Combined percutaneous retrograde intramedullary pinning and open reduction and screw fixation in the treatment of displaced Neer three-part fractures of the humerus
2 Orthopaedic surgeon at Mohamed Taher Maamouri Hospital, Nabeul, Tunisia, Email: walid_bouaicha@yahoo.fr
3 Registrar in Orthopaedics and Trauma, Nabeul, Tunisia
4 Associate Professor at the Faculty of Medicine of Tunis, Tunisia
Received: 31-Jul-2023, Manuscript No. jotsrr-23- 108637; Editor assigned: 02-Aug-2023, Pre QC No. jotsrr-23-108637 (PQ); Accepted Date: Aug 21, 2023 ; Reviewed: 14-Aug-2023 QC No. jotsrr-23-108637 (Q); Revised: 16-Aug-2023, Manuscript No. jotsrr-23-108637 (R); Published: 23-Aug-2023
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Introduction: Fractures of the proximal humerus are common injuries. Treatment options vary according to fracture patterns, surgeon preferences and implant availability. Increasing interest is being given to minimally invasive surgical procedures. In this article an original surgical procedure is described combining Percutaneous Retrograde Intramedullary Pinning (PRIP) and open reduction with lag screw fixation in the treatment of displaced near three-part fractures of the proximal humerus.
Methods: We report on the preliminary results of a retrospective series of six patients treated with PRIP and open lag screw fixation reviewed with a mean follow-up of 25 months. Radiologic assessment was made on plain x-rays. Functional results were assessed according to the Constant and Murely score, the Disabilities of The Arm, Shoulder And Hand (DASH) score, and the Analogue Visual Score (AVS).
Result: Radiologic reduction was “anatomical” in all the patients. The average Absolute Constant Score (ACS) was 55.16 (range from 30 to 80). The average DASH score was 27.3 (range from 19 to 36). Only one case of proximal pin migration was reported.
Conclusion: The association of PRIP with open reduction and lag screw fixation can be an interesting alternative yielding good results in our developing countries where more advanced fixation devices are not readily available.
Keywords
Proximal humerus fracture, percutaneous pinning, open reduction internal fixation. minimally invasive surgery
Introduction
Fractures of the proximal humerus still generate debate over their best treatment options without any literature supporting the superiority of any procedure on the mid to long-term results [1].
To date, there is no clear consensus regarding the best surgical procedure indicated in displaced fractures and many treatment options are available to orthopaedic surgeons [2, 3].
There is an increasing trend towards head preservation techniques rather than arthroplasty even in highly displaced fractures especially with the progresses made in bone fixation options since the introduction of locked plates. Complication rates, however, remain high despite advances made [4].
Avascular Necrosis (AVN) of the humeral head has been often related not only to the initial displacement and damage to the vascular supply but also to the amount of soft tissue disruption caused during surgery.
For this reason, increasing attention is being given to minimally invasive techniques such as percutaneous pinning [5-9]. However, obtaining an accurate reduction of the greater tuberosity through a percutaneous approach remains technically challenging.
Most authors agree that successful outcomes are more likely when the tuberosities are anatomically reduced, for this reason we thought about a procedure that associates the advantages of percutaneous fixation without compromising on the quality of reduction of the greater tuberosity in complex displaced fractures [7,10,11].
Our study describes a new therapeutic approach to surgical treatment of proximal humerus fractures and reports its preliminary functional and radiological results.
Materials and Methods
We report a retrospective study conducted at the Orthopedics and Trauma Department at a tertiary hospital.
From January 2014 to December 2019, six patients underwent surgical treatment for displaced fractures of the proximal humerus using a combined technique associating Open Reduction and Internal Fixation (ORIF) of the greater tuberosity with lag screws and a Percutaneous Retrograde Intramedullary Pinning (PRIP) as described by Hackethal and modified by De La Caffinière [12, 13].
All the patients were available for a minimum one-year follow-up (mean 25 months, range: 12 months to 34 months).
The patients’ records were reviewed to collect epidemiologic, radiologic and therapeutic parameters. All the patients were evaluated with radiographs and physical examination at the time of their latest follow-up.
SURGICAL TECHNIQUE AND POST-OPERATIVE CARE
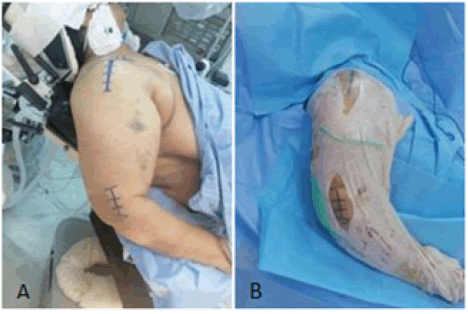
The surgical procedures were performed under general anaesthesia with the patient in the modified “beach chair” position (Fig. 1A).
Reduction manoeuvre of the surgical neck fracture component is performed under fluoroscopic guidance to insure that close reduction and orthogonal views can be obtained.
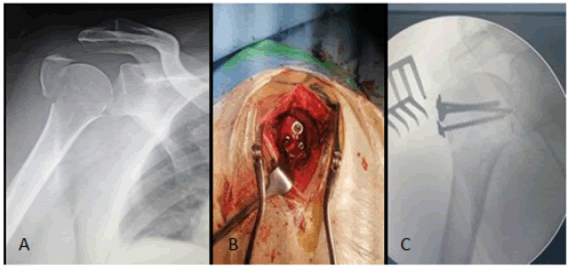
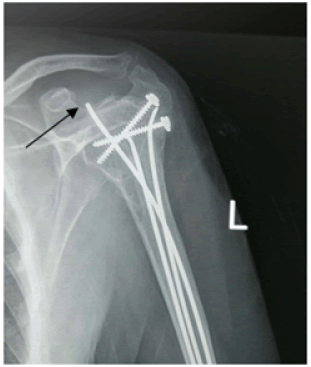
After sterile draping, a four-centimetre supero-lateral incision is made starting from the lateral edge of the acromion (Fig. 1B). This incision should not be extended more than five centimetres distally to avoid injury to the axillary nerve. Blunt dissection is then carried on to develop an interval through the fibres of the deltoid muscle. In a Neer three-part displaced fracture (Fig. 2A), an open reduction of the greater tuberosity is achieved under direct visual control and stabilized with 3.5 mm cancellous screws mounted on washers (Fig. 2B). The number of the screws depends on the size and the degree of comminution of the tuberosity fragment (Fig. 2C).
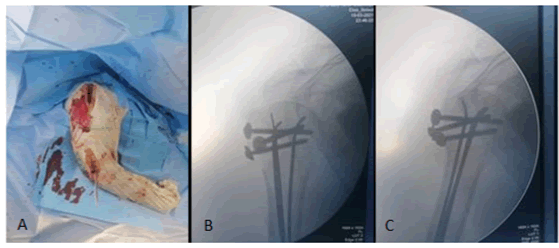
The second step of the procedure is then started with a 3 cm incision on the lateral aspect of the distal humerus (Fig. 1B). A large enough entry point is made with an awl roughly three centimetres above the lateral condyle. Three 25 to 30 /10th elastic nails are advanced from distal to proximal with fluoroscopic guidance to the level of the fracture site (Fig. 3A). Reduction manoeuvre is then attempted with progressive longitudinal traction with the shoulder abducted to 70° to 80°. During this manoeuvre, a posterior directed pressure on the shaft is made to counteract the typical anterior displacement. Once an acceptable reduction is achieved on fluoroscopy, the three pins are advanced through the fracture and into the sub-chondral bone of the humeral head in a divergent way. The final position of the pins is checked fluoroscopically in orthogonal planes to insure their extra-articular placement (Fig. 3B and 3C). Stability of the fixation is assessed with gentle rotations of the shoulder.
At the end of the procedure, the skin incisions are closed and the upper limb immobilized in a sling.
Physiotherapy is initiated with passive protected mobilization followed by progressive active range of motion of the shoulder. Removal of hardware was not mandatory for the initiation of rehabilitation.
EVALUATION OF THE FUNCTIONAL RESULTS
All the patients were examined at their latest follow-up at the outpatient clinic.
The shoulder joint was assessed for stiffness and the range of motion of the glenohumeral joint in anterior flexion, abduction, external and internal rotation noted.
The scoring system as described by Constant and Murley was used to assess the functional result at the latest follow-up: Absolute Constant’s Score (ACS) [14]. Both shoulders were assessed separately and the ACS of the injured side was compared to the contralateral side and expressed in percentage [15, 16].
The Disabilities of the Arm, Shoulder and Hand (DASH) score was also used for the functional assessment of the patients at their latest followup as well as the Visual Analogue Scale (VAS) [17].
EVALUATION OF THE RADIOLOGIC RESULTS
All fractures were classified according to initial x-rays using the Neer and AO classification systems [18].
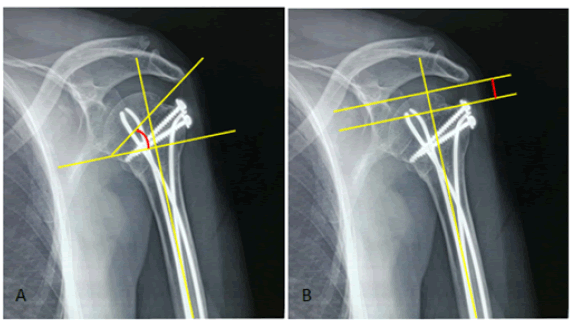
Immediate post-operative x-rays including Antero-Posterior (AP) and true lateral views were assessed by two senior consultants. Three criteria were measured:
1. The Alfa angle: (Fig. 4A). Normal: 30° to 60°.
2. Greater tuberosity displacement: measures the proximal displacement of the greater tuberosity in the frontal plane (Fig. 4B).
3. Translation
4. Shortening.
A reduction is considered “anatomical” when all the following four criteria are met:
1. Greater tuberosity displacement less than 5mm
2. Alfa angle of 45° +/- 15°
3. Translation less than 5mm
4. Shortening of less than 5mm
The last follow-up x-rays including AP and lateral views were examined for: Fracture healing, tuberosity union, loss of reduction (Alfa angle difference), signs of Avascular Necrosis (AVN) and signs of post traumatic arthritis.
POST-OPERATIVE COMPLICATIONS
The patient’s records were scrutinized for early post-operative complications such as sepsis, hematomas and neurovascular complication, as well as late post-operative complications including sepsis, joint stiffness of the elbow and/or the shoulder, regional complex pain syndrome, sub-acromial impingement, pin migration, malunions and nonunions.
Results
The records of six patients were included in this retrospective study. They were four women and two men (sex ratio 2:1). The mean age at the time of injury was 69 years (range, fifty-six to eighty-five). The injured side was predominantly the right-hand side (four patients). The mechanism of injury was a domestic fall in all our patients but one in whom it was a motor vehicle accident. Fractures were classified as Neer three-part in all the patients corresponding to the type B1 of the AO classification system.
All surgical procedures were done under general anaesthesia with the patient in the “beach chair” position. The mean surgical time was 63.3 mn (range 45 mn to 105 mn). The mean hospital stay after surgery was two days and all patients were discharged with a shoulder immobilization that was kept for a mean period of 41 days. After removal of the immobilization, a physical therapy was prescribed to all patients for a mean duration of 76 days.
The patients were reviewed after a mean follow-up period of 25 months (range 12months to 34 months)
RADIOGRAPHIC ASSESSMENT
All the fractures healed at a mean timeframe of 49 days. The mean post-operative Alfa angle was 50° (range 41° to 56°). All our reductions were qualified as “anatomic” according to the four criteria previously mentioned. No AVN of the humeral head or post traumatic arthritis was reported as well as any loosening, loss of reduction or implant failure. However, in one patient we noted a proximal migration of the pins.
FUNCTIONAL ASSESSMENT
The functional results are presented in the table (Table 1).
Table 1. Functional Results
| Patient | Gendre | Age | Type of injury | Injured side | Range of motion (°) (FF/Abd/ER) | ACS/Weighted score (%) | DASH score | AVS satisfaction |
|---|---|---|---|---|---|---|---|---|
| 1 | F | 62 | DF | Right | 120/115/40 | 62/88 | 23 | Satisfied |
| 2 | F | 85 | DF | Left | 110/100/45 | 62/95 | 21 | Very satisfied |
| 3 | F | 67 | DF | Right | 100/100/40 | 47/67 | 35 | Satisfied |
| 4 | M | 56 | MVA | Right | 150/140/60 | 80/92 | 19 | Very satisfied |
| 5 | F | 66 | DF | Right | 100/120/45 | 50/71 | 30 | Satisfied |
| 6 | M | 78 | DF | Left | 90/80/20 | 30/39 | 36 | Unsatisfied |
*Functional results (F: female, M: male, DF: domestic fall, MVA: Motor Vehicle Accident, FF: Forward Flexion, Abd: abduction, ER: External Rotation, ACS: Absolute Constant Score, Weighted score: in percentage compared to uninjured side, DASH: Disabilities of the Arm, Shoulder and Hand, AVS: Analogue Visual Score)
The average Absolute Constant Score (ACS) was 55.16 (range from 30 to 80).When compared to the opposite side, this mean weighted score reaches 75.5% (range from 39% to 95%). According to the ACS, the results were excellent in three patients, good in two and bad in one patient. The average DASH score was 27.3 (range from 19 to 36).
On the Visual Analogue Scale, three patients were very satisfied, two patients were satisfied and one patient was unsatisfied.
COMPLICATIONS
There were no early post-operative complications noted.
Two patients (33%) presented at their 3 weeks’ appointment with superficial wound sepsis due to pin irritation at the insertion point of the elastic nails, all of them subsided with wound care and antibiotics. At the latest follow-up, two patients (33%) had minimal shoulder stiffness; no elbow stiffness was reported and only one case (16.6%) of pin migration was noted (Fig. 5).
Discussion
Proximal humerus fractures are of common occurrence in daily trauma practice. Their prognosis depends not only on the pattern of the fracture but also on the quality of the bone in which they occur, the age and medical condition of the patient and the treatment option applied.
The treatment of complex proximal humerus fractures has always been a challenge for orthopaedic surgeons for decades. Although most authors agree that successful outcomes are more likely when the tuberosities are anatomically reduced [7,10, 11] and the shoulder is mobilized early, there is no consensus on the most successful surgical procedure to achieve both goals [19, 20]. This resulted in a myriad of procedures including percutaneous pinning, intramedullary nailing, hemiarthroplasty, and Open Reduction and Internal Fixation (ORIF) using a multitude of implants, which have all failed to yield consistently good or excellent clinical results [7, 10, 21]. These techniques have each their own strengths and weaknesses.
Amongst all available options, open reduction and internal fixation offers the best chances of an anatomical reduction and stable fixation allowing for early range of motion, however this method requires an extensive soft tissue stripping to obtain both adequate exposure and rigid fixation [8, 10, 11]. In fact, the greater tuberosity fragment is usually externally rotated (superior and posterior displacement) under the pull of the rotator cuff muscles, this makes achieving reduction and fixation of this fracture difficult through a classic anterior delto-pectoral approach and extensive soft tissue release is sometimes mandatory to obtain adequate exposure [22, 23]. In some cases, detaching the deltoid origin or insertion and/or the pectoralis major insertion at least partially is necessary to access this fragment [2, 22-25].
Gallo et al. went as far as to associate a supero-lateral approach to the classic anterior delto-pectoral approach in open reduction and internal fixation of complex proximal humerus fractures to improve the reduction of the greater tuberosity fragment [21].
It is well established that, with the advent of fixed-angle locked proximal humerus plates, ORIF with locking anatomical plates is associated with the best radiologic and functional results and is more adequate for fractures fixation in osteoporotic bone [26]. These advantages are counterbalanced by the risks of joint screw penetration, loss of reduction and joint stiffness due to large soft tissue dissection.
Percutaneous pinning, although minimizing soft tissue disruption, requires a longer period of shoulder immobilization, a good bone stock for stability of the fracture fixation and exposes to loss of reduction and pin migration [6]. Furthermore, fluoroscopically guided percutaneous reduction of the greater tuberosity can only be indicated in minimally displaced fractures as suggested by Jaberg et al [6].
Barnes et al described the surgical technique of close reduction and percutaneous pinning of proximal humerus fractures reporting the possibility of percutaneous lag screws and concluded that “Reduction can be difficult with this limited incision technique” [27].
We believe that our surgical management of the Neer three-part fractures using a combined open lag screw fixation and PRIP offers an original compromise between the two procedures and to the best of our knowledge this is the first series describing the association of these two techniques reported in the English literature.
The first surgical step consists in an open reduction of the greater tuberosity fragment using a classic supero-lateral approach. In our experience, this approach greatly facilitates the reduction of the greater tuberosity under direct visual control, which is viewed by some as the key to a successful outcome [8,10, 11]. After this first step is achieved, the three-part fracture is technically transformed into a two-part fracture. At this stage and under fluoroscopic guidance, three 20 to 30/10th pins are inserted in a retrograde manner into the medullary canal and through the neck of humerus fracture after close reduction is obtained.
This Percutaneous Intramedullary Retrograde Pinning (PRIP) technique was first described by Hacketal et al in 1961 to treat midshaft fractures of the humerus [12, 13]. De la Caffinière in 1988 described a modification to the original technique by changing the entry to a point 3 cm to 4 cm above the lateral condyle and that was the technique we used in our study .This surgical technique has the advantage to preserve the humeral head vascular supply by minimizing soft tissue dissection and provide solid fixation by the means of a diverging anchoring of the pins into the sub-chondral bone allowing for a shorter immobilization period with some authors prescribing immediate mobilization [28, 29].
In our study, we postponed shoulder passive range of motion to four to six weeks post operatively because of the predominance of old aged patients with signs of osteopenia to avoid possible secondary displacement.
The two mostly reported complications of the PRIP were per-operative fractures at the pins’ entry point and pin migration. In a series of 136 Neer two-part neck of humerus fractures treated with PRIP, Putz et al. reported two per-operative fractures (1.5%) and 14 intra-articular pin migrations (10%) [30].
In our study, one case of pin migration was reported and resulted in the removal of the hardware at three months post-operatively. No peroperative fractures and no elbow post-operative stiffness occurred.
At the latest fallow-up, our results were overall satisfactory with good radiologic and functional results and little complications.
The main strength of this study is that it reports an original surgical technique in the treatment of Neer three-part proximal humerus fractures. In the context of our developing countries where locked anatomical plates and intramedullary nails are not readily available for obvious economic reasons, this technique combination can be an interesting alternative.
The limitations, however, are the small sample size and a short follow-up period allowing us to report only preliminary results of this technique. In fact, AVN rates increase considerably with follow-up. Harrison et al. reported that AVN of the humeral head occurred in 4% of the patients after an average follow-up of 35 months, this same rate in the same series of patients climbed as high as 26% of the patients after an average 84 months’ follow-up [1]. For this reason, a larger number of patients and a longer follow-up period are needed to draw more definite conclusions.
Conclusion
We present a surgical combination of open and percutaneous techniques that aims to reducing soft tissues damage without compromising on the quality of reduction in displaced Neer three-part proximal humerus fractures. The preliminary results of this technique seem encouraging for the treatment of carefully selected patients and may provide a good alternative where more sophisticated implants such as antegrade intramedullary nails and locked plates are not readily available in developing countries.
References
- Harrison AK, Gruson KI, Zmistowski B, et al. Intermediate outcomes following percutaneous fixation of proximal humeral fractures. JBJS. 2012 Jul 3;94(13):1223-8. [Google Scholar] [Cross ref]
- Hawkins RJ, Bell RH, Gurr K. The three-part fracture of the proximal part of the humerus. Operative treatment. JBJS. 1986 Dec 1;68(9):1410-4. [Google Scholar] [Cross ref]
- Williams GR, Wong KL. Two-part and three-part fractures: open reduction and internal fixation versus closed reduction and percutaneous pinning. Orthopedic Clinics. 2000 Jan 1;31(1):1-21. [Google Scholar] [Cross ref]
- Brunner F, Sommer C, Bahrs C, et al. Open reduction and internal fixation of proximal humerus fractures using a proximal humeral locked plate: a prospective multicenter analysis. Journal of orthopaedic trauma. 2009 Mar 1;23(3):163-72. [Google Scholar] [Cross ref]
- Chen CY, Chao EK, Tu YK, et al. Closed management and percutaneous fixation of unstable proximal humerus fractures. Journal of Trauma and Acute Care Surgery. 1998 Dec 1;45(6):1039-45. [Google Scholar] [Cross ref]
- Jaberg H, Warner JJ, Jakob RP. Percutaneous stabilization of unstable fractures of the humerus. JBJS. 1992 Apr 1;74(4):508-15. [Google Scholar] [Cross ref]
- Jakob RP, Miniaci AN, Anson PS, et al. Four-part valgus impacted fractures of the proximal humerus. The Journal of Bone & Joint Surgery British Volume. 1991 Mar 1;73(2):295-8. [Google Scholar] [Cross ref]
- Resch H, Povacz PA, Fröhlich R, et al. Percutaneous fixation of three-and four-part fractures of the proximal humerus. The Journal of Bone & Joint Surgery British Volume. 1997 Mar 1;79(2):295-300. [Google Scholar] [Cross ref]
- Bogner R, Hübner C, Matis N, et al. Minimally-invasive treatment of three-and four-part fractures of the proximal humerus in elderly patients. The Journal of Bone & Joint Surgery British Volume. 2008 Dec 1;90(12):1602-7. [Google Scholar] [Cross ref]
- Gerber C, Werner CM, Vienne P. Internal fixation of complex fractures of the proximal humerus. The Journal of Bone & Joint Surgery British Volume. 2004 Aug 1;86(6):848-55. [Google Scholar] [Cross ref]
- Rees J, Hicks J, Ribbans W. Assessment and management of three-and four-part proximal humeral fractures. Clinical Orthopaedics and Related Research®. 1998 Aug 1;353:18-29. [Google Scholar] [Cross ref]
- Bouaicha W, Jlidi M, Kharrat M, e. Combined percutaneous retrograde intramedullary pinning and open reduction and screw fixation in the treatment of displaced Neer three-part fractures of the humerus. Research Square [Google Scholar] [Cross ref]
- De la Caffinière JY, Benzimra R, Lacaze F, Chaine A. Intramedullary pinning for humeral diaphysis fractures. A minimal risk osteosynthesis. 82 cases. Revue de Chirurgie Orthopedique et Reparatrice de L'appareil Moteur. 1999 May 1;85(2):125-35. [Google Scholar] [Cross ref]
- Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clinical orthopaedics and related research. 1987 Jan 1(214):160-4. [Google Scholar] [Cross ref]
- Constant CR, Gerber C, Emery RJ, et al. A review of the Constant score: modifications and guidelines for its use. Journal of shoulder and elbow surgery. 2008 Mar 1;17(2):355-61. [Google Scholar] [Cross ref]
- Katolik LI, Romeo AA, Cole BJ, et al. Normalization of the Constant score. Journal of shoulder and elbow surgery. 2005 May 1;14(3):279-85. [Google Scholar] [Cross ref]
- Hudak PL, Amadio PC, Bombardier C, et al. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder, and head). American journal of industrial medicine. 1996 Jun;29(6):602-8. [Google Scholar] [Cross ref]
- Papakonstantinou MK, Hart MJ, Farrugia R, et al,. Interobserver agreement of N eer and AO classifications for proximal humeral fractures. ANZ Journal of Surgery. 2016 Apr;86(4):280-4. [Google Scholar] [Cross ref]
- Bhandari M, Matthys G, McKee MD. Four part fractures of the proximal humerus. Journal of orthopaedic trauma. 2004 Feb 1;18(2):126-7. [Google Scholar] [Cross ref]
- Misra A, Kapur R, Maffulli N. Complex proximal humeral fractures in adults—a systematic review of management. Injury. 2001 Jun 1;32(5):363-72. [Google Scholar] [Cross ref]
- Gallo RA, Zeiders GJ, Altman GT. Two-incision technique for treatment of complex proximal humerus fractures. Journal of orthopaedic trauma. 2005 Nov 1;19(10):734-40. [Google Scholar] [Cross ref]
- Schlegel TF, Hawkins RJ. Displaced proximal humeral fractures: evaluation and treatment. JAAOS-Journal of the American Academy of Orthopaedic Surgeons. 1994 Jan 1;2(1):54-66. [Google Scholar] [Cross ref]
- Hawkins RJ, Kiefer GN. Internal fixation techniques for proximal humeral fractures. Clinical Orthopaedics and Related Research®. 1987 Oct 1;223:77-85. [Google Scholar] [Cross ref]
- Martini M. The sub-deltoid approach to the metaphyseal region of the humerus. JBJS. 1976 Apr 1;58(3):377-9. [Google Scholar] [Cross ref]
- Naranja RJ, Iannotti JP. Displaced three-and four-part proximal humerus fractures: evaluation and management. JAAOS-Journal of the American Academy of Orthopaedic Surgeons. 2000 Nov 1;8(6):373-82.. [Google Scholar] [Cross ref]
- Gardner MJ, Helfet DL, Lorich G. Has locked plating completely replaced conventional plating?. AMERICAN JOURNAL OF ORTHOPEDICS-BELLE MEAD-. 2004 Sep 1;33:440-6. [Google Scholar] [Cross ref]
- Herscovici Jr D, Saunders DT, Johnson MP, et al. Percutaneous fixation of proximal humeral fractures. Clinical Orthopaedics and Related Research®. 2000 Jun 1;375:97-104. [Google Scholar] [Cross ref]
- Apprill G, Boll P. Le traitement des fractures du col de l’humérus par embrochage centro-médullaire sans ouverture du foyer de fracture. Rev Chir Orthop. 1968;54(7):657-66. [Google Scholar] [Cross ref]
- Vichard PH, Bellanger P, Laurain JM. Place de l’enclouage bipolaire ascendant aux clous élastiques dans le traitement des fractures non engrénées de l’extrémité supérieure de l’humérus. Mem Acad Chir. 1982;108:381-9. [Google Scholar] [Cross ref]
- Putz P, Arias C, Bremen J, et al. Le traitement des fractures de l'epiphyse proximale de l'humerus par embrochage fascicule selon Hackethal: a propos de 136 cas. Acta orthopaedica belgica. 1987;53(1):80-7. [Google Scholar] [Cross ref]



 Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.
Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.