Evaluation of results of Minimally Invasive Plate Osteosynthesis (MIPO) with long PHILOS plate for complex metadiaphyseal proximal humerus fractures in elderly
Received: 04-Oct-2021, Manuscript No. jotsrr-21-43623; Editor assigned: 07-Oct-2021, Pre QC No. jotsrr-21-43623(PQ); Reviewed: 21-Oct-2021 QC No. jotsrr-21-43623(Q); Revised: 02-Jan-2023, Manuscript No. jotsrr-21-43623(R); Published: 30-Jan-2023
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: Proximal humerus fractures are common in elderly people. The purpose of the study is to evaluate the results of Minimally Invasive Plate Osteosyhthesis (MIPO) plating with Long PHIL
Methods: A prospective observation study conducted between 1st January 2017 to 30th December 2019. Total 10 elderly patients between 62 to 81 years of age with metadiaphyseal proximal humerus fractures were included. Radiological assessment was done at 6 weeks, 3 months, 6 months and at 1 year follow up. Functional evaluation was done with DASH score and Constant- Murley score at 1 year follow up.
Results: 100% union rate was observed. No case of non-union, malunion, infection, nerve injury and implant breakage was reported. 1 case had shoulder impingement at final follow up. The average DASH score was 23.7 and average Constant-Murley score was 82.6 at 1 year follow up.
Conclusion: MIPO is a safe and effective method for complex metadiaphyseal proximal humerus fractures in the elderly.
Keywords
Proximal humerus, radiological assessment, malunion, infection
Introduction
Proximal humerus fractures are the third most common fractures in elderly. Traditionally most of fractures are treated conservatively. However conservative methods in elderly patients with weak bones demand prolonged immobilization which can lead to joint stiffness, contractures and disuse osteoporosis. Hence for the fractures where conservative treatment is unsuccessful surgical treatment is recommended. The commonly used surgical methods are open reduction internal fixation with plating and antegrade intramedullary nailing. However both methods are associated with shortcomings. Nailing is a percutaneous method but is prone to complications like shoulder stiffness and non-union. For entry portal rotator cuff is to be cut to make entry portal. In elderly people with already some degree of shoulder periarthritis shoulder rehabilitation is troublesome. For open plating large skin incisions and extensive soft tissue dissection in needed this increases the complications like infection, non-union and radial nerve injury. Elderly people with low immunity, associated morbidities and osteoporosis are more prone to such complications [1].
With better understanding of fracture healing the philosophy of fracture stabilization has changed over the years from absolute mechanical stability to balance between fracture biology and mechanical stability. Minimally Invasive Plate Osteosynthesis (MIPO) is one such method where fracture biology is preserved and relative stability is provided to achieve fracture union. There are very few studies on MIPO plating for proximal metadiaphyseal humerus fractures [2].
The aim of this study was to evaluate the outcomes of complex metadiaphyseal proximal humerus fractures in elderly who were treated by long PHILOS plating using MIPO technique [3]. Patients with pathological fractures, open fractures and polytrauma patients were excluded from the study. Patients with underlying malignancy and on immunosuppressant drugs were also excluded from the study. Complete data about patient demographics, blood loss during surgery, surgical time and fracture union time was recorded [4].
Case Report
SURGICAL PROCEDURE
Patients were operated under general anesthesia and interscalene block anesthesia. The operating table was turned 180° as foot end of the table allowed us better movement of C arm. Patients were operated in beach chair position. C arm was kept on the opposite side of the operating surgeon. Proximally deltoid splitting approach was used. After palpating anterolateral corner of acromion 5 cm incision was given. After subcutaneous dissection raphe between anterior and middle fibres was identified and split. Axillary nerve was palpated and protected using finger dissection. Axillary nerve was gently lifted from bone by fingers while passing plate under it. No forceful traction was applied on axillary nerve. Before making distal window fracture was reduced by traction and gentle manipulation. A philos plate was put on the skin and plate length required was confirmed on X ray. A skin incision for distal window given at appropriate level along the lateral aspect of the humerus after radiological confirmation. Intermuscular space was created between biceps brachii and brachialis. Radial nerve was completely explored from the level it pierced the lateral intermuscular septum to the level where it enters the anterior compartment and protected by gently retracting it laterally while creating the tunnel for plate. An extraperiosteal tunnel was created to connect the two windows. A combination of direct and indirect methods was used to reduce the fracture [5].
Fracture reduction was achieved using traction and gentle manipulation. When needed k wires and bone levers were used proximally to achieve reduction. Image intensifier was used to confirm the reduction before inserting the plate.
Plate was inserted from proximal window taking care of axillary nerve. Image intensifier was used to check the position of plate and fracture reduction before securing with screws proximally and distally [6].
Additional interfragmentary cortical screws were used to improve reduction whenever needed. A final C arm control view was always taken to confirm reduction and correct implant position before wound closure. Post operatively patients were given arm sling support. X ray was taken at first post-operative day. Then patients were assessed at 6 weeks, 3 months, 6 months and 1 year. An Anteroposterior (AP) and lateral view X rays were taken at each follow up visit. Functional assessment with Constant-Murley score and DASH score was done at 1 year [7-9].
Results
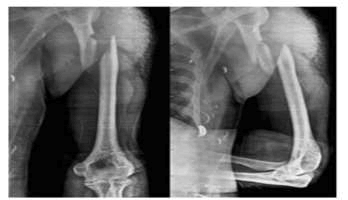
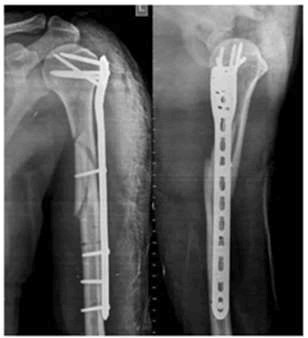
Patients were allowed to do gentle passive range of movement exercise from next day. However active movements were allowed only after 2 weeks. Patients were regularly called for follow up. The average age of the study group was 72.6 years (range 62 to 81 years). Out of 10 patients 8 were females and 2 males. 7 patients had dominant side and 3 had non dominant side fracture (Figures 1 and 2).
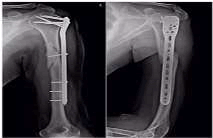
100% union rate was seen by the final follow up. No case of non-union, malunion, infection, radial or axillary nerve injury was seen in any patient. All except one patient achieved pre injury activity level (Figure 3), 1 case had painful restriction of shoulder movement) at final follow up because of slightly proximal plate placement (18 months). The average blood loss observed was 91.5 ml (range: 65 ml-125 ml) (Figures 3 and 4). The average operating time was 60.4 minutes (range: 48 to 82 minutes).
The mean Constant-Murley score was 82.6 and mean DASH score was 23.7 at 1 year follow up. The mean fracture union time was 14.7 weeks and mean follow up period was 20.4 months. All the patients completed at least case 1 year of follow up.
Discussion
Traditionally majority of shaft humerus fractures are managed conservatively. However recent published data has shown significant advantages of operative methods regarding better functional outcome and less non-union rates. Because of fragile bones in elderly complex metadiaphyseal proximal humerus fractures need prolonged immobilization which can have profound negative impact on the quality of life. Open reduction internal fixation with plating using deltopectoral approach is the most commonly used surgical method for proximal humerus fractures. James et al found satisfactory results with open reduction and internal fixation with plating for complex metadiaphyseal proximal humerus fractures. However many studies have shown complications because of extensive soft tissue stripping and vascular like avascular necrosis, infection, non-union and radial nerve injury varying from 17% to 35%. In elderly people with osteoporosis and underlying co morbidities chances of infection and implant breakage are more with open methods.
We didn’t report any case of non-union, infection, malunion, implant breakage or avascular necrosis. Antegrade intramedullary nailing is a minimally invasive method where fracture site usually is not exposed. However Garnavos et al reported complications like loss of reduction, failure of closed reduction, difficulty in distal locking, more radiation exposure and persistent shoulder pain in 60% of patients above 65 years of age with proximal metadiaphyseal fractures. We didn’t report any case of loss of reduction in the follow up. Only one case in our study ended up with restricted shoulder movements. MIPO technique with long PHILOS plate is a very good alternative for metadiaphyseal fractures inelderly. Being a tissue sparing surgery complications of open plating and nailing are taken care of. However surgical experience and adequate knowledge of neurovascular structures is essential for good outcome. Hohman et al in their study observed significant advantages with MIPO technique over open plating and nailing for humerus fractures. Incidence of non-union, infection rate, nerve injuries, shoulder stiffnes and need of revision surgeries was low in MIPO method as compared to other methods [10]. We didn’t report any case of infection, nerve injury or non-union in our study group. A number of studies have shown excellent results with MIPO plating for humerus shaft and proximal humerus fractures with both PHILOS and helical plating. Our results regarding average blood loss and average fracture union time were consistent with their findings. Jeong et al in their study have shown advantages of long PHILOS plate over narrow Locking compression plate for spiral humerus shaft fractures.
There are very few studies of MIPO plating for complex metadiaphyseal proximal humerus fractures in geriatric patients. Seyfattingulo et al observed 100% union rate, 2 cases of shoulder impingement and 2 cases of radial nerve palsy I their 24 elderly patient with proximal metadiaphyseal proximal humerus fractures. The findings regarding patient demographics, union rate, mean Constant-Murley_score and mean DASH score at 1 year follow up were consistent with our study. The drawback of MIPO plating with deltoid splitting approach proximally is risk of injury to axillary nerve. We didn’t observe any case of axillary nerve damage in our study. We didn’t fully expose the axillary nerve. First digital palpation of the nerve was done and gentle finger dissection was done to make the space beneath the nerve. Zou et al studied results of MIPO plating with philos plate through deltopectoral approach for proximal humerus fractures and observed satisfactory results. Lau et al reported radial nerve injury in 17% cases in their study and attributed it to forceful traction of the nerve while placing plate on lateral surface of humerus. We didn’t observe any case of radial nerve injury because careful exploration and gentle retraction of the nerve was done before placing the plate.
Conclusion
Some of the recent studies have recommended anterior distal window and anterior distal contouring for long PHILOS plate during MIPO technique to prevent radial nerve damage. However musculocutaneous nerve is at risk between while splitting brachialis muscle during anterior window formation. Wang et al recommended precountoring of locking philos plates on 3D printed models to prevent radial nerve damage. We used lateral distal window in all the patients and no anterior contouring was done in any of the philos plate. With indirect reduction in MIPO plating some degree of rotational deviation is expected in proximal humerus fractures. Zamboni et al observed that some degree of retroversion was observed in all the cases of MIPO plating for proximal humerus fractures but all the cases had good to excellent functional results. All except one case in our study had excellent functional outcome in our study. Ball and socket shoulder joint compensates for rotational deviation at fracture site. Small sample size and no control group is the limitation of our study. Randomized controlled trials of sample sizes are needed for more reliable results.
Conflict of Interest
None.
Financial Support
None.
Author’s Contribution
TAB has done the conception and design of the study and the writing and final approval of the manuscript. MS was involved in manuscript writing and in its critical revision and final approval. All the authors read and approved the final manuscript.
References
- Court-Brown CM, Caesar B. Epidemiology of adult fractures: A review. Injury. 2006; 37:691-697. [Crossref] [Google Scholar] [PubMed]
- Nguyen TV, Center JR, Sambrook PN, et al. Risk factors for proximal humerus, forearm and wrist fractures in elderly men and women: The Dubbo osteoporosis epidemiology study. Am J Epidemiol. 2001; 153:587-595. [Crossref] [Google Scholar] [PubMed]
- Bhandari M, Devereaux PJ, McKee MD, et al. Compression plating versus intramedullary nailing of humeral shaft fractures-a meta-analysis. Acta Orthopaedica. 2006; 77:279-284. [Crossref] [Google Scholar] [PubMed]
- Petsatodes G, Karataglis D, Papadopoulos P, et al. Antegrade interlocking nailing of humeral shaft fractures. J Orthopaedic Sci. 2004; 9:247-252. [Crossref] [Google Scholar] [PubMed]
- Brunner F, Sommer C, Bahrs C, et al. Open reduction and internal fixation of proximal humerus fractures using a proximal humeral locked plate: A prospective multicenter analysis. J Orthopaedic Trauma. 2009; 23:163-172. [Crossref] [Google Scholar] [PubMed]
- Handoll HH, Brorson S. Interventions for treating proximal humeral fractures in adults. Cochrane Database Syst Rev. 2015; 11:434. [Crossref] [Google Scholar] [PubMed]
- James IB, Farrell DJ, Evans AR, et al. Open reconstruction of complex proximal metadiaphyseal fragility fractures of the humerus. Geriatric Orthopae Surg Rehab. 2014; 5:9-13. [Crossref] [Google Scholar] [PubMed]
- Meier RA, Messmer P, Regazzoni P, et al. Unexpected high complication rate following internal fixation of unstable proximal humerus fractures with an angled blade plate. J Orthopaedic Trauma. 2006; 20:253-260. [Crossref] [Google Scholar] [PubMed]
- Jain NP, Mannan SS, Dharmarajan R, et al. Tuberosity healing after reverse shoulder arthroplasty for complex proximal humeral fractures in elderly patients-does it improve outcomes? A systematic review and meta-analysis. J Shoulder Elbow Surg. 2019; 28:78-91. [Crossref] [Google Scholar] [PubMed]
- Apivatthakakul T, Arpornchayanon O, Bavornratanavech S. Minimally Invasive Plate Osteosynthesis (MIPO) of the humeral shaft fracture. Is it possible? A cadaveric study and preliminary report. Injury. 2005; 36:530-538. [Crossref] [Google Scholar] [PubMed]




 Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.
Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.