Comparative study of anterior cruciate ligament reconstruction versus conservative treatment among non-athletes: A 10-years follow-up
2 DNB Trainee ,Department of Orthopaedics, Sir Ganga Ram Hospital, Rajinder Nagar, New Delhi, India
3 Senior Consultant, Department of Orthopaedics, Sir Ganga Ram Hospital, Rajinder Nagar, New Delhi, India
Received: 12-Feb-2018 Accepted Date: Mar 26, 2018 ; Published: 29-Mar-2018
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Objective: To compare outcome of conservative versus operative treatment for complete Anterior Cruciate Ligament (ACL) tear in non-athletes.
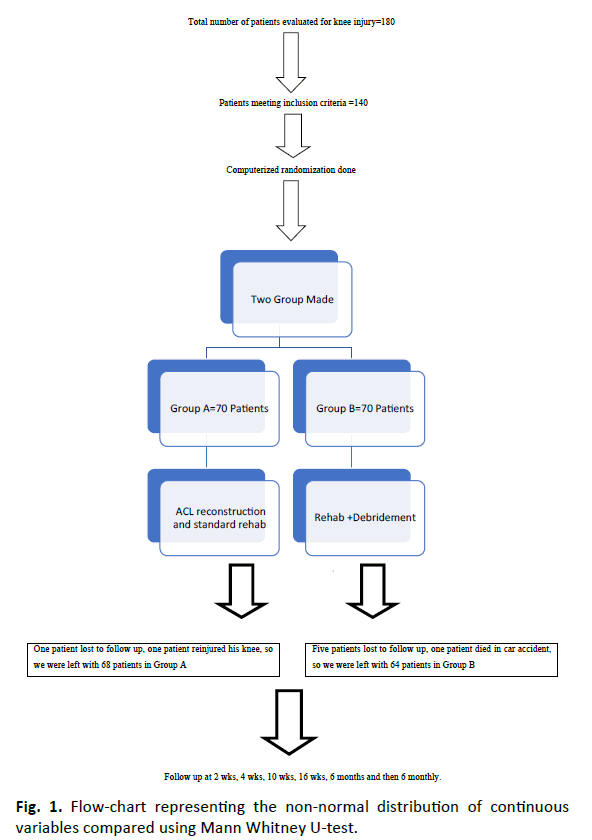
Methods: This was a prospective randomized controlled trial, total 132 Patients were enrolled and two groups were made of 68 patients in group A and 64 in group B. Group A patients were treated surgically (Arthroscopic ACL reconstruction and rehabilitation) and group B patients were treated conservatively (optional debridement and rehabilitation). The outcomes were compared using anterior laxity of knee joint (by using Lachman’s and Pivot shift test), Knee injury and Osteoarthritis Outcome Score (KOOS), International Knee Documentation Committee (IKDC) score and Tegner Activity Level (TAL).
Results and Discussion: The IKDC score at final follow-up was 73.58 (SD ± 2.72) and 72.88 (SD ± 2.69) in group A and B respectively and difference was not significant (p=0.140). The KOOS at final follow-up was 77.75 (SD ± 2.42) and 76.79 (SD ± 3.10) in group A and B respectively and difference was not significant (p=0.052). The TAL at final follow-up was 4.07 (SD ± 0.76) and 3.94 (SD ± 0.75) in group A and B respectively and difference was not significant (p=0.304). At final follow up the reconstructed group showed a positive pivot shift in 29.4% of the cases (10.3% grade 2 and 19.1% grade 1), and positive Lachman test in 29.4% (7.4% grade 1A and 22.1% grade 2A) cases. The patients in non-operative group showed positive Pivot shift (54.7% grade 1 and 45.3% grade 2) and positive Lachman test (46.9% grade 1B and 53.1% grade 2B). Although in term of instability surgically treated group was found better but functionally there was no difference between two groups.
Conclusion: This study revealed both the conservatively treated and the reconstructed group, performed similarly, except for a higher objectively measurable instability in the conservative group. However, they are just as satisfied with their knee without an operation at final follow-up, showing no difference in activity level and functional outcome subjectively. Therefore, conservative treatment should still be considered a treatment option for an ACL insufficient knee in non-athletes.
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Keywords
ACL reconstruction, Conservative management, Non-athletes
Abbreviations
ACL: Anterior Cruciate Ligament, IKDC: International Knee Documentation Committee score, KOOS: Knee injury and Osteoarthritis Outcome Score, LCL: Lateral Collateral Ligament, MCL: Medial Collateral Ligament, MCB: Motion Control Brace, OPD: Out Patient Department, PCL: Posterior Cruciate Ligament, ROM: Range Of Motion, SD: Standard Deviation, TAL: Tegner Activity Level
Introduction
Rupture of the Anterior Cruciate Ligament (ACL) is a serious knee injury that affects mainly physically active young people. The injury is characterized by joint instability that leads to decrease activity, unsatisfactory knee function and poor knee-related quality of life in short term [1,2] and in long term associated with osteoarthritis of knee [3].
One of the great difficulties in ACL rupture management is that there are no specific management guidelines to decide which patient benefits from operative versus non-operative treatment. This is partly because there are few prospective studies comparing operative and non-operative treatment of ACL injuries [4].
Nonsurgical treatment following ACL injury is less frequently reported, especially in recent years, and unfortunately non-surgical treatment was poorly defined in studies comparing surgical and non- surgical treatment [5,6].
This study was a prospective randomized controlled trial involving young, active adults (non- athletes with Tegner Activity Level up to 5) with an acute tear of the ACL to determine whether a strategy of structured rehabilitation plus early ACL reconstructive strategy is superior to a strategy of conservative treatment (arthroscopic debridement if needed plus structured rehabilitation).
Materials and Methods
This study was conducted in department of orthopaedics at 675 bedded multispecialty tertiary care hospital in Delhi. The study was a prospective randomized controlled analysis of cases having complete ACL tear. Study was done between February 2004 to July 2006. All the patients attending emergency or Out Patient Department (OPD) of our hospital with knee injury were evaluated for ACL tear. Patients who met inclusion criteria and gave consent for participation in the study were randomized (using computer randomization technique) into two groups of 70 patients each. Group A patients underwent arthroscopic ACL reconstruction + rehabilitation and group B patients were treated conservatively (Arthroscopic debridement+ rehabilitation) [7,8].
After taking informed consent, all subjects were provided a self-administered patient questionnaire containing Knee injury and Osteoarthritis Outcome Score (KOOS), International Knee Documentation Committee (IKDC) score and Tegner Activity Level (TAL) scores. Surgeon questionnaire was completed at the time of surgery and included history of knee injury, general and knee examination (including tests for anterior laxity- Lachman test and Pivot shift test), radiological examination and surgical technique used for procedure. All patients were examined during follow up clinically for instability (Lachman and Pivot shift test) and IKDC, KOOS, TAL scores were taken and recorded. One independent orthopaedic surgeon kept all records and evaluated results [9-11].
Inclusion criteria
1. Age between 18 to 35 years
2. Either sex
3. Isolated ACL tear not more than 4 weeks old to a previously uninjured knee
4. TAL up to 5.
Exclusion criteria
1. Professional athletes
2. Collateral ligament rupture
3. Full thickness cartilage lesion visualized
4. TAL 6 or more than 6
5. Meniscal tear grade III on MRI.
Statistical Method
Statistical testing conducted with the statistical package for the social science system version SPSS 17.0. Continuous-variables presented as mean SD or median if the data is unevenly distributed. Categorical variables expressed as frequencies and percentages. Comparison of normally distributed continuous variables between the groups performed using Student’s t test. Nominal categorical data between the groups compared using Chi- square test or Fischer’s exact test as appropriate. Non-normal distribution continuous variables compared using Mann Whitney U test. For all statistical tests a p-value less than 0.05 taken to indicate significant difference. The details of the all these cases were collected according to performa attached in the flow chart (Fig. 1).
Baseline variables were comparable and other variables such as Meniscal tear grade III on MRI, TAL 6 or more than 6 were excluded from the study. Therefore, we didn’t use multivariate analysis in our study to adjust the confounding effect of variables on the outcomes of the study.
Surgical technique in group A: All patients were examined under general anaesthesia anteromedial and anterolateral arthroscopic portals were made after which routine diagnostic arthroscopy was performed. Meniscal injury and articular cartilage lesion were ruled out. Four- strand, single bundle hamstring graft prepared from harvested semitendinosus and gracillis tendon (harvested from ipsilateral knee). ACL reconstruction was done using transportal technique. The tibial tunnel was made with an ACL tibial guide set at 50-degree angle, and femoral tunnel was made from anteromedial portal at 10‘o’ clock or 2‘o’ clock position according to the side of knee using femoral guide. After that tibial guide pin was placed in appropriate position, reaming was done to the pre-determined graft size. The femoral tunnel was made leaving a 3mm posterior wall and reamed to appropriate size. Then the graft with endobutton was passed from tibial to femoral tunnel using suture rail-road technique. Femoral fixation was done using endobutton. Then cycling of graft was done by passive flexion and extension before final tibial fixation with BIORCI HA screw or metal screw. Wound closure was done in layers and aseptic sterile dressing was applied and compression bandage was given to all patients. Postoperative on table examination was done by Lachman and Pivot shift test and their grading were noted.
Procedure done in group B patients
All the patients of group B were found symptomatic in our study; all of these had history of locking and severe pain so we did arthroscopic debridement in these patients. Like group A all patients were examined under general anaesthesia after which routine diagnostic arthroscopy was performed. Meniscal injury and articular cartilage lesion were evaluated and patients having meniscal injury or articular defect were not included in the study. Loose body if any removed and stump of ruptured ACL debrided. Post-operative on table examination done for anterior laxity of knee (Lachman and Pivot shift tests) and noted in performa.
Post-operative management and rehabilitation protocol
After surgery patient was shifted to recovery room and long knee brace was applied in group A patients. Intravenous antibiotic given for one post-operative day. Patient discharged on next day of surgery. Rehabilitation started from post-op day one.
In group A (Standard rehab) [12]
1. Post-op day 1: Brace in full extension till one week convert in to Motion Control Brace (MCB) within one week, quadriceps (quad) and hamstring (hams) exercises, partial weight bearing ambulation with crutches.
2. 0- 2 weeks: Range of Motion (ROM) up to 90 degrees, brace in full extension, partial weight bearing 50% to 75%, good quad, 4-way Straight Leg Raise (SLR).
3. 2 to 4 weeks: ROM up to 120 degrees, quad and hams strengthening, full weight-bearing without crutches, close chain exercises.
4. 4-6 weeks: Full flexion up to 6 weeks, discontinue brace, increase close chain exercises.
5. 8-10 weeks: Increases muscle strengthening.
6. 4 months: Jumping rope, running up to 5 months and hopping up to 6 months (Table 1).
| Variables | Group A (N=68) | Group B (N=64) | P-value |
|---|---|---|---|
| Sex Ratio (M:F) | 55:13 | 56:8 | 0.299 |
| Age (Mean ± SD) | 27.41  ±  5.48 | 27.28  ±  5.21 | 0.889 |
| Bmi (Mean ± SD) | 24.30  ±  3.04 | 25.15  ±  3.09 | 0.115 |
Table 1. Age, sex and BMI distribution.
For group B [13]
1. Acute phase, 0-2 weeks: Control pain and swelling, restore pain free ROM, improve flexibility, normalize gait mechanics, establish good quadriceps activation and weight bearing with crutches until demonstrates normal gait mechanics.
2. Sub-acute/strengthening phase, 2-6 weeks: Avoid patella femoral pain, maintain ROM and flexibility, restore muscle strength, improve neuromuscular control and discontinue crutches if have not already
3. Limited return to activity phase, more than 6 weeks: Maintain ROM and flexibility, progress with single leg strengthening to maximize strength, progress dynamic proprioception exercises to maximize neuromuscular control and initiate light jogging.
4. Return to normal activities: Maintain adequate ROM, flexibility and strength, continue progressive/dynamic strengthening, proprioceptive, plyometric and agility training (Table 1).
Role of care management model [14]
I In our study four physiotherapists trained for rehab protocol, were coined the role of care manager. For the purpose of proper rehab and follow-up, strong cooperation and collaboration was established among members of team consisting of patients, care managers and specialists. Care manager constantly monitored and assisted the patients on daily basis for compliance to adhere to rehab protocol.
Specialist (One independent orthopaedic surgeon) examined the patients during follow up clinically for instability (Lachman and Pivot shift test). IKDC, KOOS, TAL scores were taken and recorded. He kept all the records and evaluated results.
Results
Both groups were comparable in terms of Age, sex and side distribution.
Patients reported outcomes
The IKDC score at 6 months was 77.41 (SD ± 2.71) in group A and 77.26 (SD ± 2.14) in group B. The difference between the two groups was not significant on statistical analysis (p=0.731), at final follow-up the scores were 73.58 (SD ± 2.72) and 72.88 (SD ± 2.69) in group A and B respectively and difference was not significant (p=0.140). The KOOS score at 6 months was 82.09 (SD ± 2.25) in group A and 81.25 (SD ± 3.09) in group B. The difference between the two groups was not significant on statistical analysis (p =0.079), at final follow-up the scores were 77.75 (SD ± 2.42) and 76.79 (SD ± 3.10) in group A and B respectively and difference was not significant (p=0.052). The TAL at 6 months was 4.38 (SD ± 0.60) in group A and 4.23 (SD± 0.56) in group B. The difference between the two groups was not significant on statistical analysis (p=0.144), at final follow-up the scores were 4.07 (SD ± 0.76) and 3.94 (SD ± 0.75) in group A and B respectively and difference was not significant (p=0.304) (Table 2).
| Variables | Group A (n=68) | Group B (n=64) | P-value |
|---|---|---|---|
| IKDC | Mean ± SD | Mean ± SD | |
| Pre-op | 34.57 ± 2.01 | 34.14 ± 1.60 | 0.184 |
| 6 wks | 51.39 ± 1.84 | 50.72 ± 2.37 | 0.075 |
| 16 wks | 66.22  ±  1.48 | 64.74  ±  1.82 | <0.001 |
| 6 months | 77.41  ±  2.71 | 77.26  ±  2.14 | 0.731 |
| Final Follow up | 73.58 ± 2.72 | 72.88 ± 2.69 | 0.140 |
| KOOS | Mean ± SD | Mean ± SD | P-value |
| Pre op | 38.54 ± 1.69 | 38.19 ± 1.40 | 0.199 |
| 6 wks | 56.33 ± 2.42 | 54.33 ± 1.96 | <0.001 |
| 16 wks | 69.68 ± 2.53 | 68.43 ± 3.00 | 0.011 |
| 6 months | 82.09 ± 2.25 | 81.25 ± 3.09 | 0.079 |
| Final Follow up | 77.75 ± 2.42 | 76.79 ± 3.10 | 0.052 |
| TAL | Mean ± SD | Mean ± SD | P-value |
| Pre op | 1.04 ± 0.58 | 1.05 ± 0.58 | 0.978 |
| 6 wks | 1.43 ± 0.61 | 1.25 ± 0.44 | 0.058 |
| 16 wks | 3.66 ± 0.48 | 3.45 ± 0.50 | 0.016 |
| 6 months | 4.38 ± 0.60 | 4.23 ± 0.56 | 0.144 |
| Final Follow up | 4.07 ± 0.76 | 3.94 ± 0.75 | 0.304 |
Table 2. IKDC, KOOS AND TAL scores.
Mechanical stability
There is a significant difference between these two groups in the clinically assessable instability at the 6 months. The reconstructed group showed a positive pivot shift in 29.5% of the cases (7.4% grade 2 and 22.1% grade 1), and positive Lachman test in 29.4% (10.3% grade 1A and 19.1% grade 2A) cases. The non-operative patients showed positive Pivot shift (59.4% grade 1 and 40.6% grade 2) and positive Lachman test (54.7% grade 1B and 45.3% grade 2B). At final follow-up the reconstructed group showed a positive pivot shift in 29.4% of the cases (10.3% grade 2 and 19.1% grade 1), and positive Lachman test in 29.4% (7.4% grade 1A and 22.1% grade 2A) cases. The non-operative group patients showed positive Pivot shift (54.7% grade 1 and 45.3% grade 2) and positive Lachman test (46.9% grade 1B and 53.1% grade 2B). Although in term of instability surgically treated group was found better but functionally (measured by TAL) there was no difference between two groups in our study.
In Group A - mean time to return to job after surgery was 86 days (56-126) whereas in Group B it was 14 days (10-28 days).
Complications
Group A - Anterior knee pain in 4 patients, hardware prominence in 5 patients and superficial infection in 1patient while in group B haemarthrosis was noted in 4 patients and urinary retention in 3 patients (Table 3).
| Complications | Group A | Group B | P-value | ||
|---|---|---|---|---|---|
| Frequency | % | Frequency | % | ||
| None | 60 | 88.2% | 57 | 89.1% | 0.881 |
| Anterior knee pain | 4 | 5.9% | 0 | 0.0% | 0.120 |
| Haemarthrosis | 0 | 0.0% | 4 | 6.3% | 0.053 |
| Hardware prominence | 3 | 4.4% | 0 | 0.0% | 0.245 |
| Superficial infection | 1 | 1.5% | 0 | 0.0% | 1.000 |
| Urinary retention | 0 | 0.0% | 3 | 4.7% | 0.111 |
| Total | 68 | 100% | 64 | 100% | ------- |
Table 3. Complications.
Discussion
An ACL rupture is a very common musculoskeletal injury. The number ACL reconstructions are increasing globally. It is predominantly a sporting injury often resulting in knee instability. Substantial progress has been made with improving surgical technique from an open procedure to a minimal invasive arthroscopic operation. Treatment should always be tailored to each individual. There is insufficient long-term evidence to merit one specific treatment (operative or conservative) above the other. Multiple factors should be considered such as: complaints, amount of instability, sport wishes, age and willingness to commit to a six-month rehabilitation program. An ACL reconstruction will not diminish the increased chance for secondary knee osteoarthritis, neither will it restore normal knee kinematics, but it will reduce giving way complaints. These giving way complaints are still the most important indication for this operation [15].
What we do know is that the number of ACL reconstructions is increasing among non-athletes nowadays but actual incidence is not known. Our study of non-athletes who were either treated with ACL reconstruction (using hamstring graft) or were treated conservatively (optional arthroscopic debridement) showed similar clinical outcome for both groups.
This study was performed to give more insight in the outcome after ACL injury for non-athletes. Both the groups were comparable in terms of age, sex and activity level. The study showed that the operated group performed better at 10 weeks and 16 weeks post-op follow-up (IKDC, KOOS and TAL were statistically significant) but at final post-op follow-up both the groups were found equal (IKDC, KOOS and TAL were statistically insignificant). These results are comparable to previous results from other research done for either conservatively treated or reconstructed ACL injuries [8,16-20].
At final follow-up the reconstructed group showed a positive pivot shift in 29.4% of the cases (10.3% grade 2 and 19.1% grade 1), and positive Lachman test in 29.4% (7.4% grade 1A and 22.1% grade 2A) cases. The non-operative group patients showed positive Pivot shift (54.7% grade 1 and 45.3% grade 2) and positive Lachman test (46.9% grade 1B and 53.1% grade 2B) signifies the severity of instability of this group however, the degree of instability decreased with time, these results are compatible with other results of present day ACL reconstruction or conservative treatment [21,22]. Although instability as tested by positive Pivot and Lachman tests was significantly higher in nonoperative group as compared to operative group but functionally there was no difference between two groups (measured by TAL) in our study. In group A four patients had anterior knee pain which was relieved by physiotherapy and oral analgesics, one case was noted with superficial infection which healed with antibiotics, three patients reported hardware prominence (at tibial post) and required removal of tibial post implant at 6 months post-op. There were four cases of haemarthrosis and three cases of urinary retention in group B these were relieved by symptomatic treatment. Some other complications also reported in literature like infection, bacterial arthritis of the knee, embolus of the popliteal artery, a fatal pulmonary embolism, patella fracture and localized pain [23-27]. None of these complications were seen in our study (Table 4).
| Pivot shift | Group A | Group B | P-value | |||
|---|---|---|---|---|---|---|
| Frequency | % | Frequency | % | |||
| Pre-op | Grade 2 | 58 | 85.3% | 50 | 78.1% | 0.286 |
| Grade 3 | 10 | 14.7% | 14 | 21.9% | ||
| Post-operative 6 weeks | Grade 1 | 0 | 0.0% | 10 | 15.6% | <0.001 |
| Grade 2 | 0 | 0.0% | 54 | 84.4% | ||
| Negative | 68 | 100.0% | 0 | 0.0% | ||
| Post-operative 16 weeks | Grade 1 | 0 | 0.0% | 54 | 84.4% | <0.001 |
| Grade 2 | 0 | 0.0% | 10 | 15.6% | ||
| Negative | 68 | 100.0% | 0 | 0.0% | ||
| Post-operative 6 months | Grade 1 | 15 | 22.1% | 38 | 59.4% | <0.001 |
| Grade 2 | 5 | 7.4% | 26 | 40.6% | ||
| Negative | 48 | 70.6% | 0 | 0.0% | ||
| Final follow up | Grade 1 | 13 | 19.1% | 35 | 54.7% | <0.001 |
| Grade 2 | 7 | 10.3% | 29 | 45.3% | ||
| Negative | 48 | 70.6% | 0 | 0.0% | ||
| Lachman test | ||||||
| Pre-op | Grade 2B | 52 | 76.5% | 48 | 75.0% | 0.844 |
| Grade 3B | 16 | 23.5% | 16 | 25.0% | ||
| Post-operative 6 weeks | Grade 1B | 0 | 0.0% | 10 | 15.6% | <0.001 |
| Grade 2B | 0 | 0.0% | 54 | 84.4% | ||
| Negative | 68 | 100.0% | 0 | 0.0% | ||
| Post-operative 16 weeks | Grade 1A | 0 | 0.0% | 8 | 12.5% | <0.001 |
| Grade 1B | 0 | 0.0% | 47 | 73.4% | ||
| Grade 2B | 0 | 0.0% | 9 | 14.1% | ||
| Negative | 68 | 100.0% | 0 | 0.0% | ||
| Post-operative 6 months | Grade 1A | 7 | 10.3% | 0 | 0.0% | <0.001 |
| Grade 1B | 0 | 0.0% | 35 | 54.7% | ||
| Grade 2A | 13 | 19.1% | 0 | 0.0% | ||
| Grade 2 B | 0 | 0.0% | 29 | 45.3% | ||
| Negative | 48 | 70.6% | 0 | 0.0% | ||
| Final Follow up | Grade 1A | 5 | 7.4% | 0 | 0.0% | <0.001 |
| Grade 1B | 0 | 0.0% | 30 | 46.9% | ||
| Grade 2A | 15 | 22.1% | 0 | 0.0% | ||
| Grade 2 B | 0 | 0.0% | 34 | 53.1% | ||
| Negative | 48 | 70.6% | 0 | 0.0% | ||
Table 4. Assessment of Laxity (Pivot Shift and Lachman Test).
A new secondary ACL rupture in patients after an ACL reconstruction occurs in 6% of the patients in the first 5 years, this can occur in the reconstructed but also in the contra lateral knee. The sport intensity is the most important predictor of the (re) rupturing risk, specifically for the first year. Another consequence of an ACL rupture is a high probability of further damage to the knee. The risk for knee osteoarthritis within 10 to 15 years after the initial trauma is tenfold [23]. No such complication was seen in our study. In our study sample size was small so results may be differed in long term follow and in large sample size.
The aim of each individual knee instability treatment is to restore as much as possible the homeostasis of the joint. This will enable each patient to undertake the activities that were previously possible without an increased risk for comorbidity. At present it is still not fully clear which individual will benefit most with operative or conservative treatment. This study shows that an ACL reconstruction is a good operation to stabilize the knee. This study also shows that a conservatively treated ACL tear gives these patients the same feeling and functional result as ACL reconstructed knee.
Strengths
The strengths of this study are 1) This study was randomized controlled prospective study 2) Patients were treated by a single surgeon at a single center, means that there was consistency in surgical technique and implant used 3) The study included nonathletes and no confounding variable seen in our study as baseline variables were comparable and other variables such as Meniscal tear grade III on MRI, TAL 6 or more than 6 were excluded from the study and 4) Concept of care management model used in our study which improves results.
Limitations
The limitation of our study is that our study had small sample size so results may be differ in a large size sample.
Conclusion
This study revealed both the conservatively treated and the operated group, performed similarly, except for a higher objectively measurable instability for the conservative group. However, they are just as satisfied with their knee without an operation at final follow-up, showing no difference in activity level and functional outcome subjectively. Therefore, conservative treatment should still be considered a treatment option for an ACL insufficient knee in non-athletes.
Recommendations
1. The physical needs of non-athletes are different from athletes, so non-athletes with complete rupture of ACL, there is no need of primary ACL reconstruction.
2. If these patients are symptomatic (history of locking and severe pain) and there is associated meniscus/ other ligament injury/ cartilage lesion seen in MRI than go for arthroscopic debridement + meniscectomy.
3. Put asymptomatic patients on rehabilitation protocol only, no need of arthroscopy in these patients.
4. Delayed reconstruction of ACL may be done in patients who are not happy with outcome of conservative treatment.
Role of care managers is very important they can assist the patients for adherence to rehab protocol on daily basis and can help to improve the results.
REFERENCES
- Spindler K.P., Warren T.A., Callison J.C., et al.: Clinical outcome at a minimum of five years after reconstruction of the anterior cruciate ligament. J Bone Joint Surg Am. 2005;87:1673-1679.
- Spindler K.P., Wright R.W.: Anterior cruciate ligament tear. N Engl J Med. 2008;359:2135-2142.
- Lohmander L.S., Englund P.M., Dahl L.D., et al.: The long –term consequence of anterior cruciate ligament and meniscus injuries: Osteoarthritis. Am J Sports Med. 2007;35:1756-1769.
- Fithian D.C., Paxton E.W., Stone M.L., et al.: Prospective trial of a treatment algorithm for the management of the anterior cruciate ligament-injured knee. Am J Sports Med. 2005;33:335-346.
- Clancy W.G., Ray J.M., Zoltan D.J.: Acute tears of the anterior cruciate ligament. Surgical versus conservative treatment. J Bone Joint Surg Am. 1988;70:1483-1488.
- Sandberg R., Balkfors B., Nilsson B., et al.: Operative versus nonoperative treatment of recent injuries to the ligaments of the knee. A prospective randomized study. J Bone Joint Surg Am. 1987;69:1120-1126.
- Frobell R.B., Lohmander L.S., Roos E.M.: Anterior cruciate ligament injury of the knee into a randomized clinical trial comparing surgical and non-surgical treatment. Contemp Clin Trials. 2007;28:295-302.
- Buss D.D., Min R., Skyhar M., et al.: Non-operative treatment of acute anterior cruciate ligament injuries in a selected group of patients. Am J Sports Med. 1995;23:160-165.
- Roos E.M., Roos H.P., Ekdahl C., et al.: Knee injury and Osteoarthritis Outcome Score (KOOS)-validation of a Swedish version. Scand J Med Sci Sports. 1998;8:439-448.
- Irrgang J.J., Ho H., Harner C.D., et al.: Use of the International Knee Documentation Committee guidelines to assess outcome following anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 1998;6:107-114.
- Tegner Y., Lysholm J.: Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res. 1985;198:43-49.
- Phillips B.B., Milhalko M.J.: Arthroscopy of lower extremity. Canale ST, Beaty JH, editors. Campbell’s operative orthopaedics, 12th edition: Mosby Elsevier. 2013;51:2433.
- Beard D.J., Dodd C.A.: Home or supervised rehabilitation following - Anterior cruciate ligament reconstruction: A randomized controlled trial. J Ortho & Phys Ther Sports. 1998;27:134-143.
- Ciccone M.M., Aquilino A., Cortese F., et al.: Feasibility and effectiveness of disease and care management model in the primary health care system for patients with heart failure and diabetes (Project Leonardo). Vasc Health Risk Manag. 2010;6:297-305.
- Pinczewski L.A., Lyman J., Salmon L.J., et al.: A 10-year comparison of anterior cruciate ligament reconstructions with hamstring tendon and patellar tendon auto-graft: A controlled, prospective trial. Am J Sports Med. 2007:564-574.
- Meuffels D.E., Favejee M.M., Vissers M.M., et al.: Ten year follow-up study conservative versus operative treatment of anterior cruciate ligament ruptures. A matched – pair analysis of high level athletes. Br J Sports Med. 2009;43:347-351.
- Daniel D.M., Stone M.L., Dobson B.E., et al.: Fate of the ACL-injured patient. A prospective outcome study. Am J Sports Med. 1994; 22: 632-644.
- Casteleyn P.P., Handelberg F.: Non-operative management of anterior cruciate ligament injuries in the general population. J Bone Joint Surg Br. 1996;78:446-451.
- Maletius W., Messner K.: Eighteen- to twenty-four-year follow-up after complete rupture of the anterior cruciate ligament. Am J Sports Med. 1999;27:711-717.
- Nebelung W., Wuschech H.: Thirty-five years of follow-up of anterior cruciate ligament-deficient knees in high-level athletes. Arthroscopy. 2005;21:696-702.
- Ait Si Selmi T., Fithian D., Neyret P.: The evolution of osteoarthritis in 103 patients with ACL reconstruction at 17 years follow-up. Knee. 2006;13:353-358.
- Strand T., Molster A., Hordvik M., et al.: Long-term follow-up after primary repair of the anterior cruciate ligament: clinical and radiological evaluation 15-23 years postoperatively. Arch Orthop Trauma Surg. 2005;125:217-221.
- Van Tongel A., Stuyck J., Bellemans J., et al.: Septic arthritis after arthroscopic anterior cruciate ligament reconstruction: a retrospective analysis of incidence, management and outcome. Am J Sports Med. 2007;35:1059-1063.
- Allum R.: Complications of arthroscopic reconstruction of the anterior cruciate ligament. J Bone Joint Surg Br. 2003;85:12-16.
- Janssen R.P., Sala H.A.: Embolism of the popliteal artery after anterior cruciate ligament reconstruction: A case report and literature review. Knee Surg Sports Traumatol Arthrosc. 2007;15:1449-1451.
- Janssen R.P., Sala H.A.: Fatal pulmonary embolism after anterior cruciate ligament reconstruction. Am J Sports Med. 2007;35:1000-1002.
- Salmon L., Russell V., Musgrove T., et al.: Incidence and risk factors for graft rupture and contralateral rupture after anterior cruciate ligament reconstruction. Arthroscopy. 2005;21:948-957.



 Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.
Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.