Functional outcome of surgical treatment of clavicle non-union
Received: 30-Jun-2020 Accepted Date: Jul 15, 2020 ; Published: 23-Jul-2020
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: Recently, the treatment of non-union of clavicle by using compressive locked plate internal fixation with bone graft is to improve the healing process without any complications. This study assessed the functional and radiologic results of fixation by locking compression plate (LC-CDP) with bone graft for the treatment of clavicular non-union.
Methods: A prospective clinical study was conducted. Two-year follow from January 2017 to December 2019 of 14 participants (5 men and 9 women) with age vary from 24 to 40 years. The demographic data, side of the fracture, injury-surgery period, clavicular non-union type, and emerge treatment were recorded. The Disabilities of the Arm, Shoulder, and Hand (DASH) score was used. The reduction and provisional fixation by smooth K wires and bone clamp, the anatomical Low-Contact Dynamic Compression Plating (LC-DCP) placed anterosuperior of the clavicle and placed 2-3 screws on both sides of the fracture, cancellous bone harvested from the iliac crest was kept.
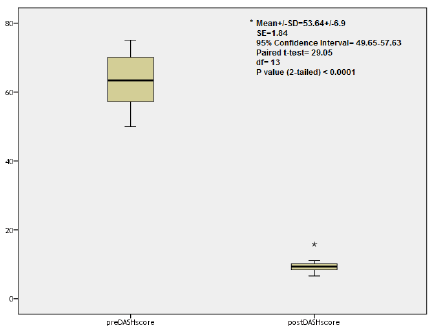
Results: The mean age was 33.79 ± 5.75 years. The left clavicular fracture recorded more than the right side (57.1% vs 42.9%). All patients treated by open reduction and internal fixation by anatomical LC-DCP with iliac crest cancellous bone graft, and all patients committed to following up of 12 months duration. The mean DASH score show improvement from 63.16 ± 7.14 points preoperatively to 9.51 ± 2.19 points postoperatively, which was strongly statistically different (Paired t-test=29.05; 95% CI=49.65-57.63; p<0.0001). Radiographically, all fractures show fully healing and union, with no added complications, were noted.
Conclusion: We concluded that use the anatomical LC-DCP and put 2-3 screws on both sides of the fracture, in addition to cancellous bone harvested from the iliac crest, lead to gain better outcome of completely healing clavicular non-union, with no further complications related to the clavicle and their associated joints.
Keywords
clavicular non-union, clavicle fracture, LC-DCP, DASH score
References
Casino Sites in Germany Blog | Casino Sites in United Kingdom Casino Sites in France Casino Sites in Canada Find Lawyer in in Arizona Blog | Casino Sites in Cyprus Find Lawyer in Michigan Best Betting Sites in Russia Car Insurance in Alabama and Colorado Find Lawyer in Pennsylvania Blog | Casino Sites in Morocco Car Insurance in Nevada Blog | Casino Sites in Nigeria Find Lawyer in Ohio Blog | Casino Sites in Romania Blog | Casino Sites in Turkey Auto Insurance in Canada Car Insurance in Arkansas Blog | Casino Sites in USA Blog | Casino Sites in VenezuelaIntroduction
The displaced fractures of the clavicle shaft non-union occur in 1%- 15%, and the most risk factors include increasing age, displacement, comminution, and female sex [1]. It is the midshaft is the most common site for non-union because of its frequency. Only patients who have sufficient symptoms like functional shoulder impairment and pain should be considered for an operation [2]. It can be disabling and present mainly with pain and limitation of shoulder movement [3- 5]. Schnetzke et al. studied 58 patients with midshaft clavicle fractures and shows variations in the clavicle fracture healing complication and reported different healing patterns of 33% atrophic, 20% hypertrophic, 7% mixed type and 40% delayed fracture healing [6]. In recent years, we have treated non-union of clavicle directly using compressive locked plate internal fixation with bone graft. Based on the evaluation of postoperative symptom relief, functional improvement of the shoulder, clavicle healing, and complications, Chen et al., hypothesized that surgical treatment of clavicle non-union would result in reducing pain level, improve function and promote fracture healing without complications [7].
Materials and Methods
Study design and setting
A prospective clinical study was designed. Two years follow from January 2017 to December 2019 of 14 participants (5 men and 9 women) with age vary from 24 to 40 years of age with deferent types of complicated healing like atrophic, and hypertrophic non-union. Non-union was defined as a lack of both periosteal and endosteal healing response and bridging of the fracture after 6 months. The demographic data, side of the fracture, injury-surgery period, clavicular non-union type, and emerge treatment were recorded. All patients reported shoulder pain and impairment of function affecting daily life activity with radiological evidence of non-union. The treatment is done by open reduction and internal fixation using anatomical LC-DCP and augmentation with a cancellous bone graft from the iliac crest.
Inclusion Criteria
1. Midshaft clavicular non-union lasting more than 6 months
2. Functional shoulder impairment
3. Patient compliant with follow up protocol
Excluded Patients
1. Clavicular non-union less than 6 months
2. No functional impairment
3. Infected non-union, tumors or pathological fractures
4. Non-compliant patient with follow up
Clinical Evaluation
The Disabilities of the Arm, Shoulder, and Hand (DASH) score was used to evaluate the improvement and functional status of each patient before and after a minimum of 12 months after surgery, all patients did X-ray before and after minimum 12 months to evaluate radiological healing.
Surgical Technique
Under general anesthesia, the patients were placed in a supine position and bump inserted between the scapula, an 8-cm incision was made along the clavicle anterosuperior, centered on fracture site. Careful dissection was carried and clavicle stripping of periosteum, and take care from caused injure to the vital structures, removing sclerosis and debridement of bone ends until bleeding bone ends was noticed and opening of the medullary canal was opened by smooth wires, reduction and provisional fixation by smooth K wires and bone clamp, the anatomical Low-Contact Dynamic Compression Plating (LC-DCP) placed anterosuperior of the clavicle and put 2-3 screws on both sides of the fracture, cancellous bone harvested from the iliac crest was put, the wounds were closed by layers and a sterile dressing applied. Postoperative rehabilitation by placing sling for comfort in the early period, Codman exercise was taught to the patients with encouragement to use the arm, and avoid heavy activity with full return to full activity when fracture healing was confirmed typically 2 to 3 months.
Ethical approval and Patients’ Consent
Written informed consent was obtained from all participants. The Medical Ethical Committee at the Abu-Ghraib General Hospital, Baghdad, Iraq, approved this study (code: 00ORTHO52).
Statistical Analysis
The statistical analyses were performed using SPSS software version 24.0 (IBM, NY, US). Paired-sample t-tests were used to compare the DASH scores pre- and post-operative, respectively. The level of significance was set at 95%, and P<0.05 was considered significant.
Results
In this study, the mean age was 33.79 ± 5.75 years; males participated were less than females (35.7% vs 64.3%); the left clavicular fracture recorded more than the right side (57.1% vs 42.9%); the meantime of period of injury-surgery was 7.78 ± 2.05 months with a range from 6 to 12 months; the atrophic type was common as 42.9%, followed by hypertrophic injury as 35.7%; the sling was the commonest emerge treatment used in 12 (85.7%) of patients (Table 1).
| Patient No. | Age (years) | Gender | Side of fracture | Period of injury-surgery (months) | Types of injury | Emerge treatment |
|---|---|---|---|---|---|---|
| 1 | 40 | M | R | 7 | Atrophic | Figure-of-8 maneuver |
| 2 | 29 | F | R | 8.5 | Hypertrophic | Sling |
| 3 | 40 | M | L | 6 | Atrophic | Sling |
| 4 | 36 | F | L | 7 | Atrophic | Sling |
| 5 | 39 | F | R | 6 | Atrophic | Sling |
| 6 | 30 | F | L | 12 | Hypertrophic | Figure-of-8 maneuver |
| 7 | 31 | F | R | 8 | Delayed | Sling |
| 8 | 24 | M | R | 6 | Hypertrophic | Sling |
| 9 | 24 | F | L | 12 | Hypertrophic | Sling |
| 10 | 40 | F | L | 9 | Atrophic | Sling |
| 11 | 31 | M | L | 7.5 | Hypertrophic | Sling |
| 12 | 33 | M | R | 8 | Mixed | Sling |
| 13 | 39 | F | L | 6 | Atrophic | Sling |
| 14 | 37 | F | L | 6 | Mixed | Sling |
Table 1. Patients characters details
According to previously described criteria, all patients treated by open reduction and internal fixation by anatomical LC-DCP with iliac crest cancellous bone graft, all patients committed to following up of 12 Functional outcome of surgical treatment of clavicle non-union months duration, and there was no any missing data or no patients were lost to follow-up (Tables 2 and 3).
| Patient No. | DASH score | Follow-up (months) | Outcome | Union | Complications | |
|---|---|---|---|---|---|---|
| Pre-surgery | Post-surgery | |||||
| 1 | 66.7 | 15.8 | 14 | Fully heal | Yes | None |
| 2 | 62.4 | 8.9 | 14 | Fully heal | Yes | None |
| 3 | 60.1 | 9.2 | 12 | Fully heal | Yes | None |
| 4 | 70.2 | 10.1 | 12 | Fully heal | Yes | None |
| 5 | 70.1 | 8.7 | 13 | Fully heal | Yes | None |
| 6 | 75.1 | 9.8 | 12 | Fully heal | Yes | None |
| 7 | 55 | 6.6 | 12 | Fully heal | Yes | None |
| 8 | 56.5 | 11.1 | 12 | Fully heal | Yes | None |
| 9 | 64.4 | 9.4 | 12 | Fully heal | Yes | None |
| 10 | 60.5 | 10.4 | 12 | Fully heal | Yes | None |
| 11 | 57.2 | 8.4 | 14 | Fully heal | Yes | None |
| 12 | 64.4 | 9.8 | 12 | Fully heal | Yes | None |
| 13 | 71.6 | 7.5 | 13 | Fully heal | Yes | None |
| 14 | 50 | 7.5 | 12 | Fully heal | Yes | None |
Table 2. Clinical assessments of the patients
| No. | % | Mean ± SD (min-max) |
||
|---|---|---|---|---|
| Age | <35 years | 7 | 50 | 33.79 ± 5.75 (24-40) |
| >35 years | 7 | 50 | ||
| Gender | Male | 5 | 35.7 | |
| Female | 9 | 64.3 | ||
| Side of # | Right | 6 | 42.9 | |
| Left | 8 | 57.1 | ||
| Period of injury-surgery | <7 months | 7 | 50 | 7.78 ± 2.05 (6-12) |
| >7 months | 7 | 50 | ||
| Types of injury | Atrophic | 6 | 42.9 | |
| Hypertrophic | 5 | 35.7 | ||
| Delayed | 1 | 7.1 | ||
| Mixed | 2 | 14.3 | ||
| Emerge treatment | Figure-of-8 maneuver | 2 | 14.3 | |
| Sling | 12 | 85.7 | ||
| Preoperative DASH scores | <64 points | 7 | 50 | 63.16 ± 7.14 (50-70.1) |
| >64 points | 7 | 50 | ||
| Postoperative DASH scores | <7 points | 1 | 7.1 | 9.51 ± 2.19 (6.6-15.8) |
| >7 points | 13 | 92.9 | ||
Table 3. Frequencies of the study characters details
The mean DASH score show improvement from 63.16 ± 7.14 (ranged from 50 to 70.1) points preoperatively to 9.51 ± 2.19 (ranged from 6.6 to 15.8) points one year postoperatively, which was strongly statistically difference (Paired t-test=29.05; df=13; 95% CI=49.65-57.63; P<0.0001) (Fig. 1 and Table 3).
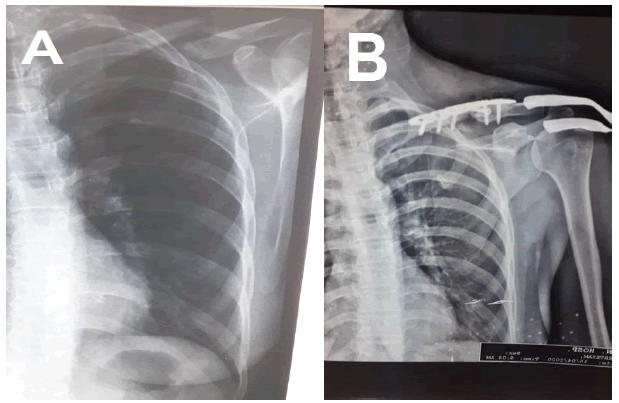
Radiographically recording, all fractures show fully healing and union, with no added complications, was noted at clavicular, acromioclavicular, or sternoclavicular joints, (Fig. 2).
Discussion
Regarding our findings after a one-year follow-up of participants, we noticed that fracture site reduction and stable fixation is a good key procedure for enhancing clavicle union. Whereas there is no agreement on the requirement for bone substitutes in previous literature, which reported that most authors insisted to used bone grafting [8-12].
Here, we placed the anatomical LC-DCP anterosuperior of the clavicle and put 2-3 screws on both sides of the fracture, cancellous bone harvested from the iliac crest was put also, after a one-year followup, we obtained fully heal the fracture, complete union clavicle, and with no added complications related to bone or joints. Schnetzke et al. revealed that bone graft transplantation can result in a significantly shorter time to bone consolidation, better clinical results in terms of the DASH scores, and lower revision rates compared with non-bonegraft transplantation [6]. However, this procedure may not empty from morbidity or complications like graft site infection, pain, and refracture. So far other orthopedic surgeons suggested that bone grafting may be unnecessary in every case of clavicular non-union fracture, and maybe all patients returned to work and regular sports activities as reported by Baker et al. when he fixed clavicular non-union with a pre-contoured locking plate [13].
In a comparison of Dynamic Compression Plating (DCP) in 16 patients and Low-Contact Dynamic Compression Plating (LC-DCP) techniques in 17 patients, Kabak et al. reported that the use of LC-DCP is a more reliable treatment method than the use of the DCP because the LCDCP has several technical advantages that make it an ideal implant for satisfying the unique anatomic and biomechanical requirements of the internal fixation of clavicular non-union and there was an agreement with our findings [14].
In the present study, LC-DCP was used to fix clavicular non-unions and we obtained good outcomes of the fully healing union of all fracture and no further complications related to bone or joints. The LC-DCP offers a low-profile solution for the plating of the clavicle. The titanium plate offers strength, with a rounded profile and a low-profile screwplate interface, which is known to enhance early callus formation [15].
There are many limitations to our study. First, the sample size was small. Second, the calculation of accurate defect size which not determines due to the lack of such facilities to clarify and measure the dimension of the defect and help us to decide whether or not to use the LC-DCP procedure. Third, the follow-up period of one year was relatively short. Fourth, our study is a clinical study and not a case-control study.
Finally, since all the patients didn’t have any complaints after healing as a result no fixation was removed.
Conclusion
Bone resection and fixation using an LC-DCP maneuver without bone graft are effective for the treatment of clavicular non-union without any complications. But when use the anatomical LC-DCP and put 2-3 screws on both sides of the fracture, in addition to cancellous bone harvested from the iliac crest was put, thus gain a better outcome of completely healing clavicular non-union, with no further complications related to the clavicle and their related joints.
Conflict of Interest
No
Funding Support
No
REFERENCES
- Blom A., Warwick D., Whitehouse M.: Apley and Solomon's system of orthopedics and trauma, 10th edition. CRC Press; 2018:757.
- Canale S.T., Beaty J.H., Azar F.M.: Campbell's operative orthopedics, 13th edition. 2017:3110-3111.
- George D.M., McKay B.P., Jaarsma R.L.: The long term outcome of displaced mid third clavicle on scapular and shoulder function: variations between immediate surgery, delayed surgery and nonsurgical management. J Shoulder Elbow Surg. 2015;24:669-676.
- Van der Meijden O.A., Gaskill T.R., Milleyy P.J.: Treatment of clavicle fractures: current concepts review. J Shoulder Elbow Surg. 2012;21:423-429.
- Martetschlaeger F., Gaskill T.R., Millett P.J.: Management of clavicle nonunion and malunion. J Shoulder Elbow Surg. 2013;22:862-868.
- Schnetzke M., Morbitzer C., Aytac S., et al.: Additional bone graft accelerate healing of clavicle nonunion and improves long tern results after 8.9 years. J Orthop Surg Res. 2015;10:2.
- Chen W., Tang K., Tao X, et al.: Clavicular nonunion treated with fixation using locked compression plate without bone graft. J Orthop Surg Res. 2018;13:317.
- Stufkens S.A., Kloen P.: Treatment of midshaft clavicular delayed and nonunions with anteroinferior locking compression plating. Arch Orthop Trauma Surg. 2010;130:159-164.
- Faraud A., Bonnevialle N., Allavena C., et al.: Outcomes from surgical treatment of middle-third clavicle fractures nonunion in adults: A series of 21 cases. Orthop Traumatol Surg Res. 2014;100:171-176.
- O'Connor D., Kutty S., McCabe J.P.: Long-term functional outcome assessment of plate fixation and autogenous bone grafting for clavicular non-union. Injury. 2004;35:575-579.
- Olsen B.S., Vaesel M.T., Sojbjerg J.O.: Treatment of midshaft clavicular nonunion with plate fixation and autologous bone grafting. J Shoulder Elbow Surg. 1995;4:337-344.
- Fuchs B., Steinmann S.P., Bishop A.T.: Free vascularized corticoperiosteal bone graft for the treatment of persistent nonunion of the clavicle. J Shoulder Elbow Surg. 2005;14:264-648.
- Baker J.F., Mullett H.: Clavicle non-union: autologous bone graft is not a necessary augment to internal fixation. Acta Orthop Belg. 2010;76:725-729.
- Kabak S., Halici M., Tuncel M., et al.: Treatment of midclavicular nonunion: Comparison of dynamic compression plating and low-contact dynamic compression plating techniques. J Shoulder Elbow Surg. 2004;13:396-403.
- Khan S.A., Shamshery P., Gupta V., et al.: Locking compression plate in long standing clavicular nonunions with poor bone stock. J Trauma. 2008;64:439-441.



 Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.
Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.