Compressive peroneal nerve neuropathy by ganglion cyst in an 11- year old boy, a case report
Received: 03-Dec-2022, Manuscript No. jotsrr-22- 82133; Editor assigned: 04-Dec-2022, Pre QC No. jotsrr-22- 82133 (PQ); Accepted Date: Dec 27, 2022 ; Reviewed: 18-Dec-2022 QC No. jotsrr-22- 82133 (Q); Revised: 25-Dec-2022, Manuscript No. jotsrr-22- 82133 (R); Published: 02-Jan-2023, DOI: .10.37532/1897-2276.2022.17( 12).72
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
The Common Peroneal Nerve (CPN) is the most common compressive neuropathy in the lower limbs. However, CPN compression is a rare entity in the pediatric age group. We report an eleven-year-old child who presented with a right foot drop secondary to a ganglion cyst from the proximal tibiofibular joint and demonstrated recovery three months after nerve decompression.
Keywords
Ganglion cyst, proximal tibio fibular joint, peroneal nerve
Introduction
The Common Peroneal Nerve (CPN) is the most common compressive neuropathy in the lower limbs. Although the most common site of compression is at the fibular neck, the nerve can be compressed through its whole course [1, 2]. Many conditions lead to the compression of CPN, including extrinsic masses and intrinsic nerve sheath tumours, traumatic and iatrogenic causes [3]. However, CPN compression is rare in the pediatric age group [4]. Therefore, we report an elevenyear-old child who presented with a right foot drop secondary to a ganglion cyst from the proximal tibiofibular joint. The child was operated on, the CPN was decompressed, and the histopathological study confirmed the ganglion diagnosis. The child demonstrated recovery at three months.
Case Presentation
An 11-year-old boy developed an abnormal gait with right-sided foot drop and was treated by the family doctor with multiple casting for a one-month duration as supposed to have unwitnessed trauma, although the child denied the history of trauma. Due to a lack of child response on casting, he was referred to our institute for further evaluation. The clinical examination of the child revealed right foot drop and stoppage gait with no local tenderness and a painless full passive range of motion. The lower limb examination revealed flickering of the anterior leg compartment and muscle power grade 1 of the ankle and big toe dorsiflexion with preserved ankle plantarflexion power. Sensory examination revealed diminished sensation over the anterolateral leg and dorsum of the foot. Therefore, the child examination was compatible with CPN palsy (Figure 1).
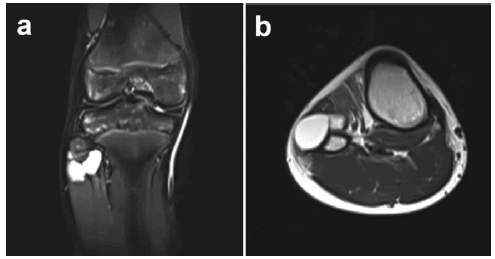
Leg and foot radiographs were negative, while leg MRI revealed a synovial cyst measuring 30mm × 15mm × 30mm arising from the proximal tibiofibular joint and compressing the CPN at the level of the fibular neck, (Figure 2).
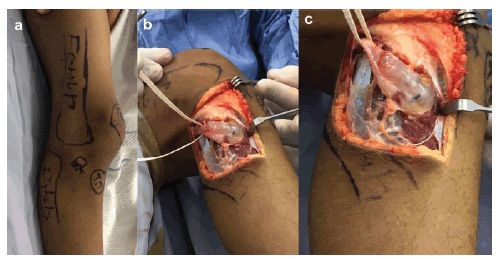
Therefore, a decision to explore and decompress the nerve was taken. The surgery was done in the supine position using a tourniquet through a direct lateral approach. Intraoperative findings showed a mass from the proximal tibiofibular joint compressing on the CPN, presumably a tibiofibular ganglion cyst, (Figure 3).
The mass was excised, the CPN was released, the wound was closed in layers, and a splint was applied for three weeks, followed by ankle orthosis for four weeks to prevent the equinus. Stitches were removed at two weeks, and the histopathologic study confirmed the diagnosis of a ganglion cyst. The child demonstrated progressive improvement over monthly follow-up; at three months, ankle dorsiflexion power was restored (5/5), and the big toe dorsiflexion improved to 3/5.
Discussion
Compressive neuropathy of the CPN is the most common lower-extremity entrapment neuropathy and the third most common after median and ulnar nerve entrapment and accounts for 15% of all peripheral entrapment neuropathies. It tends to be more common in adults and men, with a male-to-female ratio of 2.8:1. However, it is rare in the pediatric age group [4-6].
Compression of the CPN can occur at any location at its course in the thigh and the leg. However, the most common compression site is near the fibular head. Injury and compression of the CPN may occur with traumatic conditions such as fibular neck fracture and fracture and dislocation of the knee. Iatrogenic causes occur around knee osteotomies, especially with correcting severe genu valgum and arthroplasty and limb lengthening procedures. External nerve compression has a wide spectrum of pathology, including improperly fitted cast, interneural and extraneural tumours, bone tumours, and vascular abnormalities. Extraneous exercises and abnormal positions are known causes of compression. However, idiopathic pathology is considered after excluding other causes [7-11].
Compressive CPN neuropathy is usually a slowly progressive condition that develops over a few weeks to months and presents with weakness of ankle and toes dorsiflexion and eversion, resulting in foot drop and gait problems. Sensory disturbances manifested by decreased sensation or pain in the distribution of the CPN. Acute palsy is usually traumatic such as penetrating injuries [12, 13].
Imaging study help in identifying the cause and level of compression. However, a CT scan helps diagnose bony pathology, while ultrasonography and MRI are for soft tissue pathology. Electrodiagnostic studies help localize the site of pathology, determine the severity of compression, and monitor recovery after decompression [14, 15]. Electrodiagnostic studies should be performed for patients with new onset foot drop as a baseline, and the study can be repeated every three months to monitor recovery or deterioration. However, in the case of trauma, neurodiagnostic tests should be delayed till six weeks [16, 17].
Non-operative treatment can be the first line of treatment in CPN compression, especially in conditions caused by positions or activities such as squatting and strenuous exercise. This includes activity modification, rehabilitation therapy, braces, and glucocorticosteroid injection. However, surgery carries faster and better recovery [18, 19]. Uzenot et al. considered surgery without recovery after six months, while Dallari et al. recommended early surgery once the diagnosis compressive peroneal nerve neuropathy by ganglion cyst in an 11- year old boy-A case report
was confirmed [20, 21]. Ismael et al. and Bahri et al. reported better functional recovery with earlier surgery [22, 23].
Conclusion
Common peroneal nerve compressive neuropathy is rare in children and results in foot drop, gait problems, and sensory disturbances. However, non-operative treatment can be the first line of treatment. Nevertheless, early surgery carries better and faster functional recovery. Therefore, decompression is recommended once the diagnosis is confirmed.
References
- Marciniak C. Fibular (peroneal) neuropathy: electrodiagnostic features and clinical correlates. Phys Med Rehabil Clin N Am. 2013;24:121-37. [Google Scholar] [CrossRef]
- Mahan M. Common peroneal entrapment across the fibular head. A Comprehensive Review. Vol. 1. New York: Theime Medical Publishers; 2015:705-8. [Google Scholar] [CrossRef]
- Bowley MP, Doughty CT. Entrapment Neuropathies of the Lower Extremity. Med Clin North Am. 2019 Mar;103(2):371-82. [Google Scholar] [CrossRef]
- Gayet LE, Morand F, et al. Compression of the peroneal nerve by a cyst in a seven-year-old child. Eur J Pediatr Surg. 1998 Feb;8(1):61-3. [Google Scholar] [CrossRef]
- Maalla R, Youssef M, et al. Peroneal nerve entrapment at the fibular head: outcomes of neurolysis. Orthop Traumatol Surg Res. 2013;99:719-22. [Google Scholar] [CrossRef]
- Schuh A, Handschu R, et al. Peroneal nerve entrapment syndrome]. MMW Fortschr Med. 2017 Dec;159(21-22):84-8. [Google Scholar] [CrossRef]
- Anderson JC. Common Fibular Nerve Compression: Anatomy, Symptoms, Clinical Evaluation, and Surgical Decompression. Clin Podiatr Med Surg. 2016 Apr;33(2):283-91. [Google Scholar] [CrossRef]
- Beltran LS, Bencardino J, et al . Entrapment neuropathies III: lower limb. Semin Musculoskelet Radiol. 2010 Nov;14(5):501-11. [Google Scholar] [CrossRef]
- Faktorovich S, Filatov A, Rizvi Z. Common Compression Neuropathies. Clin Geriatr Med. 2021 May;37(2):241-52. [Google Scholar] [CrossRef]
- Zeng X, Xie L, Qiu Z, Sun K. Compression neuropathy of common peroneal nerve caused by a popliteal cyst: A case report. Medicine (Baltimore). 2018 Apr;97(16):e9922. [Google Scholar] [CrossRef]
- Huang Y, Chu X, Zhu Q. Peripheral nerve injury as a complication from orthopedic operation. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 1997 Nov;11(6):343-6. [Google Scholar] [CrossRef]
- Garg B, Poage C. Peroneal Nerve Palsy: Evaluation and Management. J Am Acad Orthop Surg. 2016 May;24(5):e49. [Google Scholar] [CrossRef]
- Craig A. Entrapment neuropathies of the lower extremity. PM R. 2013 May;5(5 Suppl):S31-40. [GoogleScholar] [CrossRef]
- Becciolini M, Pivec C, Riegler G. Ultrasound Imaging of the Deep Peroneal Nerve. J Ultrasound Med. 2021 Apr;40(4):821-38. [Google Scholar] [CrossRef]
- Kim JY, Ihn YK, Kim JS, et al. Non-traumatic peroneal nerve palsy: MRI findings. Clin Radiol. 2007 Jan;62(1):58-64. [Google Scholar] [CrossRef]
- Peters BR, Pripotnev S, Chi D, et al. Complete Foot Drop With Normal Electrodiagnostic Studies: Sunderland "Zero" Ischemic Conduction Block of the Common Peroneal Nerve. Ann Plast Surg. 2022 Apr 1;88(4):425-8. [Google Scholar] [CrossRef]
- Masakado Y, Kawakami M, Suzuki K, et al. Clinical neurophysiology in the diagnosis of peroneal nerve palsy. Keio J Med. 2008 Jun;57(2):84-9. [Google Scholar] [CrossRef]
- Baron D. Prise en charge locale des syndromes canalaires. Rev Rhum 2007;74:424-33[Google Scholar] [CrossRef]
- Fortier LM, Markel M, et al. An Update on Peroneal Nerve Entrapment and Neuropathy. Orthop Rev (Pavia). 2021 Jun 19;13(2):24937[Google Scholar] [CrossRef].
- Uzenot D, Cantiniaux S, Pouget J. Syndromes canalaires entre hanches et pieds. Rev Rhum 2007;74:401-8. [Google Scholar] [CrossRef]
- Dallari D, Pellacani A, Marinelli A, et al. Deep peroneal nerve paresis in a runner caused by ganglion at capitulum peronei. Case report and review of the literature. J Sports Med Phys Fitness 2004;44:436-40. [Google Scholar] [CrossRef]
- Ismael F, Wahbi S, Lahtaoui A, et al. Compression du nerf fibulaire commun par un kyste synovial. Rev Maroc Chir Orthop Traumatol 2005;24:37-9. [GoogleScholar] [CrossRef]
- Bahri H, Gomis R, et al. Complications neurologiques des lésions post-traumatiqes de la cheville. Ed Masson; 1982. p. 170-5. [Google Scholar] [CrossRef]




 Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.
Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.