Effect of implant size, version and rotator cuff tendons preservation on the outcome of Reverse Shoulder Arthroplasty
2 Imperial College NHS Trust, London, UK
3 Stockport NHS Trust, Liverpool, UK
Received: 12-Mar-2022, Manuscript No. jotsrr-22-57004; Editor assigned: 16-Mar-2022, Pre QC No. jotsrr-22-57004(PQ); Accepted Date: Mar 25, 2022 ; Reviewed: 19-Mar-2022 QC No. jotsrr-22-57004(Q); Revised: 24-Mar-2022, Manuscript No. jotsrr-22-57004(R); Published: 31-Mar-2022, DOI: Doi: 10.37532/1897- 2276.2022.17(3).70
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Introduction: Functional outcomes following reverse geometry shoulder arthroplasty can vary. This study assessed the effects of glenosphere size, humeral stem version, posterior rotator cuff status and subscapularis repair on patient reported outcome and range of motion.
Methods: A consecutive series of 132 patients from two orthopaedic centres that use the same onlay system for reverse shoulder arthroplasty were reviewed over a 6-year period. Outcome measures consisted of the Oxford Shoulder Score (OSS) and Range of Motion (ROM) at one year following surgery. These were assessed against glenosphere sizes (small (36 mm-38 mm) and large (40 mm-42 mm)), humeral stem retroversion (less or more than 20 degrees), rotator cuff status (posterior rotator cuff present or absent) and subscapularis tendon (repaired or not) at the end of procedure.
Results: Larger glenospheres and less humeral stem retroversion yielded better ROM and OSS but this was not statistically significant. Subscapularis repair had no effect on outcomes. Preservation of posterior rotator cuff tendons improved functional outcomes. The number of tendons present at the end of procedure had a positive effect on outcome (best with two tendons and better with one compared to a completely bold humeral head).
Conclusion: Preservation of posterior rotator cuff tendons during reverse shoulder arthroplasty improves clinical outcomes while subscapularis repair is found to be unnecessary. Implant size and version in reverse geometry arthroplasty have no significant effects on clinical outcome.
Keywords
rotator cuff, reverse shoulder, arthroplasty, glenosphere size, humeral retroversion
Introduction
Reverse Shoulder Arthroplasty (RSA) and Anatomical total shoulder arthroplasty are common methods used nowadays to treat shoulder joint arthritis [1]. Introduced by Neer in 1970s, Anatomical total shoulder arthroplasty has been a widely used method to treat shoulder arthritis; however, the outcome depends on the intact rotator cuff tendons [2]. Therefore, RSA came into play in 1985 as a better choice with better outcome to treat rotator cuff shoulder arthropathy.
RSA reverse the normal shoulder anatomy in order to utilize the action of deltoid muscle to replace the deficient rotator cuff. Thus, we cannot use the ordinary methods to measure the best size of prosthesis to be used to replace the originals [3-5].
Patients’ comorbidities, psychological status and preoperative ROM can all influence the outcome of RSA. The effect of Glenosphere size on range of motion (ROM) and shoulder function has been studies by computer models, physical model and in vitro cadaveric studies [6-11]. The result of bony studies which did not use any soft tissue but only changing size and angle of the Glenosphere proved that increasing the size can increase ROM especially the abduction and external rotation [12]. By clearing more space for the Polyethelene (PE) before impinging against the scapula (notching), lateralization of the glenoid component has shown to have a positive effect on ROM [13]. Subscapularis tendon repair has shown no effects on dislocation rate [14].
In this study, we assessed the effects of glenosphere size, humeral component version and the status of rotator cuff tendons on the outcome of RSA.
Method
This study consisted of a retrospective review of a consecutive series of patients with a retrospective data collection of ROM and OSS at two orthopaedics centres. The outcome measures included the range of motion and Oxford Shoulder Score pre-and postoperatively. Details from intraoperative notes included the status of the rotator cuff tendons at the end of procedure, the size and the lateralisation of the Glenosphere, the version of the humeral component and whether the subscapularis tendon was repaired or not. All cases were included in the study, except cases were surgery done because of fracture. The use of large and small glenosphere was decided by surgeon according to intra-operative measures; the repair of subscapularis done wherever the soft tissue allows without tension. The two centres used two different makes of the implant but both have a similar design (onlay system).
All procedures were performed using deltopectoral approach. Post-operative rehabilitation included early active assisted range motion in 90 degrees of flexion and abduction, 30 degrees of external rotation for 6 weeks then as patient is able afterwards. Reviews where at six weeks, six months in one year. Oxford shoulder scores were obtained at six months and one year. The ultimate range of motion was considered to be the one that is recorded at one year and was assessed clinically using a goniometer.
Procedures performed for fractures were excluded. The size of glenosphere was categorised as large (for glenospheres 40 mm or more) or small (for glenospheres smaller than 40 mm). Humeral component retroversion was categorised as less or more than 20 degrees. The status of rotator cuff tendons at the end of procedure was categorised as present or absent (including which tendon is still preserved). Besides, notes included whether the subscapularis tendon was repaired at the end of procedure or not (because it was not possible or because the subscapularis was absent).
Mann Whitney U test compared the improvement in the OSS and ROM between the two groups, while Subscapularis repair assessed using Fisher’s exact test. The effect of humeral retroversion was assessed using chi-square test. Statistical analysis was carried out using the IBM SPSS version 26; a p-value of less than 0.05 was considered statistically significant.
Results
The total number of patients involved in the study was 132; the mean age of patients was 58 years old (40 to 84); there were 88 males and 44 females. All the data for the 132 patients were available for one year follow up including OSS and ROM.
There was one patient with axillary nerve palsy who made a full recovery by 2 years after surgery. Two patients had acromial stress fractures that healed by 12 months postoperatively. There were no cases of dislocation or periprosthetic fractures.
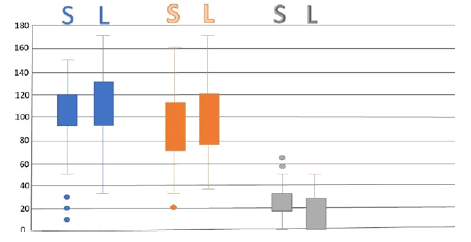
There were 22 patients who had the large size glenosphere and 110 patients had the small size glenosphere; In the small glenosphere group, the median ROM at one year was 100 for flexion, 90 for abduction and 20 degrees for external rotation and the median OSS was 32. In the large glenosphere group, the median ROM at one year was 100 for flexion, 95 for abduction and 22 for external rotation and the median OSS was 36; the distribution of ROM for both groups (Figure 1).
The use of large glenosphere led to a better ROM and OSS; however, this was not statistically significant (Table 1).
Table 1. Effect of Glenosphere size on the Outcome
| Category | Large Glenosphere Group | Small Glenosphere Group | P Value |
| Total Number of Patients | 22 | 110 | --- |
| Median Flexion in one year* | 100 | 100 | 0.66 |
| Median Abduction in one year* | 95 | 90 | 0.35 |
| Median External Rotation in one year* | 22 | 20 | 0.32 |
| Median Oxford Shoulder Score in one year* | 36 | 32 | 0.29 |
| Subscapularis Repair (%) ** | 15(68%) | 80(72%) | 0.67 |
If we assessed the repair of subscapularis as an independent factor to evaluate its effect on External Rotation and OSS in one year follow up. In total, the subscapularis was repaired in 95 out of 132 patients (72%) at the end of procedure. The result showed a mean OSS of 32 at one year and a median of ER of 20 degrees. This was compared to a mean of OSS of 32 and a median of ER of 22 degrees in those who did not have the subscapularis repaired. The repair of subscapularis had no effect on OSS at one year follow up. However, I did restrict the external rotation by few degrees but this was neither clinically nor statistically significant (p value is 0.67).
Regarding the humeral retroversion, 54% of patients had retroversion more than 20 degrees; in patients with retroversion of 20 degree or less, the median ROM was 100 degrees for flexion, 94 degrees for abduction and 23 degrees for external rotation and the median OSS score was 35. This is compared to a median ROM of 100 for flexion, 95 for abduction and 22 for external rotation 22 in patients with aretroversion of more than 20 degrees and a median OSS of 32, Chi-Square test used to assess the correlation between retroversion and ROM and OSS; the correlation was statistically non-significant. Humeral component retroversion had no impact on ROM and OSS in this study (Table 2).
Table 2. Effect of Humeral Retroversion on Outcome
| Category | Humeral retroversion <= 20 degrees | Humeral Retroversion >20 degrees | P Value |
| Total number of patients | 71 | 61 | --- |
| Mean Flexion in one year * | 100 | 100 | 0.66 |
| Mean Abduction in one year * | 94 | 95 | 0.32 |
| Mean External Rotation in one year * | 23 | 22 | 0.65 |
| Mean Oxford Shoulder Score in one year * | 35 | 32 | 0.91 |
The status of rotator cuff tendons at the end of
the procedure was divided into 4 categories:
1. All present but degenerative supraspinatus
2. Only Supraspinatus is absent
3. Only Teres minor is present Category
4. All torn (bald head)
Results showed that the number of intact tendons positively affects the functional outcome. The mean flexion, abduction and ER were significantly better when we compared each of categories 1, 2 and 3 to category 4. Teres minor was found to be the most important as its presence alone yielded as good function as that from intact tendons in category 1 and 2. (no statistically significant difference between means of ROM parameters between category 1 and 3 and also between 2 and 3) (Table 3).
Table 3. Effect of Rotator cuff status on the Outcome
| Rotator cuff status | Number of patients(percentage) | Mean Flexion | Mean Abduction | Mean Ex Rotation | OSS |
| Category 1: teres ok, infra ok, supra present but (pasta or degenerative) | 62(47%) | 125.6 | 100.7 | 30 | 36 |
| Category 2: Teres ok, infra ok, supra-absent | 32(24%) | 128 | 100.3 | 28 | 34 |
| Category 3: Teres ok, infra torn | 12(9%) | 123.3 | 95 | 25 | 34 |
| Category 4: All torn | 26(20%) | 103.7 | 88 | 20 | 32 |
Discussion
In theory, larger glenospheres lead to a better ROM and more stability compared to smaller ones [15]. Other factors such as the status of rotator cuff tendons, preoperative ROM and other patient-related factors can affect the functional outcome of RSA [16,17]; in this study, we focused primarily on the effects of glenosphere size, humeral component version and the rotator cuff status on the outcome.
Daniel et al, studied the effect of the glenosphere size on the joint reaction force and ROM, he proved that the larger the size the better the ROM and more joint reaction force but yet didn’t assess the soft tissue factors [17]. The glenosphere size did not have a significant effect on the ROM or the functional score; despite the subtle differences in the range of flexion and external rotation in favour of larger glenospheres, this difference was neither clinically nor statistically significant (p value: 0.35 and 0.32 respectively). Such a result can be attributed to the fact that the outcome is a result of interplay of many other factors one of them is the rotator cuff status.
Joshua W. Giles et al, investigated the impact of cuff repair on RSA outcome, they investigated the effect of both the cuff repair and the glenosphere lateralization in vitro [18]. Interestingly, they concluded that cuff repair antagonize the RSA function. Likewise researcher studied the impact of rotator cuff repair prior to RSA and concluded that this did not offer any significant improvement [19]. In contrary, our study showed that intact rotator cuff tendons yield better function and that out of all 4 tendons; Teres minor was found to be the most important. This could be explained by the potential preservation of external rotation while the arm is abducted, a function that is provided by teres minor and that is required in many daily tasks [20]. We believe that preservation of as much rotator cuff tendons as possible during RSA should theoretically offer a better outcome, but this needs to be studied further through randomized trials. Scientist studied the effect of humeral retroversion on ROM in RSA and concluded that more retroversion conferred a better ROM; in their study, the variation in retroversion was quite vast (-20 degrees to +40 degrees) and that is difference between the lowest and highest two retroversion recorded in their series of patients [21]. In our study, retroversion of humeral implant had no impact on range of motion or function, and this conforms the findings of other studies [22, 23].
However, it is important to note that the variation of retroversion in our series of patients was between 5 and 30 degrees and, when compared to the study by scientists, we can conclude that it is possible that retroversion within 40 degrees (within normal variants) does not have impact on ROM and function. Author studies the effect of subscapularis repair on RSA dislocation rate; they found there is significant relation between the repair and the dislocation rate, the more the repair the less the dislocation rate. Unlike our study which showed of 28% of cases with no subscapularis repair done, none have a recorded dislocation.
Conclusion
Preservation of rotator cuff tendons during reverse shoulder arthroplasty improves clinical outcomes while subscapularis repair is found to be unnecessary. Implant size and version in reverse geometry arthroplasty have no significant effects on clinical outcome.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author’s Contribution
Mustafa Al-Yaseen result writing, statistics and discussion writing; Yatwing Smart Introduction writing, data collection; Parisah Seyed-Safi study methods writing; Abdelmonem Hassan discussion writing; Daoud Makki revising the article and supervise writing and editing; Barnes Morgan data collection and editing; Dilraj Sandher Data collection and editing
Ethics Approval
Ethical approval was not sought for the present study because it’s a retrospective study using existing Data. This study was completed in accordance with the Helsinki Declaration as revised in 2013.
References
- Bohsali K.I., Wirth M.A., Rockwood Jr.: Complications of total shoulder arthroplasty. J Bone Jt Surg. 2006; 88: 2279-2292. Google scholarCrossref
- Deore V.T., Griffiths E., Monga P.J., et al.: Shoulder arthroplasty past, present and future. J Arthrosc Jt Surg. 2018; 5: 3-8. Google scholarCrossref
- Castagna A., Delcogliano M., Caro F., et al.: Conversion of shoulder arthroplasty to reverse implants: clinical and radiological results using a modular system. Int Orthop. 2013; 37:1297-1305. Google scholarCrossref
- Drake G.N., Connor D.P., Edwards T.B., et al.: Indications for reverse total shoulder arthroplasty in rotator cuff disease. Clin Orthop Relat Res. 2010; 468:1526-1533. Google scholarCrossref
- Langohr G.D., Giles J.W., Athwal G.S., et al.: The effect of glenosphere diameter in reverse shoulder arthroplasty on muscle force, joint load, and range of motion. J Shoulder Elb Surg. 2015; 24: 972-979. Google scholarCrossref
- Friedman R.J., Eichinger J., Schoch B., et al.: Preoperative parameters that predict postoperative patient-reported outcome measures and range of motion with anatomic and reverse total shoulder arthroplasty. JSES Open Access. 2019; 3:266-272. Google scholarCrossref
- Biase C.F., Ziveri G., Delcogliano M., et al.: The use of an eccentric glenosphere compared with a concentric glenosphere in reverse total shoulder arthroplasty: two-year minimum follow-up results. Int Orthop. 2013; 37:1949-1955. Google scholarCrossref
- Gutirrez S., Comiskey C.A., Luo Z.P., et al.: Range of impingement-free abduction and adduction deficit after reverse shoulder arthroplasty: hierarchy of surgical and implant-design-related factors. J Bone Jt Surg. 2008; 90: 2606-2615. Google scholarCrossref
- Gutirrez S., Keller T.S., Levy J.C., et al.: Hierarchy of stability factors in reverse shoulder arthroplasty. Clin Orthop Relat Res. 2008; 466:670-676. Google scholarCrossref
- Gutirrez S., Levy J.C., Frankle M.A., et al.: Evaluation of abduction range of motion and avoidance of inferior scapular impingement in a reverse shoulder model. J Shoulder Elb Surg. 2008; 17:608-615. Google scholarCrossref
- Kukkonen J., Kauko T., Vahlberg T., et al.: Investigating minimal clinically important difference for Constant score in patients undergoing rotator cuff surgery. J Shoulder Elb Surg. 2013; 22:1650-1655. Google scholarCrossref
- Virani N.A., Cabezas A., Gutirrez S., et al.: Reverse shoulder arthroplasty components and surgical techniques that restore glenohumeral motion. J Shoulder Elb Surg. 2013; 22:179-187. Google scholarCrossref
- Werner B.S., Chaoui J., Walch G.J., et al.: The influence of humeral neck shaft angle and glenoid lateralization on range of motion in reverse shoulder arthroplasty. J Shoulder Elb Surg. 2017; 26:1726-1731. Google scholarCrossref
- Edwards T.B., Williams M.D., Labriola J.E., et al.: Subscapularis insufficiency and the risk of shoulder dislocation after reverse shoulder arthroplasty. J Shoulder Elb Surg. 2009; 18: 892-896. Google scholarCrossref
- Frankle M.A., Teramoto A., Luo Z.P., et al.: Glenoid morphology in reverse shoulder arthroplasty: classification and surgical implications. J Shoulder Elb Surg. 2009; 18: 874-885. Google scholarCrossref
- Churchill R.S., Brems J.J., Kotschi H.J., et al.: Glenoid size, inclination, and version: an anatomic study. J Shoulder Elb Surg. 2001; 10:327-332. Google scholarCrossref
- Humphrey C.S., Kelly J.D., Norris T.R., et al.: Optimizing glenosphere position and fixation in reverse shoulder arthroplasty, part two: the three-column concept. J Shoulder Elb Surg. 2008; 17:595-601. Google scholarCrossref
- Giles J.W., Langohr G.D.G., Johnson J.A., et al.: The rotator cuff muscles are antagonists after reverse total shoulder arthroplasty. J Shoulder Elb Surg. 2016; 25: 1592-1600. Google scholarCrossref
- Erickson B.J., Ling D., Wong A., et al.: Does having a rotator cuff repair prior to reverse total shoulder arthroplasty influence the outcome? Bone Jt J. 2019; 101-B:63-67. Google scholarCrossref
- Werner B.C., Wong A.C., Mahony G.T., et al.: Causes of poor postoperative improvement after reverse total shoulder arthroplasty. J Shoulder Elb Surg. 2016; 25:e217-e222. Google scholarCrossref
- Stephenson D.R., Oh J.H., McGarry M.H., et al.: Effect of humeral component version on impingement in reverse total shoulder arthroplasty. J Shoulder Elb Surg. 2011; 20:652-658. Google scholarCrossref
- Gulotta L.V., Choi D., Marinello P., et al.: Humeral component retroversion in reverse total shoulder arthroplasty: a biomechanical study. J Shoulder Elb Surg. 2012; 21:1121-1127. Google scholarCrossref
- Aleem A.W., Feeley B.T., Austin L.S., et al.: Effect of humeral component version on outcomes in reverse shoulder arthroplasty. Orthopedics. 2017; 40:179-186. Google scholarCrossref



 Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.
Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.