | 210 | 76.4 |
| Postoperative malalignment | ||
| Yes | 9 | 3.3 |
| No | 263 | 95.6 |
| Characteristic | Range | Mean |
| Age | 19-86 years | 48.1 years |
| BMI | 17.5-47.0 Kg/m2 | 27.3 Kg/m2 |
| Preoperative fracture depression | 0-40 mm | 8.2 mm |
| Postoperative fracture depression | 0-6.4 mm | 0.5 mm |
Table 1: Demographic characteristics included in logistic regression
Variables in the analysis include sex, age, BMI, Charlson Comorbidity Index (CCI), open fracture, high-energy injury mechanism, workers compensation, presence of a vascular or nerve injury, mm of tibial plateau depression on initial presentation, tibial spine fracture, OTA 41 B vs. 41 C fracture type, and residual plateau depression postoperatively (Table 1). The two analyses differed only in their inclusion of 3-month SMFA score.
Stepwise forward logistic regression was used with entry testing based on the significance of the “score statistic” (entry<0.05) and removal testing based on the probability of the Wald statistic (removal>0.10). No outliers were removed. The constant number created for our equation is inherent to our statistical analysis methodology and has been used and validated in previous studies [19,20]. Regression coefficients were calculated and are reported as 95% confidence intervals. The assumptions of linearity, independence of errors, homoscedasticity, unusual points and normality of residuals were met.
Results
275 patients were prospectively followed for an average of 19.7 months (Range: 12-127 months). Based on our definition of a poor functional outcome, patients with SMFA>21.4 were determined to have a poor functional outcome at long-term follow up.
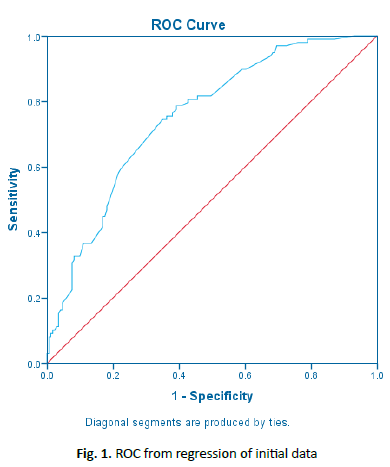
At long-term follow-up, initial variables determined to be significant predictors of poor outcome were worker’s compensation insurance (B=2.337; p=0.012), tobacco smoking (B=1.013; p=0.016), CCI (B=0.472; p=0.021), postoperative depression (B=0.304; p=0.03), identification as a racial minority (B=0.770; p=0.037). Conversely, social alcohol use (B=-0.810; p=0.034) and operative use of spinal anesthesia (B=-1.247; p=0.022) were associated with better functional outcomes (Table 2). The final model, created through stepwise forward logistic regression, (Table 3) was statistically significant (χ2 (7)=37.574, p<0.0005) and explained 24.9% (Nagelkerke R2) of the variance in outcome. AUC for the model was 0.752. A Receiver Operator Curve (ROC) a cutoff value of 0.360 (1-specificity, x-axis) was chosen for the model which equated to a sensitivity of 74% and a specificity of 64% (Fig. 1). When applied to the validation cohort, it predicted poor outcomes with a sensitivity of 75.9% and specificity of 69.6%.
| 95% CI for Exp (B) | |||||||
|---|---|---|---|---|---|---|---|
| B | SE | Wald | p-value | Exp(B) | Lower | Upper | |
| Minority status | 0.77 | 0.369 | 4.364 | 0.037 | 2.16 | 1.049 | 4.45 |
| CCI | 0.472 | 0.205 | 5.288 | 0.021 | 1.603 | 1.072 | 2.396 |
| Smoker | 1.013 | 0.419 | 5.841 | 0.016 | 2.754 | 1.211 | 6.262 |
| Alcohol use | -0.81 | 0.381 | 4.511 | 0.034 | 0.445 | 0.211 | 0.939 |
| Worker's compensation | 2.337 | 0.933 | 6.276 | 0.012 | 10.35 | 1.663 | 64.419 |
| Postoperative depression | 0.304 | 0.14 | 4.723 | 0.03 | 1.356 | 1.03 | 1.784 |
| Spinal anesthesia | -1.247 | 0.542 | 5.283 | 0.022 | 0.287 | 0.099 | 0.832 |
| Constant | -1.284 | 0.358 | 12.843 | 0 | 0.277 | 0 | 0 |
Table 2: Variables resulting from regression of initial patient data
| e^(-1.284+0.77[Minority*]+0.472[cci†]+1.013[Smoker*]-0.81[Social drinker*]+2.337[Worker's compensation*]+0.304[Post-op depression‡]-1.247[Spinal anesthesia*]) |
| 1+e^(-1.284+0.77[Minority*]+0.472[cci†]+1.013[Smoker*]-0.81[Social drinker*]+2.337[Worker's compensation*]+0.304[Post-op depression‡]-1.247[Spinal anesthesia*]) |
*Minority, smoker, social drinker, worker’s compensation, and spinal anesthesia are dichotomous variables with a value of 1 if true and 0 if not true
†CCI is the patient’s Charlson Comorbidity Index
‡Post-op depression is the patient’s residual depression in mm following ORIF
Table 3: PIVOT score from regression of initial patient data
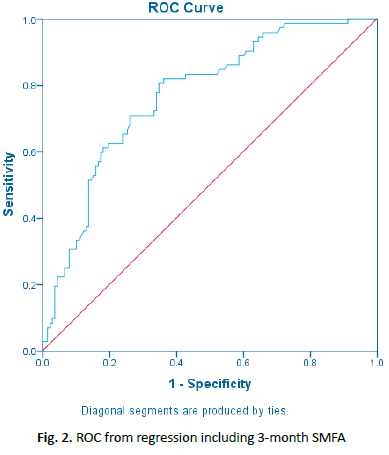
When functional status at 3 months was taken into account, significant predictors of poor outcome were standardized 3-month SMFA index (B=0.041; p=0.002), worker’s compensation insurance, (B=2.706; p=0.008), and CCI (B=0.476; p=0.049). Female gender, conversely, was associated with better functional outcome (B=-0.911; p=0.030) and use of spinal anesthesia was associated with better outcomes (B=-1.730; p=0.017) (Table 4). The model (Table 5) was statistically significant (χ2 (5)=37.157, p<0.0005) and explained 24.6% (Nagelkerke R2) of the variance in outcome. AUC for the model was 0.769. A Receiver Operative Curve (ROC) cutoff value of 0.300 (1-specificity, x-axis) was chosen for the model which equated to a sensitivity of 72% and a specificity of 70% (Fig. 2). When applied to the validation cohort, it predicted poor outcomes with a sensitivity of 90.0% and specificity of 68.4%. Refer to Table 6 for sample baseline and 3-month PIVOT score calculations.
| 95% CI for Exp (B) | |||||||
|---|---|---|---|---|---|---|---|
| B | SE | Wald | p-value | Exp(B) | Lower | Upper | |
| Female gender | -0.911 | 0.419 | 4.374 | 0.030 | 0.402 | 0.177 | 0.914 |
| CCI | 0.476 | 0.242 | 3.886 | 0.049 | 1.610 | 1.003 | 2.585 |
| Worker’s compensation | 2.706 | 1.028 | 6.935 | 0.008 | 14.975 | 1.998 | 112.234 |
| Spinal anesthesia | -1.730 | 0.689 | 6.309 | 0.012 | 0.177 | 0.046 | 0.684 |
| 3-month SMFA Index | 0.041 | 0.013 | 9.692 | 0.002 | 01.042 | 1.015 | 1.069 |
| Constant | -1.886 | 0.576 | 10.736 | 0.001 | 0.152 | 0 | 0 |
Table 4: Variables resulting from regression including 3-month SMFA
| e^(-1.886-0.911[female*]+0.476[CCI†]+2.706[worker's compensation*]-1.73[spinal anesthesia*]+0.041[3 Month Standardized SMFA‡]) |
| 1+e^(-1.886-0.911[female*]+0.476[CCI†]+2.706[worker's Compensation*]-1.73[spinal anesthesia*]+0.041[3 Month Standardized SMFA‡]) |
*Female, worker’s compensation, and spinal anesthesia are dichotomous variables with a value of 1 if true and 0 if not true.
†CCI is the patient’s Charlson Comorbidity Index
‡3-month standardized SMFA is the patient’s standardized total SMFA score at 3 months
Table 5: PIVOT score from regression including 3-month follow-up
| Sample PIVOT calculation with initial patient data: | ||||||||
| Racial minority | Smoker | Worker's compensation | Spinal anesthesia | Post-op depression | Social drinker | CCI | PIVOT score | |
| Patient 1 | No | No | No | Yes | 1 mm | Yes | 1 | 0.0714 |
| Patient 2 | Yes | Yes | No | Yes | 3 mm | No | 0 | 0.541 |
| Patient 1 has a PIVOT score of 7.14%, which is considered “low risk” for poor outcome Patient 2 has a PIVOT score of 54.10%, which is considered “high risk” for poor outcome |
||||||||
| Sample PIVOT calculation with patient data at 3-month follow-up: | ||||||||
| Female | CCI | Worker's compensation | Spinal anesthesia | Standardized total SMFA | PIVOT score | |||
| Patient 3 | Yes | 0 | No | Yes | 18.5 | 0.0542 | ||
| Patient 4 | No | 1 | Yes | No | 23.9 | 0.907 | ||
Patient 3 has a PIVOT score of 5.42%, which is considered “low risk” for poor outcome
Patient 4 has a PIVOT score of 90.7%, which is considered “high risk” for poor outcome
Table 6: Sample PIVOT calculations
Discussion
The aim of operative fixation of tibial plateau fractures is threefold: joint stabilization, reconstruction of the tibial articular surface, and promotion of early range-of-knee motion. Despite these goals, there is a spectrum of functional recovery seen with this fracture pattern. The goal of this study was to characterize risk factors that portended a poor functional outcome that could be identified throughout a patient’s clinical course. We were able to develop a reproducible predictive score to identify patients at risk for poor functional outcome.
Of the risk factors identified in this study for developing a poor functional outcome, tobacco use, alcohol use, and utilization of spinal anesthesia were the only modifiable risk factors. Smoking has been demonstrated to have deleterious effects with fracture healing [21]. There is little literature regarding the effect of smoking on overall functional recovery in patients with fractures. However, smoking has been shown to be a risk factor for requiring manipulation under anesthesia in patients who have undergone primary total knee arthroplasty indicating a propensity towards knee stiffness [22]. Smoking is known to be associated with poor wound healing, infection, and nonunion in fractures, also potentially contributing to poor outcomes [23]. Identification of this modifiable risk factor early in the management of tibial fractures allows for treatment of smoking in such a way that will minimize wound and fracture healing complications and allow for maximal functional recovery. The correlation between social alcohol use and improved functional outcome has previously been noted in another study [24]. Its etiology is not well-understood and merits further exploration. The results concerning the use of regional anesthesia is congruent with benefits that have been established in existing literature [25].
Insofar as non-modifiable risk factors are concerned, workers compensation insurance status is well-established in the literature as a risk factor for poor subjective outcomes following surgery [26], including a variety of orthopedic procedures [27-29]. This effect is consistent throughout the literature and among meta-analyses. Ethnic minority status has been extensively explored in the literature relating to general surgery [30,31], and prior research suggests that ethnic differences exist in outcomes following arthroplasty [32] spine surgery [33], and in outcomes following lower extremity fracture [34]. However, previous research from our group suggested that race was not an independent risk factor for poor outcome following treatment of all tibial plateau fractures [35] Meanwhile, CCI has been previously revealed to be a predictor of functional outcome following surgery, as well as a risk factor for in-hospital mortality and adverse events [36-38].
Recent publications by Konda et al. have laid the groundwork for developing targeted algorithms for directing resource utilization in the context of orthopedic trauma [19,39]. The vast amounts of extant data contained within electronic health records show considerable promise in allowing providers to uncover previously unseen correlations. In an era of rapid technological advancement where algorithms have revolutionized nearly every facet of daily life and saved significant amounts of money and healthcare resources, we must use every tool at our disposal to combat skyrocketing healthcare costs.
One limitation of this study is its sample size. While a cohort of 275 patients is a sizable population for regression analysis, it was effectively reduced by one-third through the use of an internal validation cohort. A greater study population would enable generation of a more precise model and creation of a smoother, more accurate ROC curve to better set the cutoff value. Furthermore, if the size of the validation cohort were increased, it would allow for evaluation of the algorithm with less risk of statistical error.
Although a 10-point difference from the mean SMFA at 12 months is a reasonable threshold for a poor outcome 7-9, using a larger threshold (20 points) would provide higher specificity and positive predictive value in order to better differentiate those with significant postoperative disability. We chose not to use a larger threshold based on our sample size, as using a larger threshold significantly decreased the number of poor outcome patients, precluding a meaningful analysis. Larger patient populations with standardized functional outcome scores can be used in the future to modify the PIVOT model accordingly.
Conclusion
We believe the novel PIVOT score can be used as a risk assessment tool for short and long-term postoperative function. For patients with a high PIVOT score (poor outcomes) at the outset of treatment, physicians can institute early, directed interventions geared towards improving function and range-of-motion. This would follow principles of value-based care by optimizing patient function for a select few poor performing patients at the expense of additional resource intensive interventions.
Cutoff values were determined by visual examination of ROC to optimize both sensitivity and specificity but may be adjusted if emphasis on one metric were desired. The incorporation of cost data into models may help individuate cutoff values on an institution-by-institution basis in order to aid physicians in making cost-conscious decisions.
The incorporation of functional status at 3 months postoperatively allows the physician to alter their treatment plan to the needs of the patient as those needs evolve during the course of treatment, enhancing the potential utility of this model. In particular, while there is a lack of literature on rehabilitation following tibial plateau fracture, future studies can stratify “high-risk” and “low-risk” PIVOT score populations to determine if aggressive physical therapy can be used to improve outcomes in at-risk populations.
Clinicians who wish to use the PIVOT score to guide therapy interventions can go to this free website (www.orthopredict.wordpress. com) to input patient variables and calculate the risk of poor outcome as well as receive recommendations on value-based pathways to optimize short and long-term patient function. Similarly, clinicians can paste the equation into an excel document and enter each individual variable to calculate the score.
REFERENCES
- Egol K.A., Koval K.J., Zuckerman J.D.: Handbook of fractures: Fifth edition. 2018.
- Elsoe R., Larsen P., Nielsen N.P.H., et al.: Population-based epidemiology of tibial plateau fractures. Orthopedics. 2015;38:e780-e786.
- Wasserstein D., Henry P., Paterson J.M., et al.: Risk of total knee arthroplasty after operatively treated tibial plateau fracture a matched-population-based cohort study. JBJS. 2014;96:144-150.
- Jansen H., Frey S.P., Doht S., et al.: Medium-term results after complex intra-articular fractures of the tibial plateau. J Orthop Sci. 2013;18:569-577.
- Urruela A.M., Davidovitch R., Karia R., et al.: Results following operative treatment of tibial plateau fractures. J Knee Surg. 2013;26:161-166.
- Mcnamara I.R., Smith T.O., Shepherd K.L., et al.: Surgical fixation methods for tibial plateau fractures. Cochrane Database Syst Rev. 2015;9.
- Hunsaker F.G., Cioffi D.A., Amadio P.C., et al.: The American Academy of Orthopaedic Surgeons outcomes instruments: Normative values from the general population. JBJS. 2002;84:208-215.
- Swiontkowski M.F., Engelberg R., Martin D.P., et al.: Short musculoskeletal function assessment questionnaire: Validity, reliability, and responsiveness. JBJS. 1999;81:1245-1260.
- Hoffmann M.F., Sietsema D.L., Jones C.B.: Lost to follow-up: Reasons and outcomes following tibial plateau fractures. Eur J Orthop Surg Traumatol. 2016;26:937-942.
- Biz C., Maso G., Gambato M., et al.: Challenging surgical treatment of displaced articular tibial plateau fractures: Do early knee radiographic features have a predictive value of the mid-term clinical functional outcomes? Orthop Surg. 2019;11:1149-1162.
- Aurich M., Koenig V., Hofmann G.: Comminuted intraarticular fractures of the tibial plateau lead to posttraumatic osteoarthritis of the knee: current treatment review. Asian J Surg. 2018;41:99-105.
- Henry P., Wasserstein D., Paterson M., et al.: Risk factors for reoperation and mortality after the operative treatment of tibial plateau fractures in Ontario. 1996-2009. J Orthop Trauma. 2015;29:182-188.
- Ahearn N., Oppy A., Halliday R., et al.: The outcome following fixation of bicondylar tibial plateau fractures. Bone Joint J. 2014;96:956-962.
- Parkkinen M., Madanat R., Mustonen A., et al.: Factors predicting the development of early osteoarthritis following lateral tibial plateau fractures: mid-term clinical and radiographic outcomes of 73 operatively treated patients. Scand J Surg. 2014;103:256-262.
- Van Dreumel R.L.M., Van Wunnik B.P.W., Janssen L., et al.: Mid- to long-term functional outcome after open reduction and internal fixation of tibial plateau fractures. Injury. 2015;46:1608-1612.
- Yao Y., Lv H., Zan J., et al.: Functional outcomes of bicondylar tibial plateau fractures treated with dual buttress plates and risk factors: A case series. Injury. 2014;45:1980-1984.
- Schatzker J., McBroom R.: The tibial plateau fracture. The Toronto experience 1968-1975. Clin Orthop Relat Res. 1979;138:94-104.
- Kellam J.F., Meinberg E.G., Agel J., et al.: Fracture and dislocation classification compendium-2018. 2018;32:S1.
- Konda S.R., Seymour R., Manoli A., et al.: Development of a middle-age and geriatric trauma mortality risk score: A tool to guide palliative care consultations. Bull Hosp Joint Dis. 2016;74:298.
- Konda S.R., Carlock K.D., Hildebrandt K.R., et al.: Predicting functional outcomes following fracture nonunion repair-development and validation of a risk profiling tool. J Orthop Trauma. 2020;34:214-220.
- Cusano N.E.: Skeletal effects of smoking. Curr Osteoporos Rep. 2015;13:302-309.
- Issa K., Rifai A., Boylan M.R., et al.: Do various factors affect the frequency of manipulation under anesthesia after primary total knee arthroplasty? Clin Orthop Relat Res. 2015;473:143-147.
- Chang C.J., Jou I.M., Wu T.T., et al.: Cigarette smoke inhalation impairs angiogenesis in early bone healing processes and delays fracture union. Bone Joint Res. 2020;9:99-107.
- Saleh H., Driesman A., Fisher N., et al.: Social to moderate alcohol consumption provides a protective effect for functional outcomes after fixation of orthopaedic fractures. J Orthop Trauma. 2017;31:173-178.
- Vadivelu N., Kai A.M., Maslin B., et al.: Role of regional anesthesia in foot and ankle surgery. Foot Ankle Spec. 2015;8:212-219.
- Harris I., Mulford J., Solomon M., et al.: Association between compensation status and outcome after surgery: A meta-analysis. J Am Med Assoc. 2005;293:1644-1652.
- Cheriyan T., Harris B., Cheriyan J., et al.: Association between compensation status and outcomes in spine surgery: A meta-analysis of 31 studies. Spine J. 2015;15:2564-2573.
- De Moraes V.Y., Godin K., Tamaoki M.J.S., et al.: Workers’ compensation status: Does it affect orthopaedic surgery outcomes? A meta-analysis. PLoS One. 2012;7:e50251.
- Kadzielski J.J., Bot A.G.J., Ring D.: The influence of job satisfaction, burnout, pain, and worker’s compensation status on disability after finger injuries. J Hand Surg Am. 2012;37:1812-1819.
- Hall E.C., Hashmi Z.G., Zafar S.N., et al.: Racial/ethnic disparities in emergency general surgery: Explained by hospital-level characteristics? Am J Surg. 2015;209:604-609.
- Bloo G.J.A., Hesselink G.J., Oron A., et al.: Meta-analysis of operative mortality and complications in patients from minority ethnic groups. Br J Surg. 2014;101:1341-1349.
- Kamath A.F., Horneff J.G., Gaffney V., et al.: Ethnic and gender differences in the functional disparities after primary total knee arthroplasty. Clin Orthop Relat Res. 2010;468:3355-3361.
- Skolasky R.L., Thorpe R.J., Wegener S.T., et al.: Complications and mortality in cervical spine surgery: Racial differences. Spine. 2014;39:1506-1512.
- Driesman A., Fisher N., Konda S.R., et al.: Racial disparities in outcomes of operatively treated lower extremity fractures. Arch Orthop Trauma Surg. 2017;137:1335-1340.
- Driesman A., Mahure S.A., Paoli A., et al.: Race and ethnicity have a mixed effect on the treatment of tibial plateau fractures. J Orthop Trauma. 2017;31:309-314.
- Kabboord A.D., Van Eijk M., Fiocco M., et al.: Assessment of comorbidity burden and its association with functional rehabilitation outcome after stroke or hip fracture: A systematic review and meta-analysis. J Am Med Dir Assoc. 2016;17:1066-1013.
- Schouten R., Keynan O., Lee R.S., et al.: Health-related quality-of-life outcomes after thoracic (T1-T10) fractures. Spine J. 2014;14:1635-1642.
- Shields E., Sundem L., Childs S., et al.: Factors predicting patient-reported functional outcome scores after humeral shaft fractures. Injury. 2015;46:693-698.
- Konda S.R., Lott A., Saleh H., et al.: How does frailty factor into mortality risk assessment of a middle-aged and geriatric trauma population? Geriatr Or



 Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.
Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.