Fluoroscopic guided close reduction and percutaneous k-wire fixation of paediatric proximal humeral fractures
2 Department of Orthopedics, Government Medical College Srinagar, Jammu and Kashmir, India
Received: 20-Jul-2013 Accepted Date: Aug 20, 2023 ; Published: 20-Aug-2028
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: Paediatric proximal humeral fractures, relatively rare injuries are often managed conservatively. In adolescent patients owing to less remodelling potential of fracture site with residual gross angulation and deformity, surgical reduction and fixation is increasingly advocated. However, controversy continues regarding ideal fixation techniques of these fractures. With the ease of application and preventable minor complications, closed reduction and percutaneous k-wire fixation is probably the better option available.
Materials and methods: This was a prospective study in tertiary hospital from 2013 to 2015 comprising of 18 patients treated by closed reduction and percutaneous k-wire fixation under fluoroscopic guidance. Most common cause of fracture was fall from height and male patients predominated the study. Most of the cases were Salter- Harris type II and Neer Horowitz type IV injuries.
Results: With a mean follow-up of 1.8 years, average healing was observed at 6 weeks. Eighty percent of cases were excellent and none as poor. Four patients developed superficial pin tract infection and none deep infection. There was no case of postoperative neurovascular deficit.
Conclusion: Closed reduction under fluoroscopic guidance with percutaneous k-wire fixation is safe, effective, reliable, reproducible and economical method of proximal humeral fractures
Keywords
Paediatric, Humeral fractures, Salter-Harris type II, Neurovascular
Introduction
Proximal humeral fractures represent 4% to 5% of total fractures, 1% of all paediatric fractures and 3% to 6% of total epiphyseal injuries [1,2]. Proximal humeral physis contributes 80% of humeral longitudinal growth as a result of that has tremendous potential for remodeling [3]. Displacement is absent in 40% of metaphyseal fractures while it is present in 85% of epiphyseal injuries. The displacement in adolescent and early adult’s due to limited growth potential left have chances of residual deformities and cosmetic problems [4,5]. Owing to this concern surgeons recently started recommending operative reduction and fixation of these fracturs [6,7].
Most often reduction is achieved by closed reduction except in rare cases of soft tissue entrapment when open reduction has to be performed. Biceps tendon gets entrapped only after 100 percent anterior displacement of distal shaft fragment in epiphyseal injuries and likewise, the distal fragment may get buttonholed through the capsule, periosteum into muscles necessitating open reduction [8]. As a result of this these fractures are amenable to closed reduction with or without joystick technique. After successful reduction, methods of fracture fixation include k-wire (Kirschner wire), screws, staples and plates [9-12]. Closed reduction and percutaneous k-wire fixation is easy, reproducible, with the acceptable outcome, became the basis of this prospective study.
Materials and Methods
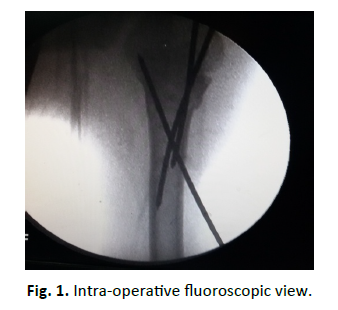
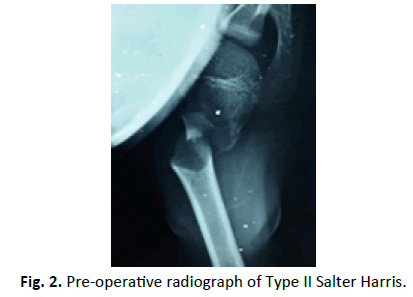
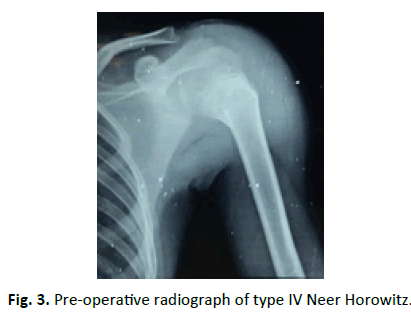
This was a prospective study of patients with open proximal humeral physis with displaced fractures, treated by closed reduction and k-wire fixation. The aim of the study was the clinical outcome of paediatric proximal humeral fractures by closed reduction and percutaneous k-wire fixation. The patients were admitted between May 2013 to July 2015. There were 18 patients with 12 males and 6 females with the Left-sided injury in 10 patients and right-sided in 8 patients. Most common mechanism of injury was fall (fall from trees, while playing, fall from a window) followed by road traffic accidents. All the patients included in this study were closed injuries. Fifteen patients had Salter-Harris type II, 2 type I and 1 type III injuries, and as per Neer Horowitz system of classification 12 were type IV, 4 type III and 2 type II [13,14]. None of the patients had any neurovascular deficit at the time of presentation. Three patients had abrasion over shoulder due to trauma (Fig. 1).
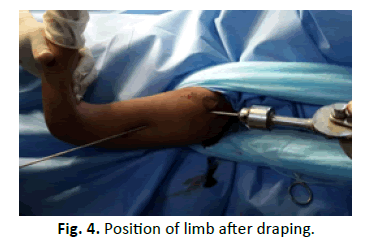
After radiographic evaluation (Fig. 2 and 3) treatment modalities were explaining to the attendants (parents), written informed consent was taken and patients were prepared for surgery. Routine biochemistry and serological investigation were done and patients admitted during the day were shifted to operation room for closed reduction and k-wire fixation in the emergency operation theatre. In the Operation room patients were positioned supine on the radiolucent table with the facility of Fluoroscopy Fig. 3 and 4. After anaesthesia (preferably general anaesthesia), the patient was draped with whole upper extremity free for reduction and manipulation during fixation. Closed reduction was achieved by abduction, forward flexion and external rotation. Being satisfied with reduction, percutaneous k-wire fixation was started from the lateral aspect of distal fragment well below the anticipated level of axillary nerve Fig. 1. This was supplemented by one more k-wire for additional strength. Finally, k-wire was passed from proximal fragment just outside articular surface towards medial cortex of distal fragment and increasing no. of k-wires for additional strength as desired Fig. 4. In cases when simple traction and counter traction was not effective for reduction, k-wires inserted in fracture fragments were utilized as joysticks for manipulation and one of the k-wires was advanced to achieve fixation, followed by routine fixation technique. None of the patients was open reduced after joystick manipulation (8 patients). k-wires were cut outside the skin bent and dressing done. Immobilisation of limb was done by arm chest sling for 3 weeks thereafter progressive physiotherapy was started beginning with pendulum exercises, k-wires were removed after 6 weeks on outpatient basis Fig. 5.
Results
The age group of patients was 8-16 years, with the average age of 12 years. Mean radiographic angulation of about 50°. All the fractures were reduced within 3 days after trauma and on the same day of hospital admission except 3 patients, which needed initial stabilisation (one had associated blunt trauma abdomen, 2 neurosurgical referrals for loss of consciousness after trauma, were treated on the 3rd day after surgical clearance). The average Constant score was 92 (68-100) [15]. The mean follows up was 1.8 years with a minimum follow-up of one year. Average radiological healing was achieved at 6 weeks (4 to 10 weeks). The 80% of patient had excellent results, 20% as good and fair and none poor as per constant Score. 4 patients developed superficial pin tract infection which included erythema with tenderness in 2 cases, discharge around the pin in 2 patients but no loosening of pins. Infection subsided with Oral antibiotics (Co-amoxiclav) for 5 days. None of the patients had shoulder stiffness. There was no neurovascular injury reported during the postoperative period.
Discussion
There is favourable consensus for the nonoperative management of proximal humeral fractures in children and adolescents owing to remarkable potential of remodeling and the wide range of motion of shoulder joint [2,16]. However, as the child reaches adolescence nearing skeletal maturity, this remodeling potential decreases considerably with the reported remodeling of correction less than 20 degrees after 11 years [5]. Pahlavan et al. in systemic review of 14 studies (1960-2010) on operative and non-operative treatment of paediatric proximal humeral fractures based on conflicting results suggested age-based criteria for treatment. The age groups being up to 10 years, 10-13 years and more than 13 years, and the recommendation being immobilisation without a reduction in younger age groups and reduction with surgical stabilisation in higher age groups while in intermediate group decision is made on a case to case basis depending on extent of displacement and setting [17]. initially, Beaty recommended reduction regardless of fixation in patients < 5 yrs age with 100% translation and >70° and >10 years ago 50% translation and >40°angulation while in 5-10 age group translation 50% and angulation age dependent [18]. In 2014 Lefervea et al. recommended reduction based on age as. Up to 10 years 100% translation or >70° angulation, 10-13 years 50% translation or >40 angulation and >13 years>30% translation or >20 angulation [4]. In older children and adolescents displaced and angulated fractures deserve reduction and fixation, for favourable early mobilisation and functional recovery. Closed reduction (sometimes limited open reduction) and percutaneous k-wire fixation is a reliable method of reduction, as well as fixation of these fractures with less invasive nature of the surgery, prevent additional soft tissue damage and avascular necrosis of humeral head [19]. Percutaneous k-wire fixation is accepted and reliable alternative to operative reduction and intramedullary and plate fixation [9,20]. Whereas in open reduction there is added injury to soft tissue, risk for neurovascular injury and compromise of vascularity of epiphysis, there is no added benefit for intramedullary flexible nailing in which most of the times open reduction is needed, with duration of surgery more and overall cost many times higher than the simple k-wire fixation [21-23]. The only disadvantage attributed with k-wire fixation is superficial pin tract infection which most of the times is easily manageable without compromising functional outcome [4,9,12,19,23]. Even comparison of k-wire burying under the skin was not found more beneficial than simply bending wire and keeping outside the skin which facilitates easy removal on OPD basis [23]. However, there is still need for safe corridors for percutaneous pin placement in children [24] and randomized control studies for comparison between flexible nailing and k-wire fixation. The limitation of this study is adequate muscle relaxation needed for reduction and subsequent effects of anesthesia on the child, chances of migration of smooth wires, superficial pin tract infection and limited data on k-wires in proximal humeral paediatric fractures.
Conclusion
Closed reduction and k-wire fixation is an easy, reliable, safe and reproducible way of management of adolescent paediatric proximal humeral fractures applicable in almost all nations developed or developing with easy post-reduction immobilisation and rehabilitation with satisfactory outcome results.
REFERENCES
- Aggarwal S., Bali K., Dhillon M.S., et al:. Displaced proximal humeral fractures: an Indian experience with locking plates. J Orthop Surg. 2010;5:60-67.
- Bishop J.Y., Flatow E.L.: Pediatric shoulder trauma. ClinOrthopRelat Res. 2005;432:41-48.
- Pritchett J.W. Growth and prediction of growth in the upper extremity. J Bone Joint Surg Am. 1988;70:520-525.
- Lefevrea Y., Journeaub P., Angelliaumea A., et al.: Proximal humerus fractures in children and adolescents Orthopaedics& Traumatology: Surgery & Research. 2014;100:S149-S156.
- Dameron TB., Reibel D.B.: Fractures involving the proximal humeral epiphyseal plate. J Bone Joint Surg Am. 1969;51:289-297.
- Burgos-Flores J., Gonzalez-Herranz P., Lopez-Mondejar J.A., et al.: Fractures of the proximal humeral epiphysis. IntOrthop. 1993;17:16-19.
- Bahrs C., Zipplies S., Ochs B.G., et al.: Proximal humeral fractures in children and adolescents. J PediatrOrthop. 2009;29:238-242.
- Visser J.D., Rietberg M.: Interposition of the tendon of the long head of the biceps in fracture-separation of the proximal humeral epiphysis. Neth J Surg. 1980;32:12-15.
- Chen C.Y., Chao E.K.: Closed management and percutaneous fixation of unstable proximal humerus fractures. J Trauma. 1998;45:1039-1045.
- Jaberg H., Warner J.J.P., Jakob R.P. Percutaneous stabilization of unstable fractures of the humerus. J Bone Joint Surg. 1992;74-A:508-515.
- Naidu S.H., Bixler B., Capo J.T., et al.: Percutaneous pinning of proximal humerus fractures: A biomechanical study. Orthopedics. 1997;20:1073-1076.
- Williams G.R., Wong K.L. Two-part and three-part fractures reduction and internal fixation versus closed reduction and percutaneous pinning. OrthopClin North Am. 2000;31:1-21.
- Neer C.S. II, Horwitz B.S.: Fractures of the proximal humeral epiphysial plate. ClinOrthopRelat Res. 1965;41:24-31.
- Wang Jr P., Koval K.J., Lehman W., et al.: Salter-Harris type III fracture-dislocation of the proximal humerus. J PediatrOrthopB. 1997;6:219-22.
- Constant C.R., Murley A.H.G.: A clinical method of functional assessment of shoulder. ClinOrthopRelat Res. 1987;214:160-164.
- David S., Kuhn C., Ekkernkamp A.: ProximaleHumerusfraktur des KindesundAdoleszenten. EinehaüfigüberbehandelteFraktur. Chirurg. 2006;77:827-834.
- Pahlavan S., Baldwin K.D., Pandya N.K., et al. Proximal humerusfractures in the pediatric population: a systematic review. J Child Orthop. 2011;5:187-194.
- Beaty J.H.: Fractures of the proximal humerus and shaft in children. InstrCourseLect. 1992;41:369-372.
- El-Bigawi H., El-Gazzar A., Kandeel W.: Percutaneous fixation for displaced proximal humeral fractures In adolescents and young adults. Egypt Orthop J. 2013;48:229-233.
- Soete P.J., Clayson P.E.: Transitory percutaneous pinning in fractures of the proximal humerus. J Shoulder Elbow Surg. 1999;8:569-573.
- Xie F., Wang S., Jiao Q., et al.: Minimally invasive treatment for severely displaced proximal humeral fractures in children using titanium elastic nails. J PediatrOrthop. 2011;31:839-846.
- Hutchinson P.H., Bae D.S., Waters P.M.: Intramedullary nailing versus percutaneous pin fixation of pediatric proximal humerus fractures: a comparison of complications and early radiographic results. J PediatrOrthop. 2011;31:617-622.
- Shore B.J., Daniel J.H., Patricia E.M., et al.: Surgical management for displaced pediatric proximal humeral fractures: a cost analysis. Journal of Children's Orthopaedics. 2015;9:55-64.
- Mehin R., Mehin A., Wickham D., et al.: Pinning technique for shoulder fractures in adolescents: computer modeling of percutaneous pinning of proximal humeral fractures. Can J Surg. 2009;52:E222-E228.




 Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.
Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.