Comparative study of posterolateral fusion versus combination of posterolateral and posterior lumbar interbody fusion in spondylolisthesis treated with posterior decompression and pedicle screw fixation
2 Department of Orthopedics, Birrd Hospital, Tirupati , Andhra Pradesh, India
3 Department of Orthopedics, Bawa Hospital, India
4 Department of Medicne, SRGD Amritsar, India, Email: Ejasminekaur8621@yahoo.com
Received: 01-Jul-2021 Accepted Date: Jul 16, 2021 ; Published: 23-Jul-2021, DOI: 10.37532/1897-2276.2021.16(1).27
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: Spondylolisthesis is defi ned as forward slippage of cephalad vertabra on a caudal vertebra. It is a combination of 2 greek words-Spondylos (Vertebra) and Olisthanein (to slip or fall). Spondylolysis is the most common cause of low back pain in adolescents and about 15% to 25% of patients of spondylolysis will ultimately develop spondylolisthesis.
Methods: The study was conducted to compare the Clinical and the Functional outcome of Posterolateral fusion versus combination of Posterolateral and Posterior lumbar interbody fusion in spondylolisthesis treated with posterior decompression and pedicular screw fi xation performed between March 2015 and March 2016,fi rst 13 patients consecutive patients underwent Posterolateral Fusion (PLF) while last 13 patients underwent combination of posterolateral fusion and Posterior Lumbar Interbody Fusion (PLIF). The clinical outcome was evaluated according to the Visual Analogue Scale (VAS) and functional outcome was evaluated according to Oswestry Disability Index (ODI).
Results: Maximum patients were in age group of 51-60 years in both groups with mean age of presentation being 47.3 years. Low backache was the most common symptom being present in 100% of patients. Radicular pain and claudication were the next most common symptoms.
This study shows that in group 2 where patients were treated with combination of PLIF and PLF 76.9% of patients had Grade 2 fusion while only 38.5% of patients in group 1 had Grade 2 fusion (p=0.025). ODI and VAS also improved more in group 2 and this diff erence was statistically signifi cant (p<.001).
Conclusion: Combination of posterolateral and posterior lumbar interbody provides good clinical,functional and radiological outcome with less complications as compared PLF alone.
Keywords
Spondylolisthesis; Posterolateral Fusion; Pedicle Screw Fixation; VAS; ODI; fusion rate; interbody fusion; spondylosis; Meyerding ; body slippage
Introduction
The term Spondylolisthesis comes from combination of two greek words-Spondylos (Vertebra) and Olisthanein (to slip or fall) [1].
Spondylolysis is the most common cause of backache in adults [2-4]. Th e incidence of spondylolisthesis in the general adult population is 4% to 8%, depending upon the race, age, and sex of the population. Approximately 8% to 14% of adolescent athletes’ suff ere from spondylolysis .In general, women are at greater risk than men [5]. Lower back pain, sciatica, paraesthesia, weakness and intermittent claudication are the main symptoms.
Spondylolisthesis can manifest anywhere in the spine with the lumbosacral region being most commonly aff ected. L5 region is involved in with almost 70% to 95% cases.
Treatment of spondylolisthesis depends on the severity of symptoms which the patients have. Most patients who present with spondylolisthesis are asymptomatic or have minor symptoms like pain [6]. Conservative measures include no steroidal medications, selective nerve/pars injections; brace therapy, restriction of athletic activities, and bed rest. If patients fail to respond to 3-6 months of non-surgical treatment, surgical intervention is considered [7].
Many surgical techniques are available including Posterolateral Fusion (PLF), posterior lumbar interbody fusion (PLIF), Transforaminal Lumbar Interbody Fusion (TLIF), Anterior Lumbar Interbody Fusion (ALIF) with or without posterior instrumentation. Th e simplest surgical procedure is to do arthrodesis without instrumentation, but this has been found to be associated with a high rate of non-union. Addition of pedicle screw to the above provides stability to the spine and improves the fusion rate.
Patients and Methods
Th is is a prospective study of 26 cases (13 in each group) operated between March 2015 to March 2016 conducted in Balaji Institute of Surgery,Research and Rehabilitation for the Disabled to Compare posterolateral fusion versus combination of posterolateral and posterior lumbar interbody fusion in Spondylolisthesis treated with Posterior Decompression and Pedicle screw fi xation. Informed consent was taken from the patients and ethical committee approval was taken.
Patients diagnosed with spondylolysis and spondylolisthesis with failed conservative treatment between age group of 30-70 years of both sexes were included in this study. Patients with Meyerding Grade-V spondylolisthesis and those who did not have a regular follow up for a minimum period of 3 months were excluded. A total of 26 consecutive patients were taken which divided into 2 groups:
• Group 1: Underwent Posterolateral fusion.
• Group 2: Underwent the Combination of Posterolateral and Posterior lumbar interbody fusion.
Preoperative investigations included hemoglobin, blood grouping, others tests depending on co-morbidity and to rule out infection total leucocyte count, diff erential count, Erythrocyte Sedimentation Rate (ESR), C Reactive Protein (CRP) were done. Radiographic evaluation consists of standard anteroposterior, lateral, oblique, fl exion and extension views were taken in standing position. An MRI scan of lumbosacral spine was also done to determine the extent of the nerve root involvement.
Th e percentage of vertebral body slippage was measured by Meyerding classifi cation [8].
• Grade I - 0-25 %
• Grade II - 25-50 %
• Grade III - 50 -75 %
• Grade IV - 75-100 %
• Grade V - 100 % - Spondyloptosis
Clinical outcome was determined on the basis of Visual Analogue Score (VAS) [9]. Functional outcome was calculated on the basis of Oswestry Disability Index (ODI) [10]. Radiological outcome was determined by Radiological fusion scale [11]. Improvement in symptoms including low backache, radicular pain, Claudication, sphincter disturbance, numbness and weakness were assessed at each follow up. Fusion was then assessed by plain lumbar spine radiographs at 6 weeks, 3 months, 6 months and 12 months aft er operation.
Operative Procedure
Aft er the administration of general anaesthesia, the patient was placed on Spinal frame in prone position (this decreases intra-abdominal pressure resulting in decreased venous pressure and bleeding in the epidural plexus) on the operating table, with hips in as much neutral as possible (an attempt to reduce the listhesis) and knees in fl exion (to prevent undue stretching of nerve roots). Proper padding of the pressure points was done.
A standard posterior midline incision was made and the paraspinal musculature detached subperiosteally and freed to the outer margins of the transverse processes on either sides. Haemostasis was achieved by means of bipolar electro cauterization and packing. Care was taken to identify and cauterize the dorsal branches of lumbar arteries. Decompression by laminectomy and facetectomy was done. Each nerve root was followed out past its nerve root canal to ensure adequate decompression and release of the adhesions, scar tissue or any other bony or soft tissue impingements. Osteophytes, previous fusion masses from pseudoarthrosis, if present were removed.
Entry point
At the junction of the lateral to facet and the transverse processes or intersection of the vertical line through the facet joints and a horizontal line through the transverse process. Th e facet joints of the involved segments were identifi ed and the joint surfaces excised. A posterior decortication was performed at this stage. K-wires were put through the entry point and exact placement was confi rmed under fl uoroscopic guidance. Pedicle screws were inserted under fl uoroscopic control, using a standard “free hand targeting” technique. Decompression was commenced via the midline, removing adjacent borders of the spinous processes of the vertebrae above and below. Interspinous ligaments and ligamentumfl ava were excised to enter the neural canal. Th e spinal fenestration was enlarged with suffi cient decompressivelaminotomy superiorly and inferiorly to expose and mobilise the nerve roots on both sides. Th ese were then retracted to expose the disc space. A cruciate incision was made on both sides of the annulus and the disc material was removed with pituitary rongeurs. Two longitudinal rods were bent to maintain the lumbar lordosis and were put in the head of pedicle screws, and the construct was tightened and distraced to achieve the normal disc height and vertebral alignment. In group 1, the removed spinous process and laminectomy bone chips was taken as graft and was put in between the transverse processes along with tricalcium phosphate granules.
In group 2, Th e spinous process and laminectomy bone chips and tricalcium phosphate granules was taken as graft and was put in between the transverse processes and intervertebral disc space [12-14]. Free fat graft was put over exposed dura mater to prevent postoperative adhesions. Closure was done in layers over a sub fascial suction drain in both groups.
Results
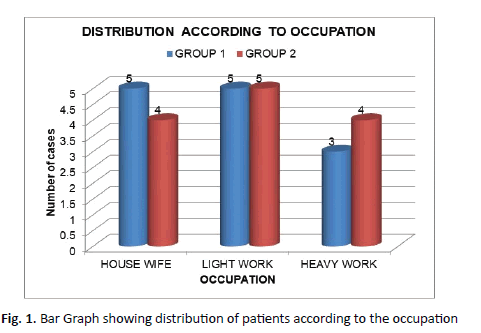
Th e age of presentation ranged from 31 years to 65 years. Maximum patients were in age group of 51-60 years in both groups with mean age of presentation being 47.3 years. 20 out of 26 (76.9%) patients were females with 11 females in group 1 and 9 females in group 2. (38.4%) out of the 26 patients were light workers whereas 7 (26.9%) were heavy workers. Maximum no. of patients 5 (38.4%) in both groups were light workers.
All patients included in this study were symptomatic. Low backache was the most common symptom being present in 100% of patients. Radicular pain and claudication were the next most common symptoms. None of our patient had sphincter disturbances in form of bowel and bladder involvement. 6 patients in each group had neurological defi cit in form of numbness and weakness of lower limbs.
On examination, 21 (80.8%) of patients were having no motor defi cit. 4 (15.4%) patients were having grade 4 power in EHL either on one side or both sides. 17 (65.3%) patients were having no sensory loss. 9 (34.6%) out of the 26 patients were having either unilateral or bilateral L5 radiculopathy .
Th e commonest level involved was L4-L5 in 13 patients (50%) followed by L5-S1 level (12 cases, 46.2 %) and L3-L4 level (1 case, 3.8%).
In group 1 in which posterolateral fusion of vertebra was done, pre operatively 4 (30.8%) patients had Meyerding Grade 1, 8 (61.5%) had Grade 2, whereas 1 (3.4%) patient had Grade 3 vertebral body slippage. In combination of posterolateral and posterior lumbar interbody fusion, pre operatively 6 (46.2%) patients were having Grade 1, 4 (30.8%) was in Grade 2, 2 (7.7%) were having grade 3 whereas 1 (3.4%) patient was having Grade 4 slippage according to Meyerding classifi cation.
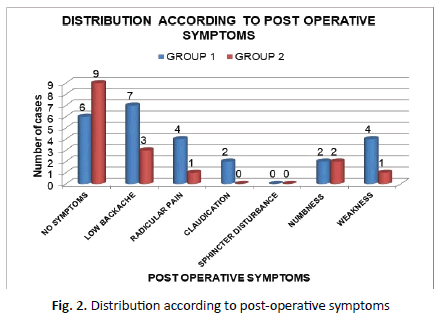
Post operatively, symptoms improved in all patients. 6(46.1%) patients were asymptomatic aft er surgery. Only 6 patients were left with low backache and only 4 patients had radicular pain which was low intensity as compared to pre-operative pain. In combination of posterolateral and posterior lumbar interbody fusion, there was signifi cant reduction in pain. Only 2 (7.7%) of patients were left with pain aft er surgery and 50% of patients had no numbness or weakness aft er surgery.
10 (76.9%) of patients in group 2 had Grade 2 fusion while only 5 (38.5%) of patients in group 1 had Grade 2 fusion. In group 1, 11 (84.6%) patients had grade 0 or 1 while only 2 patients (15.4%) had grade 2 or 3 post operatively. In group 2, 10 patients (76.9%) had grade 0 or 1 fusion. (Tables 1-3)
| AGE GROUP (YEARS) | GROUP 1 | GROUP 2 | TOTAL |
|---|---|---|---|
| 31-40 | 4 (30.7%) | 3 (23.1%) | 7 (26.9%) |
| 41-50 | 3 (23.1%) | 4 (30.7%) | 7(26.9%) |
| 51-60 | 5 (38.4%) | 6 (46.1%) | 11 (42.3%) |
| 61-70 | 1(7.7%) | 0 | 1 (3.4%) |
| TOTAL | 13 | 13 | 26 (100%) |
Table 1. Table showing distribution of patients according to age group
| SYMPTOMS | GROUP 1 | GROUP 2 |
|---|---|---|
| NO SYMPTOMS | 0 | 0 |
| LOW BACKACHE | 13 (100%) | 13 (100%) |
| RADICULAR PAIN | 11 (84.6%) | 13 (100%) |
| CLAUDICATION | 11 (84.6%) | 7 (53.8%) |
| SPHINCTER DISTURBANCE | 0 | 0 |
| NUMBNESS | 2 (15.4%) | 4 (30.7%) |
| WEAKNESS | 3(23.1%) | 3(23.1%) |
Table 2. Showing distribution according to pre-operative symptoms
|
NO OF CASES |
PLF |
PLF+PLIF |
FUSION RATE FOR PLIF+ PLF |
|---|---|---|---|---|
Rosa GL et al [22] |
35 |
0.667 |
0.765 |
0.95 |
William Abdu et al [23] |
380 |
0.6724 |
0.8567 |
0.875 |
Our Study |
26 |
0.615 |
0.846 |
0.923 |
Table 3. Comparison of our study with previous studies in terms of good functional outcome and fusion rates
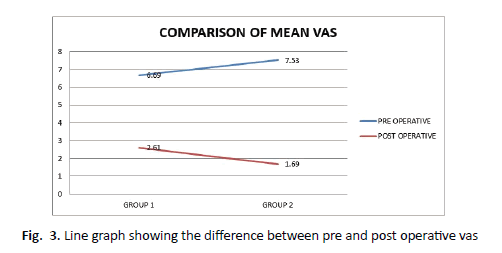
Visual Analogue Scale (VAS) was used to quantify the amount of pain patient was having. VAS diff erence which was calculated by subtracting pre and post-operative VAS, it was more in group 2 than group 1 and this diff erence was highly signifi cant (p=0.008)
Clinical outcome was defi ned according to diff erence between pre and post-operative VAS. Th e diff erence was divided into 3 categories which were as following:
If the diff erence was 0-2 then outcome was poor.
If the diff erence was 3-5 then outcome was fair.
If the diff erence was >5 then outcome was good.
According to this classifi cation, 7 (53.8%) patients each had a good outcome in group 1 while in group 2, 11 (84.6%) patients had good outcome (p=0.180).
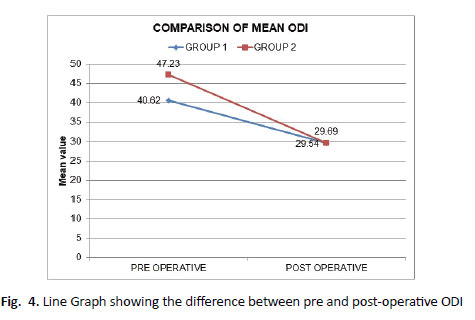
Oswestry Disability Index (ODI) is a clinical assessment of low back pain. It includes ten categories: pain intensity, personal care, lift ing, walking, sitting, standing, sleeping, sex life, social life and travelling. Each category is assigned 5 points. Th e post-operative ODI improved in both groups but it was more in group 2 and it was highly signifi cant (p<0.001).
Th e functional outcome was decided according to diff erence in pre and post-operative ODI. Th e diff erence of ODI was then divided into 3 categories for predicting the functional outcome which was as following:
If diff erence was <6%, the outcome was poor.
If diff erence was 6-12%, the outcome was fair.
If diff erence was >12%, the outcome was good.
12 (92.3%) had good functional outcome in group 2 while 69.2% had good functional outcome in group 1.
22(84.6%) had no complications during and post-surgery. 1(7.7%) patient had dural tear while 2(15.3%) patients had screws broken in group 1, while only 1 (7.7%) patient had infection in group 2.
Discussion
In our study, the youngest patient was 31 years old and eldest patient was 65 years. Mean age of patients was 47.3 years. 20 patients were female (76.9%) and 6 were male (23.1%). Two males and 11 females comprised Group I (PLF). In Group II (PLF+PLIF) there were 9 females and 4 males indicating female preponderance in this condition (F:M- 2:1). Similar results have been obtained in the previous studies. Th is can be due to the reason that most operated had degenerative lumbar spine and the osteoporosis is one of the defi nitive signs of degeneration. In Indian scenario, osteoporosis is a highly prevalent in females and the progression of spine degeneration is more severe and earlier in females [15,16].
Th e various signs and symptoms were present for months to years with 50% of patients were having these symptoms for less than 6 months, 9 (34.6%) had symptoms for more than six months whereas 4 (15.4%) of patients had complaints lasting for more than one year.
In our study 13 patients underwent PLF with PLIF and there was signifi cant reduction in pain. Only 2 (7.7%) out of the 13 patients were left with pain aft er surgery and 50% of patients had no numbness or weakness aft er surgery.
In group 2, no patient had poor outcome. 2 patients had fair outcome whereas 11 patients had good outcome based upon ODI score. Salah Fallatah et al. in 2013 showed a slight but not signifi cant trend toward a better functional outcome in the Posterior interbody fusion group [17].
Post operatively grading was done aft er 6 months. 3 (23.1%) and 6 (46.2%) patients were having Grade 0 in xray in group 1 and 2 respectively. In group 1, 8 (61.5%) had grade 1 while 1 (7.7%) patient each had grade 2 and 3. In group 2, 4 (30.8%) and 3 (23.1%) had grade 1 and 2 respectively. None of the patient had grade 4 postoperatively.
Th e fusion grade was studied on x-ray done aft er 6 months. In group 1, 3 patients did not have fusion whereas 5 (38.5%) patients each had grade 1 and grade 2 fusion. In group 2, 10 (76.9%) had grade 2 fusion, 2 (15.4%) had grade 3 fusion, 1 (7.7%) patient had grade 1 fusion. Th is showed that fusion rates were more in group 2 as compared to group 1. Similarly Zhou ZJ et al. in 2011 and Yong-Ping Ye et al in 2013 showed that fusion rate was signifi cantly higher in the PLIF-treated group than that in PLF treated group [18].
Th e overall fusion rates in two groups was 10 (76.9%) and 13 (100%) respectively in the two groups. Emile Dehoux et al in year 2004 also showed that the fusion rate was 68% with PLF and 93% with PLIF [19].
Th e intra and post-operative complications were more in group 1. 1 (7.7%) patient had dural tear while 2 patients had screws broken while only 1 (7.7%) patient had infection in group 2. Th is was in concordance with the studies done in past. Lei Cheng in year 2008 showed that the PLIF group had better fusion and fewer complications as compared to PLF group [20]. Similarly, Fernando Luiz Rolemberg Dantas et al. in the year 1999-2001 showed that both surgical procedures were eff ective. The PLIF with pedicle screws group presented better clinical outcomes. Group I presented more complications when compared with Group II [21].
In conclusion, Posterior Lumbar Interbody Fusion (PLIF) is an eff ective method in the treatment of spondylolisthesis, as it provided good spinal fusion, less complication with satisfactory clinical outcome [23].
Periasamy et al. [24] conducted a retrospective study on 75 patients who underwent PLF plus PLIF. Good Clinical outcome was achieved in 85.3% of cases. (Figures 1-4)
Th us, combination of Posterolateral (PLF) and Posterior Lumbar Interbody Fusion (PLIF) is an eff ective method in the treatment of spondylolisthesis, as it provided good spinal fusion, less complications and gives a satisfactory clinical, functional and radiological outcome.
Conclusion
Overall it was concluded that combination of both posterolateral and posterior lumbar interbody fusion technique gives a 360 degree fusion and have apparent mechanical and surgical advantages and gives a good clinical, functional and radiological outcome.
With proper placement of pedicle screws and pre-countouring of connecting rods lumbar lordosis is restored, disc space height is maintained and spondylolisthesis is reduced. In combination of posterolateral and posterior lumbar interbody fusion we used the removed spinous process and laminectomy bone chips as graft for fusion. We did not use iliac bone as bone graft , so donor site morbidity at iliac crest was prevented. We used lamina as interbody graft and did not use interbody cages which lead to a cost eff ective study.
Posterior decompression of the spinal canal combined with anterior and posterior arthrodesis performed at one stage through a posterior approach is a safe and eff ective technique in managing spondylolisthesis.
In spondylolisthesis, forward displacement of the vertebra is determined on the lateral view. Meyerding devised a simple method to grade the listhesis according to the percentage of slippage. The anteroposterior diameter of the subjacent vertebral body is divided into four equal parts. A slip in the fi rst quarter of this vertebral body is grade I; one in the last quarter is grade IV.
REFERENCES
- Canale ST, Beaty JH. Campbell’s Operative Orthopaedics. 11th ed.Mosby Elsevier publishers.2008; Vol.2, part XII: 1729 – 2273.
- Fredrickson BE,Baker D, McHolick WJ. The natural history of spondylolisis and spondylolisthesis. J Bone Joint Surg Am.1984; 66:699–707.
- Frymoyer JW. Back pain and sciatica.N Engl J Med.1988; 318:291–300.
- Frymoyer JW,Selby DK. Segmental instability. Rationale for treatment. Spine.1985; 10:280–6.
- Rosenberg NJ.Degenerative spondylolisthesis: Predisposingfactors. J Bone Joint Surg Am.1975; 57: 467-74.
- Vakenberg HA, Haanen HCM.The epidemiology of low backpain, in White AA III, Gordon SL (eds): American Academy of Orthopaedic Surgeons Symposium on Idiopathic Low Back Pain.St Louis: CV Mosby. 1982: 9-22.
- Jones TR,Rao RD. Adult isthmic spondylolisthesis.J Am Acad Ort hop Surg. 2009; 17:609-17.
- Meyerding HW. Spondylolisthesis.Surg Gynecol Obstet. 1932; 54:371
- Guyatt GH,Townsend M,Berman LB,Keller JL.A comparison of Likert and visual analogue scales for measuring change in function.J Chronic Dis.1987;40:1129-33.
- Fairbank JC,Couper J,Davies JB,O’Brien JP.The Oswestry low back disability questionnaire.Physiotherapy. 1980;66:271-3.
- Kant AP,Daum WJ,Dean SM,Uchida T. Evaluation of lumbar spine fusion.Plain radiographs versus direct surgical exploration and observation.Spine .1995;20:2313-7.
- Kho VK, Chen WC. Posterolateral fusion using laminectomy bone chips in the treatment of lumbar spondylolisthesis.InternationalOrthop SICOT.2008;32:115-19.
- Csecsei GI,Klekner AP, Dobai J, Lajgut A,Sikula J. Posterior interbody fusion using laminectomy bone and transpedicular screw fixation in the treatment of lumbar spondylolisthesis. Surg-Neuro. 2000 Jan;53(1):2-6.
- Gupta A ,Chauhan V .Experimental posterolateral spinal fusion with beta tricalcium phosphate ceramic and bone marrow aspirate composite graft. Indian Journal of Orthopaedics. 2010;44: 402-8.
- Yu CH, Wang CT, Chen PQ. Instrumented posterior lumbar interbody fusion in adult spondylolisthesis. Clinical orthopaedics and related research. 2008; 466(12):3034-43.
- Acharya S, Srivastava A, Sen I. Osteoporosis in Indian women aged 40-60 years. Archives of Osteoporosis. 2010; 5(1-2):83-9.
- Fallatah S,Wai E and Christopher SB.The value of adding posterior interbody fusion in the surgical treatment of degenerative lumbar spine disorders: A systematic review International Journal of Spine Surgery .2013;7: 24–8.
- Zhou ZJ, Zhao FD,Fang XQ. Meta-analysis of instrumented posterior interbody fusion versus instrumented posterolateral fusion in the lumbar spine.J.Neurosurg Spine. 2011; 15:295-310.
- Dehoux E, Fourati E, Madi K, Reddy B, Segal P. Posterolateral versus interbody fusion inisthmic spondylolisthesis: functional results in 52 cases with a minimum follow-up of 6 years. Acta Orthop. Belg. 2004 Dec; 70(6):578-82.
- Cheng L, Nie L, Zhang L. Posterior lumbar interbody fusion versus posterolateral fusion in spondylolisthesis: a prospective controlled study in the Han nationality.SICOT.2009;33:1043-47.
- Dantas FLR, Prandini MN, Ferreira MAT .Comparison between posterior lumbar fusion with pedicle screws and posterior lumbar interbody fusion with pedicle screws in adult spondylolisthesis .Arq Neuropsiquiatr. 2007;65(3-B):764-70.
- Rosa GL, Conti A, Cacciola F, Cardali S, Torre DL, Gambadauro NM et al. Pedicle screw fixation for isthmic spondylolisthesis: does posterior lumbar interbody fusion improve outcome over posterolateral fusion? J Neurosurg (Spine 2).2003; 99:1-15.
- Abdu WA,Lurie JD, Spratt KF, Tosteson ANA,Zhao W,Tosteson TD et al. Degenerative SpondylolisthesisDoes Fusion Method Influence Outcome? Four-Year Results of the Spine Patient Outcomes Research Trial.Spine..2009;34(21): 2351–60.
- Kumar P, Shah K, Eugene F, Wheelwright. Posterior lumbar interbody fusion using cages, combined with instrumented posterolateral fusion: A study of 75 cases. ActaOrthop.Belg. 2008; 74:240-8.



 Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.
Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.