Evaluation of treatment of thoraco-lumbar flexion distraction injuries by percutaneous transpedicular screw instrumentation : a prospective study
2 Department of Orthopaedics, RG Kar Medical College & Hospital, Kolkata, India
Received: 05-Jan-2023, Manuscript No. jotsrr-23- 85627; Editor assigned: 07-Jan-2023, Pre QC No. jotsrr-23- 85627 (PQ); Accepted Date: Jan 16, 2023 ; Reviewed: 10-Jan-2023 QC No. jotsrr-23- 85627 (Q); Revised: 14-Jan-2023, Manuscript No. jotsrr-23- 85627 (R); Published: 19-Jan-2023
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Introduction
Flexion-distraction injuries occur due to distractive forces leading to disruption of the posterior and middle columns of the spine [1]. These injuries are frequently associated with anterior column injuries such as compression fractures, often leading to further instability or kyphosis [2]. These injuries are also frequently associated with neurodeficit due to canal compromise and ab dominal injuries [2]. This fracture pattern was first classified by Chance, who originally described a flexion injury to the vertebrae resulting in disruption of the posterior arch system [3]. These fractures classically consist of a fracture line through the spinous process, laminae, transverse processes, pedicles, and into the vertebral body (Fig. 1), but involvement of soft tissues, such as the posterior Ligamentous complex, is very common (Fig. 2) [4, 5]. The most common location for a flexion-distraction injury is around the thoracolumbar junction, although it can occur at any level of the spine [6]. Flexiondistraction injuries account for 1%–16% of all thoracolumbar fractures, depending on the population examined [7].
Treatment of flexion-distraction injuries often requires surgical fixation and fusion if there is damage to the posterior ligamentous complex, as the associated ligaments heal poorly despite reduction and prolonged immobilization, and conservative management often results in significant kyphotic deformity and neurological deterioration [1, 4].
More recently, minimally invasive techniques have gained traction due to advantages with regard to minimizing paraspinal tissue damage during the approach, leading to decrease in blood loss, operative time, and use of postoperative analgesics [5, 8]. Minimally invasive percutaneous instrumentation is a viable option for selective unstable fractures that do not require open reduction or open decompression of the neural elements. There have been relatively few reports of percutaneous pedicle screw fixation for flexion distraction injuries in the literature, and reports are mostly oriented regarding bony injuries and its healing [5, 9].
We would like to describe the outcome of our patients with flexiondistraction thoracolumbar injury treated with minimally invasive pedicle screw fixation in last three years.
Materials and Methods
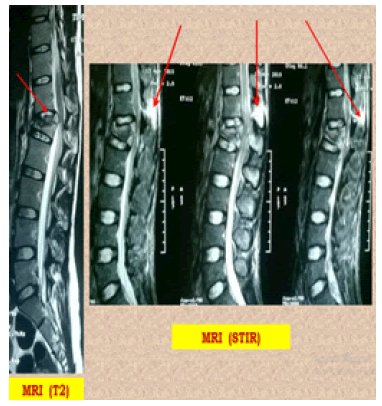
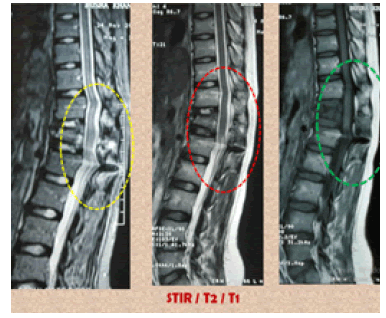
Patients with flexion-distraction injury who were treated between Jan 2017 and May 2019 were followed up prospectively. Neurological status was determined using the ASIA scoring system, which is based on the modified Frankel score on admission as well as at each follow-up visit [10]. The degree of kyphotic angulation, or Cobb angle, was measured from lateral radiographs using the cephalad and caudal intact endplates on admission, at discharge, and at each follow-up visit. The residual canal was based on the AP diameter of the canal at the site of injury, expressed as a percentage of the average AP diameter at the intact levels cephalad and caudal to the level of the injury. Injuries were classified using the AO classification as well as the TLICS for thoracolumbar injuries [11]. Total operative time and length of hospital stay were noted. In postoperative period, apart from Cobb angle, incidence of violation of the medial wall of pedicle and abutment of cephalad joint were also noted. Healing of PLC was noted at postoperative MRI (3 months follow-up) on both T1 & STIR sequence. Functional assessments were done by measuring VAS & ODI score in both preoperative and post-operative follow-up periods. Patients with neurological deficit, with other associated injuries and patients with less than one-year follow-up were excluded from this study.
Results
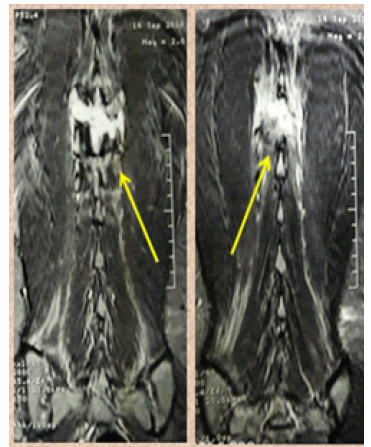
A total of 12 patients (9 males, 3 female) with flexion- distraction injury were treated at our institution by Minimally Invasive Pedicle screw fixation (MIPS) in prone position between Jan 2017 and May 2019. The average age of all 12 patients was 26 years (range 14 years-56 years). The mechanism of injury in most of them was road traffic accidents except in two female patients who had injuries during contact sports. In all cases, non-contrast MRI demonstrated injury to some portion of the posterior Ligamentous complex (Fig. 3) as bright hyper-intensity signal. The levels of injury ranged from T-6 to L-3. The most commonly injured level was L-1 (6 cases). The average residual canal after injury was 90% (range 86%–100%).
All except two cases were operated within 3 days of admission. In 7 cases, fusion construct were restricted to one segment above and below the index level, with a unilateral or bilateral pedicle screw inserted in the index level. In rest of the cases, construct was extended up to two cephalad & caudal levels. No patient showed neurological deterioration in post-operative period. Total operative time in average was 66 minutes (range 45 min-120 min). Duration of hospital stay in average was 5 days (average 3 days-8 days). With experience, operative time gradually decreased, though it is basically related with the length of instrumentation.
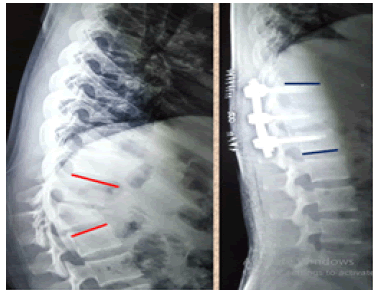
The average kyphotic angulation at admission was 8 degrees (2°-10°), which improved significantly to 2.5° (1.5°-6°) (Fig. 4). A total of 80 MIPS were evaluated on CT. Among them only 5 screws showed Grade II violation. No incidence of Grade III or higher violation was noted. Among the 24 proximal facet joints, only five joints had Grade II violation, none higher. On routine postoperative MRI assessment at 4 months, all cases showed near complete healing of posterior ligament complex in T1 sequence and complete absence of hyper intensity signal in STIR sequence (Fig. 5).
The pain profile during the first 7 postoperative days has been reflected by VAS scores; average 2.6 [1-4]. Working ability was assessed as the capacity of the patients to return to their previous working position. In our study, every patient had resumed their full working capacity in due course of time. Heavy weight lifting and contact sports were restrained until the radiological signs of PLC healing are clearly evident. No incidence of superficial or deep infection, CSF leakage, vascular and visceral injury happened. No need for hardware removal in any of the cases until last follow-up.
Discussion
Although Percutaneous Transpedicular Fixation is currently been using for thoracolumbar fractures, a number of articles have cited few drawbacks of this technique, such as a reduced angular stability of the polyaxial screws, lesser potential to correct kyphotic deformity, suboptimal condition for spinal fusion, and the fact that the majority of such systems can provide only short-segment fixation [12]. Although the initial results with short-segment fixation in thoracolumbar trauma cases were dismal, showing mechanical failure in as many as 50% of patients, currently the general consensus about the suitability of this therapeutic approach is that it is acceptable in preselected patient groups [13]. Therefore, most of the literature suggests that this procedure should be performed with no inter-segmental fusion in patients with supposedly favourable bone healing potential and in the absence of significant ligamentous instability [unstable burst-type fractures (AO/ Magerl Type A3 classification) without severe kyphotic deformity] [14, 15].
With a very few literatures support on implementation of MIPS in flexion-distraction spine injury (AO/Magerl Type B1 & B2 classification), we have experienced a promising result on clinical, radiological and functional outcome in our study [5, 9, 16]. No evidence of statistically significant increase in Kyphotic angle in any of the cases till last followup have been detected.
Some authors advocate polymethylmethacrylate augmentation of percutaneous transpedicular screws with or without kyphoplasty of fractured vertebrae in patients without osteoporosis [17]. We do not find this concept to be useful in patients with normal bone supply because screw anchoring appeared to be adequate and sufficient, according to our results. In our opinion, polymethylmethacrylate augmentation only increases the potential risk of perioperative complications. Furthermore, there are no published data to clarify the potential longterm consequences of bone cement placed into the vertebral body, and speculation about interference with the natural vertebral body healing process might be correct [18].
In our study only five screws out of eighty (6.25%) had radiologically significant medial cortical pedicular breech. The ratio is well below than the similar literatures [19,20]. In 58.3% cases (7/12), we restricted our instrumentation to one level around the index segment. As per JS Uribe et al, short-segment fixation (one level above and below the fracture) with a short screw (25mm -35 mm in length) through the pedicle at the index level provides substantial biomechanical support to allow for appropriate healing [21]. Compromise of the pedicle(s) may prohibit placement of an index level screw. Likewise, compromised bone integrity at an adjacent level may warrant extension to an additional level to ensure appropriate purchase [22]. Percutaneous methods do not allow direct decompression of neural elements. However, indirect decompressions in these cases were achieved by both positioning of the patient in prone and by the ligamentotaxis principle along the screws. For many burst fractures, prone placement of the patient on the operating room bed causes postural reduction of the traumatic deformity and Distraction across the fractured segment allowed for ligamentotaxis and anterior stretching of the retropulsed bone fragment, thereby decreasing canal encroachment [21].
Removal of instrumentation after healing of the injured segments is an option, and removal serves to preserve the patient’s motion segments. In our practice, if a patient is not having postoperative pain, hardware failure, or prominence of their hardware, we usually feel that they would not benefit from an additional procedure to remove the instrumentation. If these problems do occur, a discussion is held with the patient regarding hardware removal. However, timing of instrumentation removal is less clear-cut in the cases of ligamentous injury than in cases of primarily osseous injury, but removal is not recommended prior to at least 1 year in the case of ligamentous injury
To our knowledge, there have been very few reports of percutaneous pedicle screw instrumentation for treatment of flexion-distraction injuries with a disrupted posterior ligamentous injury component [5,9,16]. No study has so far documented the healing of PLC in postoperative MRI (T1 & STIR) when most of them had documented the bony healing only in CT scans. Therefore, although promising, given the relative paucity of long-term data regarding MIS procedures as a treatment for flexion-distraction injuries, no definitive conclusions can be made; however, minimally invasive fixation should be considered as a viable and effective option.
Conclusion
Flexion-distraction injuries with disrupted PLC & without neurodeficit can be effectively treated by minimally invasive pedicle screw fixation which restores adequate stability and sufficient neural decompression. Associated benefits like reduction in blood loss and hospital stay leads to quicker rehabilitation which ultimately improves functional outcome. However, further studies are needed to assess the long-term outcome of patients treated with percutaneous pedicle screw fixation compared with traditional open instrumented fusion techniques.
References
- Denis F. The three column spine and its significance in the classification of acute thoracolumbar spinal injuries. Spine. 1983 8(8):817-31. [Google Scholar]
[CrossRef]
- Vaccaro AR, Lehman Jr RA, Hurlbert RJ, et al. A new classification of thoracolumbar injuries: the importance of injury morphology, the integrity of the posterior ligamentous complex, and neurologic status. Spine. 2005; 30(20):2325-2333. [Google Scholar]
[CrossRef]
- Chance GQ. Note on a type of flexion fracture of the spine. Br J Radiol. 1948; 21(249):452-453. [Google Scholar]
[CrossRef]
- Liu YJ, Chang MC, Wang ST,et al. Flexion–distraction injury of the thoracolumbar spine. Injury. 2003; 34(12):920-923. [Google Scholar]
[CrossRef]
- Schizas C, Kosmopoulos V. Percutaneous surgical treatment of Chance fractures using cannulated pedicle screws: report of two cases. J Neurosurg: Spine. 2007; 7(1):71-74. [Google Schola]
[CrossRef]
- Chapman JR, Agel J, Jurkovich GJ, et al. Thoracolumbar flexion-distraction injuries: associated morbidity and neurological outcomes. Spine. 2008; 33(6):648-657. [Google Scholar]
[CrossRef]
- Patel AA, Vaccaro AR, Albert TJ, et al. The adoption of a new classification system: time-dependent variation in interobserver reliability of the thoracolumbar injury severity score classification system. Spine. 2007; 32(3):E105-110. [Google Scholar]
[CrossRef]
- Kim DY, Lee SH, Chung SK, et al. Comparison of Multifidus Muscle Atrophy and Trunk Extension Muscle Strength: Percutaneous: Versus: Open Pedicle Screw Fixation. Spine. 2005; 30(1):123-129. [Google Scholar]
[CrossRef]
- Beringer W, Potts E, Khairi S, et al: Percutaneous pedicle screw instrumentation for temporary internal bracing of nondisplaced bony Chance fractures. J Spinal Disord Tech 20:242–247, 2007. [Google Scholar]
[CrossRef]
- Frankel HL, Hancock DO, Hyslop G, et al: The value of postural reduction in the initial management of closed injuries of the spine with paraplegia and tetraplegia. I. Paraplegia 7:179–192, 1969. [Google Scholar]
[CrossRef]
- Bono CM, Vaccaro AR, Hurlbert RJ, et al. Validating a newly proposed classification system for thoracolumbar spine trauma: looking to the future of the thoracolumbar injury classification and severity score. J orthop trauma. 2006; 20(8):567-572. [Google Scholar]
[CrossRef]
- Fan SW, Hu ZJ, Fang XQ, et al. Comparison of paraspinal muscle injury in one‐level lumbar posterior inter‐body fusion: modified minimally invasive and traditional open approaches. Orthopaedic surgery. 2010; 2(3):194-200. [Google Scholar]
[CrossRef]
- Zdeblick TA, Sasso RC, Vaccaro AR, et al. Surgical treatment of thoracolumbar fractures. Instr Course Lect. 2009; 58:639-644. [Google Scholar]
- Yang H, Shi JH, Ebraheim M, et al. Outcome of thoracolumbar burst fractures treated with indirect reduction and fixation without fusion. Eur Spine J. 2011; 20(3):380-386. [Google Scholar]
[CrossRef]
- Vanek P, Bradac O, Konopkova R, et al. Treatment of thoracolumbar trauma by short-segment percutaneous transpedicular screw instrumentation: prospective comparative study with a minimum 2-year follow-up. Journal of Neurosurgery: Spine. 2014; 20(2):150-156. [Google Scholar]
[CrossRef]
- Grossbach AJ, Dahdaleh NS, Abel TJ, et al. Flexion-distraction injuries of the thoracolumbar spine: open fusion versus percutaneous pedicle screw fixation. Neurosurgical focus. 2013; 35(2):E2. [Google Schola][CrossRef]
- Rahamimov N, Mulla H, Shani A, et al. Percutaneous augmented instrumentation of unstable thoracolumbar burst fractures. European Spine Journal. 2012; 21(5):850-854. [Google Scholar][CrossRef]
- Kim KH, Kuh SU, Park JY, et al. What is the importance of “halo” phenomenon around bone cement following vertebral augmentation for osteoporotic compression fracture? Osteoporosis International. 2012; 23(10):2559-2565. [Google Scholar]
[CrossRef]
- Raley DA, Mobbs RJ. Retrospective computed tomography scan analysis of percutaneously inserted pedicle screws for posterior transpedicular stabilization of the thoracic and lumbar spine: accuracy and complication rates. Spine. 2012; 37(12):1092-1100. [Google Scholar]
[CrossRef]
- Smith ZA, Sugimoto K, Lawton CD, et al. Incidence of lumbar spine pedicle breach after percutaneous screw fixation: a radiographic evaluation of 601 screws in 151 patients. Clinical Spine Surgery. 2014; 27(7):358-363. [Google Scholar]
[CrossRef]
- Walker CT, Xu DS, Godzik J, et al. Minimally invasive surgery for thoracolumbar spinal trauma. Annals of translational medicine. 2018; 6(6). [Google Scholar]
[CrossRef]
- Tezeren G, Bulut O, Tukenmez M, et al. Long segment instrumentation of thoracolumbar burst fracture: fusion versus nonfusion. Journal of back and musculoskeletal rehabilitation. 2009; 22(2):107-112. [Google Scholar]
[CrossRef]




 Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.
Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.