Efficacy of common stabilization techniques on protecting the ulnar collateral ligament of the thumb: A cadaveric study
2 Northeast Ohio Medical University College of Medicine 4209 St, OH-44, Rootstown, OH, 44272, USA
3 School of Health and Rehabilitation Sciences, The Ohio State University College of Medicine 453 W 10, USA
Received: 19-Sep-2022, Manuscript No. JOTSRR-22-75217;; Editor assigned: 21-Sep-2022, Pre QC No. JOTSRR-22-75217;(PQ); Accepted Date: Oct 07, 2022 ; Reviewed: 02-Oct-2022 QC No. JOTSRR-22-75217;(Q); Revised: 03-Oct-2022, Manuscript No. JOTSRR-22-75217;(R); Published: 08-Oct-2022, DOI: 10.37532/1897- 2276.2022.17(9).72
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Introduction: The thumb ulnar collateral ligament is commonly injured, especially during sport, resulting in an acute injury that must be appropriately managed
Purpose of Study: To evaluate the effectiveness of common stabilization techniques for the thumb UCL in fresh cadaveric specimens and to analyze the anatomical differences between male and female UCLs.
Methods: Eight, fresh cadaveric specimens (79 ± 8 years old) were evaluated in four conditions; nostabilization, spica tape job, abduction tape job, and an over the counter spica orthosis. The forearm was stabilized, positioning the thumb in neutral. The thumb was attached to a Teflon rail-guided drop tower using an impact load transfer system designed to abduct the thumb with 131 Newton (N) of force. TEMA motion analysis software was used to calculate the maximum abduction angles at impact. Following biomechanical testing, an incision was performed along the ulnar aspect of the thumb to expose the UCL for measurement.
Conclusions: This is the first study to assess the efficacy of commonly used thumb stabilization methods. Bracing is often regarded as superior to taping, but these data suggest otherwise. This information may aid clinicians in understanding how to best protect the thumb UCL from sustaining initial injury and protection when returning to sport.
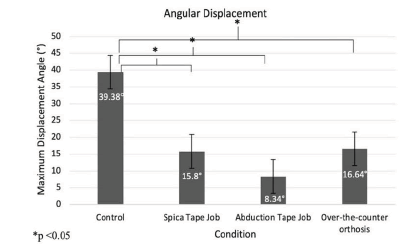
Results: All stabilization conditions significantly limited thumb abduction. The thumb abduction tape job was most effective (8.3°), followed by the spica tape job (15.8°), and the spica orthosis (16.6°). Each specimen was dissected following testing and no ligament damage was identified. No statistically significant difference was found between the length and width of male and female thumb UCLs.
Key Words
thumb ulnar collateral ligament, thumb injury, skier’s thumb, thumb stabilization, prevention
Introduction
Hand injuries in athletics frequently involve the collateral ligaments at the metacarpophalangeal (MCP) joint of the thumb. Rupture to the ulnar collateral ligament (UCL) accounts for approximately 86% of all injuries occurring at the base of the thumb [1-5]. The injury commonly occurs during sport-related activities when the thumb is forcefully abducted at the MCP joint, causing the ligament to stretch and sometimes tear completely [1].
Injury to the UCL was previously referred to as Gamekeeper’s thumb because it was common among Scottish gamekeepers in the twentieth century [6]. Gamekeeper’s thumb is also known as the skier’s thumb, which refers to the high incidence of this specific ligamentous injury in skiers [7]. Injury to the UCL is prevalent in a wide variety of contact sports; including soccer, fighting, and American football [7]. This injury jeopardizes an athlete’s ability to compete and perform at a competitive level. Long-term complications include weakened grip strength, instability, pain, and secondary osteoarthritis [8-9]. Chronic laxity of the UCL can occur due to repetitive valgus stress; however instantaneous mechanisms are more likely to result in an acute injury of the UCL [10].
Biomechanical testing has been conducted on the thumb UCL to determine load-to-failure ratios, primarily when comparing the strength of repaired ligaments using a variety of surgical techniques [1,11-14]. The surgical technique used to repair the UCL depends on the anatomy of the lesion. Repairing the UCL often includes one or two suture anchors to reattach the ruptured ligament to its insertion site [2] Biomechanical testing of the UCL, including post-surgical repair and load to failure ratios of the intact ligament has been conducted at slow rates, including the abduction of the thumb 0.1 mm/s and 1 mm/s[1,11-13].
While a significant amount of data has been collected from these biomechanical studies, there is minimal data examining the rupture of the UCL at high loading rates, such as those seen in athletics. Injuries that do not require surgery may be treated conservatively, but that decision depends on various factors, including the grade of injury, location of the tear, and patientrelated factors [5,15]. When treating an athlete with this injury, it is important to properly protect the athlete, especially when returning to the sport, ideally with non-bulky but supportive devices for overall thumb stabilization to prevent further complications. Therefore, the objective of this study was to evaluate the effectiveness of three common stabilization devices for the thumb UCL in fresh cadaveric specimens. An additional objective of this study was to quantify the dimensions of the thumb UCL in vivo and to evaluate any differences based on sex.
Method
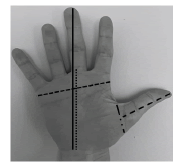
Eight fresh cadaveric right hands (4 females, 4 males; average age, 79 ± 8 years) were obtained. The specimens were harvested at midforearm and thawed to room temperature. Anthropometric measurements were obtained using a digital caliper (Model 1467, General Tools & Instruments, New York, NY) and included hand length, palm length, hand breadth, thumb length, thumb circumference, and range of motion at the carpometacarpal (CMC) and MCP joints (Figure 1).
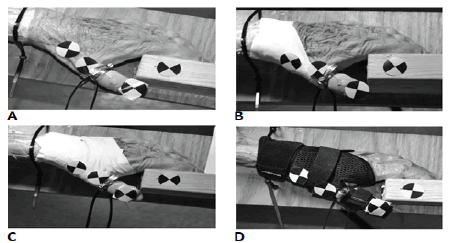
A hand-held goniometer was used to measure thumb abduction at the CMC joint and valgus movement at the MCP joint. The specimens were prepared for testing in four conditions which were assigned in random order. Conditions included a thumb spica tape job (SpicaT), a thumb abduction tape job (AbdT), an Over-The-Counter thumb spica orthosis (OTC) (Mueller Sports Medicine, Prairie Du Sac, WI), and a no-stabilization device condition which acted as the control condition (Cont) (Figure 2).
The spica tape job condition was executed by first placing an anchor strip around the wrist with 1.5-inch athletic tape (Johnson and Johnson, Pensacola, FL), then three figure-eight strips were applied independently around the 1st MCP joint with 0.5-inch athletic tape, followed by a closure strip of 1.5- inch tape placed around the wrist. The AbdT condition was completed along the radial aspect of the thenar eminence and the thumb, first by placing an anchor strip of 1.5-inch tape around the palm and wrist, then placing u-strips connecting to the anchors, spanning from the dorsal to the palmar surface from the CMC to the MCP joint. Lastly, closure strips were placed around the wrist and palm. Tape jobs were performed by an Athletic Trainer (LCB) with 20 years of experience. Both taping applications function to protect the thumb against forced abduction. Following preparation, the hand was secured in a custom fixture (Figure 3).
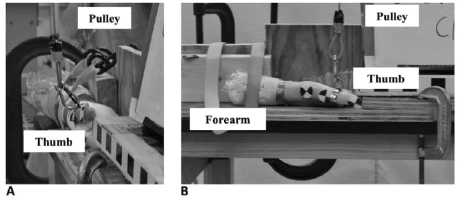
The thumb was placed in a neutral position for each test condition, at approximately a 30° flexed position, as suggested by the literature [16-18]. The thumb was then secured with a hose clamp 15 mm distal to the MCP joint of the thumb. The hose clamp was attached to a cable pulley system connected to a vertical Teflon-rail guided drop tower (Figure 4).
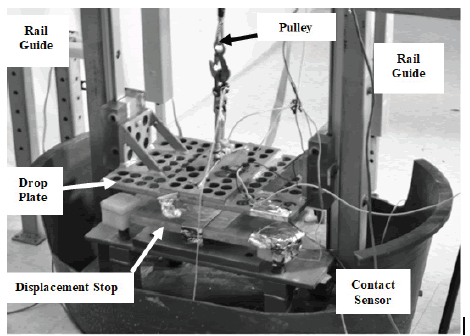
The drop tower’s load platform starting position was exactly 0.5 m above the impact site each time to control velocity, energy, and force. A small amount of slack was given in the cable to allow the thumb to remain neutral an inch above the stoppers on the tower. Once taught, the falling platform of approximately 131 N of force was applied to the thumb. A light trap was used to measure the precise speed at impact. A high-speed video camera (Phantom MIRO M320S, Vision Research, Inc.) was situated to capture thumb abduction from a lateral view at approximately 1,000 frames per second.
TEMA motion analysis software (Image Systems Nordic AB, Linkoping, Sweden) was used to analyze videos of thumb abduction and calculate the maximum abduction angle at impact (Figure 5).
Abduction angles were calculated using the distal interphalangeal joint of the second digit, CMC joint, and MCP joint of the thumb as points of reference. Paired t-tests were run comparing abduction angles of the stabilization conditions to the control group. Consistency between the velocity, acceleration, energy, and force was assessed using the coefficient of variation for each test. After biomechanical testing was performed, each hand was dissected for further analysis. An incision was performed along the ulnar aspect of the thumb and excess tissue was removed. The thumb UCL was exposed and its relationship to the adductor policies muscle was observed. An independent t-test was performed comparing the means of the UCL length and width concerning sex. All statistics were analyzed using IBM SPSS Statistics, version 25 (IBM Corp., Armonk, NY).
Results
Eight fresh-frozen cadavers were included in this investigation. Anthropometry measurements performed after biomechanical testing is listed below (Table 1).
Table 1: Anthropometric data
| Specimen | Age | Sex | Hand Length (mm) | Palm Length (mm) | Hand Breadth (mm) | Thumb Length (mm) | Thumb Circumference (mm) | UCL Length (mm) | UCL Width (mm) | MCP Range of Motion (degrees) |
|---|---|---|---|---|---|---|---|---|---|---|
| (yrs) | ||||||||||
| 1 | 76 | M | 18.9 | 9.8 | 9.1 | 6.5 | 7.9 | 11.6 | 3.5 | 23 |
| 2 | 64 | M | 18.5 | 10.9 | 7.8 | 6.9 | 6.9 | 14.5 | 5.1 | 34 |
| 3 | 89 | F | 18.6 | 10.5 | 7.2 | 7 | 5.5 | 13.6 | 6.8 | 34 |
| 4 | 81 | F | 18 | 9.8 | 7.9 | 6 | 7.2 | 11.9 | 5.1 | 42 |
| 5 | 86 | M | 19.4 | 10.6 | 8.3 | 7.6 | 7.1 | 11.2 | 4 | 24 |
| 6 | 84 | F | 16.5 | 9.8 | 7.1 | 5.7 | 7 | 11.7 | 4.7 | 46 |
| 7 | 74 | F | 15.8 | 9 | 6.8 | 5.8 | 21 | 8.8 | 3.6 | 25 |
| 8 | 76 | M | 18.8 | 10.9 | 7.8 | 7.4 | 6.5 | 12 | 5 | 30 |
| Mean | 79 | 18.1 | 10.2 | 7.8 | 6.6 | 6.7 | 11.9 | 4.7 | 32 | |
| (SD) | -8 | -1.3 | -0.7 | -0.7 | -0.7 | -0.8 | -1.7 | -1.1 | -8 |
Mean thumb abduction angles at impact for the Cont was 39.38° ± 13.70°, SpicaT was 15.80° ± 6.20°, AbdT was 8.34° ± 10.92°, and OTC was 16.64° ± 10.32° (Figure 6).
The abduction angles were scaled to account for variable thumb length, but no significant differences were found. Paired t-tests revealed significant differences between the Cont and each stabilization device (p<0.05) (Table 2).
Table 2: Paired sample t-test results
| Conditions | T (df) | p-value |
|---|---|---|
| Cont vs. SpicaT | 8.477 (7) | <0.001 |
| Cont vs. AbdT | 7.818 (7) | <0.001 |
| Cont vs. OTC | 6.056 (7) | 0.001 |
| SpicaT vs. AbdT | 3.800 (7) | 0.007 |
| SpicaT vs. OTC | -0.652 (7) | 0.535 |
| Abd T vs. OTC | -4.070 (7) | 0.005 |
The control allows significantly more abduction than any of the stabilizing conditions. The trials were randomized, and time intervals were recorded between each test for consistency and to consider recovery of the specimen tissue, primarily the adductor pollicis muscle. The average time between trials was 11 ± 3 minutes. The coefficient of variation for velocity= 1.6 (range 2.5 m/s-2.64 m/ s), acceleration = 3.6 (range 7.0 m/s2-7.84 m/s2), energy=3.3 (range 62.8 J-70.6 J), and force = 3.26 (range 125.5 N- 141.2 N).
Following the biomechanical testing, each thumb was dissected. An independent t-test was used to determine the differences between male and female hand anthropometric dimensions and UCL dimensions. There was a significant difference between males and females regarding hand length, hand breadth, and thumb length (p<0.05). No significant difference was found when comparing palm length, thumb circumference, and range of motion of the CMC and MCP joints, respectively. There was no significant difference between the length of the UCL between males and females (t (6)=0.663, p= 0.524).
Discussion
The primary objective of this study was to evaluate the effectiveness of common stabilization techniques for the thumb UCL by measuring angular displacement in fresh cadaveric specimens. Results demonstrate that the AbdT and SpicaT were more effective at reducing mean abduction angles of the thumb at the CMC and MCP joints than the OTC orthosis, and all were better than no stabilization device at all. The AbdT reduced mean abduction angles by 78.8%, the spicaT condition reduced mean abduction angles by 59.9%, and the OTC orthosis reduced mean abduction angles by 57.7% when compared to Cont.
The average abduction angles for the control (39.38O ) are consistent with previous literature (32.6O ) [1]. Our average abduction angles in the stabilization conditions can be compared to a custom orthosis described in the literature (24.0°) in up to 100 N of force applied [1]. Our study offers insight into the thumb and UCL stability against valgus forces at a high rate of speed.
Previous studies tested the UCL and thumb abduction at rates of 0.1 mm/s and 1 mm/s and mainly looked at load-to-failure ratios, pinch, and grip forces of the UCL [1,13,14]. While these studies offer a great deal of information regarding the properties of the thumb UCL, it is difficult to apply this to a real-time injury mechanism of injury. We consistently abducted the thumb at rates of approximately 1 m/s, which is much higher than the rates of thumb abduction described in the literature [1,13,14]. Our rationale for choosing 1 m/s was to make our rates of abduction considerably closer to real-life scenarios, whereas other studies applied abduction rates several magnitudes lower [1,13,14]. Our study is more representative of the instantaneous mechanism of injury sustained by many athletes in contact and non-contact sports. Determining the necessary thumb abduction force was also difficult because of the wide range of UCL load to failure values reported in the literature, which ranged from 111 N to 156 N and 246 N to 513 N in two biomechanical studies with fresh cadaveric specimens [1,14]. The force applied to the thumb in our study ranged from 111 N to 150 N. After dissection of the fresh cadaveric specimens, it was determined that there were no ligament failures. There was no preload applied to the thumb during the biomechanical testing because a small preload of 1 pound was able to almost fully abduct the thumb, which could be attributed to the increased flexibility of the fresh specimen tissue.
The final objective of this study was to assess for damage to the ligament, quantify the dimensions of the UCL in vivo, and evaluate any differences based on sex. A retrospective analysis by Boesmueller et al.
(2017) determined that women were prone to lower velocity injuries to the thumb UCL, leading to mid-substance tears. Men, however, were more prone to intense mechanisms of injury, and primarily resulted in distal ligament or bony avulsion fractures [16]. This information could further be explained if there was an anatomical difference between male and female UCL dimensions regarding anthropometric measurements of the hand and thumb. We found a significant difference between hand length, hand breadth, and thumb length (p<0.05), however, there was no significant difference between the ligament length and width when comparing between sexes.
Recent literature indicated that there is no statistically significant difference in UCL length between males and females in their dominant hand as indicated on ultrasound [19]. However, a statistically significant difference was found between males and females in their non-dominant hands [19]. This information does further raise the question of why males and females have different rupture sites. On average, our specimens UCL width and length were within the ranges described previously in the literature; 4 mm-8 mm wide and 12 mm-14 mm long [20]. The origin of the UCL was confirmed, located on the dorsal aspect of the first metacarpal and inserted onto the medial aspect of the base of the proximal phalanx of the thumb [2]. Further anatomical and biomechanical studies should be conducted to confirm the difference in the location of UCL rupture between males and females.
The biomechanical portion of the study had several limitations. Subtle variation in the tension and placement of tape during the taping procedures could be attributed to the specimen rigidity and a lack of dynamic feedback. The exact fit of the OTC orthosis was also a factor, as the cadaveric hands were various sizes. We used a universal orthosis that fit each specimen; however, smaller hands may have allowed for excess movement within the orthosis during testing. The small sample size is one of our greatest limitations, which is why we choose the methodology of assessing all four conditions on each specimen. The repeated motion could have resulted in an increased tissue laxity in the specimen, however, we tried to control for this by randomizing the order that the stabilization techniques were applied. Lastly, due to the use of cadaveric specimens, we were not able to obtain information regarding hand dominance, which could affect the strength of the intrinsic and extrinsic musculature of the hand.
Conclusion
When protecting the thumb UCL, it is essential to prevent the thumb from excessive abduction, while allowing the athlete to use the affected hand as much as possible for maximum desired performance. This study, to our knowledge, was the first to evaluate maximum thumb abduction angles at high velocities to assess the efficacy of commonly used thumb stabilization methods trying to find the most effective protection for the UCL. Protective taping or bracing is used in many aspects of athletics to help prevent or provide a safe return to play a following injury. These data suggest that taping methods are superior to bracing, though more study is warranted. This information may aid clinicians in understanding how to best protect the thumb UCL from sustaining initial injury and protection when returning to sport.
References
- Gil JA, Ebert K, Blanchard K, et al. Efficacy of a radial-based thumb metacarpophalangeal-stabilizing orthosis for protecting the thumb metacarpophalangeal joint ulnar collateral ligament. J Hand Ther. 2019;32(1):80-85. [Google Scholar] [CrossRef]
- Mahajan M, Rhemrev SJ. Rupture of the ulnar collateral ligament of the thumb - a review. Int J Emerg Med. 2013 Aug 12;6(1):31.[Google Scholar] [CrossRef]
- Lee AT, Carlson MG. Thumb metacarpophalangeal joint collateral ligament injury management. Hand Clin. 2012 Aug;28(3):361-70. [Google Scholar] [CrossRef]
- Moutet F, Guinard D, Lebrun C, et al. Metacarpo-phalangeal thumb sprains based on experience with more than 1,000 cases. Ann Chir Main. 1989;8(2):99-109. [Google Scholar] [CrossRef]
- Ritting AW, Baldwin PC, Rodner CM. Ulnar collateral ligament injury of the thumb metacarpophalangeal joint. Clin J Sport Med. 2010 Mar;20(2):106-12. [Google Scholar] [CrossRef]
- CAMPBELL CS. Gamekeeper's thumb. J Bone Joint Surg Br. 1955 Feb;37-B(1):148-9. [Google Scholar] [CrossRef]
- Harding P, McKeag L. Skier's thumb: a literature review. Aust J Physiother. 1995;41(1):29-33. [GoogleScholar] [CrossRef]
- Bernstein DT, McCulloch PC, Winston LA, et al. Early Return to Play With Thumb Spica Gauntlet Casting for Ulnar Collateral Ligament Injuries Complicated by Adjacent Joint Dislocations in Collegiate Football Linemen. Hand (N Y). 2020 Jan;15(1):92-96. [CrossRef] [Google Scholar]
- McCue FC 3rd, Hakala MW, Andrews JR, et al. Ulnar collateral ligament injuries of the thumb in athletes. J Sports Med. 1974 Mar-Apr;2(2):70-80. [Google Scholar] [CrossRef]
- Richard JR. Gamekeeper's thumb: ulnar collateral ligament injury. Am Fam Physician. 1996 Apr;53(5):1775-81. [CrossRef] [Google Scholar]
- Harley BJ, Werner FW, Green JK. A biomechanical modeling of injury, repair, and rehabilitation of ulnar collateral ligament injuries of the thumb. J Hand Surg Am. 2004 Sep; 29(5):915-20. [Google Scholar] [CrossRef]
- Lien JR, Brunfeldt A, Julka A, et al. Ulnar collateral ligament strain of the thumb metacarpophalangeal joint: biomechanical comparison of two postoperative immobilization techniques. Hand (N Y). 2015 Dec;10(4):721-5. [Google Scholar] [CrossRef]
- Shin EH, Drake ML, Parks BG, et al. Hook Plate Versus Suture Anchor Fixation for Thumb Ulnar Collateral Ligament Fracture-Avulsions: A Cadaver Study. J Hand Surg Am. 2016 Feb;41(2):192-5.[CrossRef] [Google Scholar]
- Firoozbakhsh K, Yi IS, Moneim MS, et al. A study of ulnar collateral ligament of the thumb metacarpophalangeal joint. Clin Orthop Relat Res. 2002 Oct;(403):240-7. PMID: 12360033. [CrossRef] [Google Scholar]
- Madan SS, Pai DR, Kaur A, Dixit R. Injury to ulnar collateral ligament of thumb. Orthop Surg. 2014 Feb;6(1):1-7.[CrossRef] [Google Scholar]
- Boesmueller, S., Huf, W. Retti, G. et al. The influence of sex and trauma impact on the rupture site of the ulnar collateral ligament of the thumb. PLoS ONE. 2017; 12: 1-10. [CrossRef] [Google Scholar]
- Timm KE. Pollex valgus: orthopaedic management for ulnar instability of the metacarpophalangeal joint of the thumb. J Orthop Sports Phys Ther. 1985;6(6):334-42. [CrossRef] [Google Scholar]
- Mayer SW, Ruch DS, Leversedge FJ. The influence of thumb metacarpophalangeal joint rotation on the evaluation of ulnar collateral ligament injuries: a biomechanical study in a cadaver model. J Hand Surg Am. 2014 Mar;39(3):474-9. [Google Scholar] [CrossRef]
- Cagnolati AF, Nader M, Nogueira-Barbosa MH, et al. Ultrasonographic characterization of the ulnar collateral ligament of normal thumbs in different age groups. Clinics (Sao Paulo). 2018 Oct 29;73:e162. [CrossRef] [Google Scholar]
- Carlson MG, Warner KK, Meyers KN, et al. Anatomy of the thumb metacarpophalangeal ulnar and radial collateral ligaments. The Journal of Hand Surgery. 2012 Oct;37(10):2021-2026. [CrossRef] [Google Scholar]




 Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.
Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.