Intramedullary hindfoot fusion as salvage procedure following distal tibia peri-hardware failure in a neuropathic patient: a case report
Received: 27-Dec-2022, Manuscript No. jotsrr-22- 84857; Editor assigned: 28-Dec-2022, Pre QC No. jotsrr-22- 84857(PQ); Accepted Date: Jan 10, 2023 ; Reviewed: 03-Jan-2023 QC No. jotsrr-22- 84857(Q); Revised: 09-Jan-2023, Manuscript No. jotsrr-22- 84857(R); Published: 18-Jan-2023
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: Tibotalocalcaneal arthrodesis is a salvage procedure reserved for severe tibiotalar and subtalar arthritis, hindfoot deformities, failed ankle arthroplasty, talar osteonecrosis, acute trauma, charco arthropathy, and other hindfoot pathologies. Multiple methods are described including intramedullary arthrodesis. We report the use of a long nail for concurrent tibial plateau and shaft fixation and hindfoot fusion in a neuropathic patient who experienced osseous failure at the level of ankle status-post index tibial nailing.
Case Report: A 52-year-old, neuropathic female, previously treated with open reduction and intramedullary fixation for tibial plateau and tibial shaft fractures, respectively, experienced bony failure at the level of the ankle with hardware protrusion through the plafond, abutting the talus. Anterograde intramedullary fixation with an extended nail was used to support her initial tibial shaft and plateau fractures and provide simultaneous salvage hindfoot fusion.
Conclusion: Anterograde intramedullary nailing with a long standard tibial nail is a viable treatment option to provide proximal tibia fixation and hindfoot arthrodesis in neuropathic patients that have experienced distal failure around existing intramedullary hardware.
Keywords
tibiotalocalcaneal arthrodesis, anterograde intramedullary hindfoot arthrodesis, anterograde hindfoot fusion, tibia hardware failure
Introduction
Tibiotalocalcaneal (TTC) arthrodesis is widely accepted as a salvage procedure for a variety of complex hindfoot pathologies. Acute trauma with significant bone loss, post-traumatic, degenerative, and rheumatoid arthritis, Charcot arthropathy, loss, destruction, and Avascular Necrosis (AVN) of the talus, failed ankle arthroplasty or fusion, infection, neuromuscular and congenital deformities, pseudoarthrosis, and tumor resection have all been defined as indications for hindfoot arthrodesis [1-27]. More recently, it has been proposed as an alternative to standard fixation techniques for fragility ankle fractures with poor soft tissue envelope and for neuropathic patients in whom primary ankle fracture fixation has failed [21, 23, 28-30]. Explicit contraindications to TTC fusions are the presence of an active infection and advanced vascular disease. Severe angular deformity of the distal tibia, ankle or hindfoot rendering a well-aligned reduction problematic or a healthy, mobile subtalar joint are relative contraindications [3, 4, 7, 8, 13, 19].
Different methods for successful TTC arthrodesis exist which include the use of Steinmann pins, staples, screws, plates, external fixation, retrograde intramedullary nailing, or combination of internal and external fixation constructs [2-6,8,10-13,15,19,20,22,24]. Intramedullary nailing offers the biomechanical benefit of higher bending stiffness, increased rotational stability, load-sharing capacity, and dynamic compression capabilities [3-5, 7, 8, 10, 20, 22]. One additional benefit is its ability to be performed through minimally invasive technique which may be advantageous in populations at risk for complications such as soft tissue breakdown [13, 19, 21, 23, 24].
Ankle arthrodesis has evolved significantly over the last century, with the earliest description by Lexer in 1906 where boiled corpse bone was passed through the calcaneus, talus, and tibia, a technique known as Bolzungs arthrodese. Albee, in 1915, modified this procedure to incorporate the patient’s own biology by way of autologous fibular spikes. Adams is first credited in 1948 with published data on use of a retrograde metallic nail followed by Leikkonen, Kuntscher, and Bingold who described variations of this in the late 40s and mid-50s. In 1962, Kuntsher detailed tibioltalocalcaneal arthrodesis with use of an unlocked retrograde cone-shaped nail from the calcaneus into the tibia. Intramedullary nails with interlocking screws became available in the early 1990s, and Kile and colleagues in 1994 reported the use of a straight, interlocked intramedullary device, a variation of the Johnson Nail (Smith & Nephew Richards Inc, Memphis TN, USA) [1-3,6-8,11,13,15]. Since that time, nails unintended for TTC arthrodesis have been used including proximal humeral nails used by Hammett and colleagues and femoral nails by Pinzur and Kelikian. [3] Today, companies manufacture nails designed explicitly for TTC arthrodesis, though the use of other nail types continues to be utilized [3, 22-27] .
In this report, we describe what we believe to be the first use of a long tibial nail placed in an anterograde fashion for coinciding tibial plateau and shaft fixation and TTC arthrodesis in a neuropathic patient who experienced bony failure distally around an existing tibial implant.
Case Report
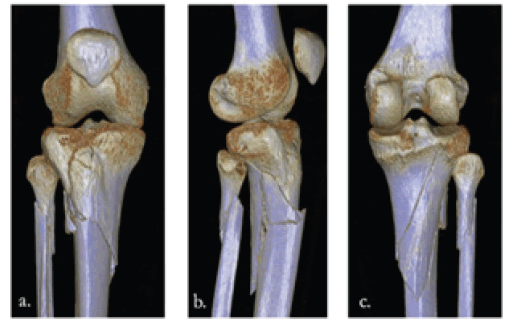
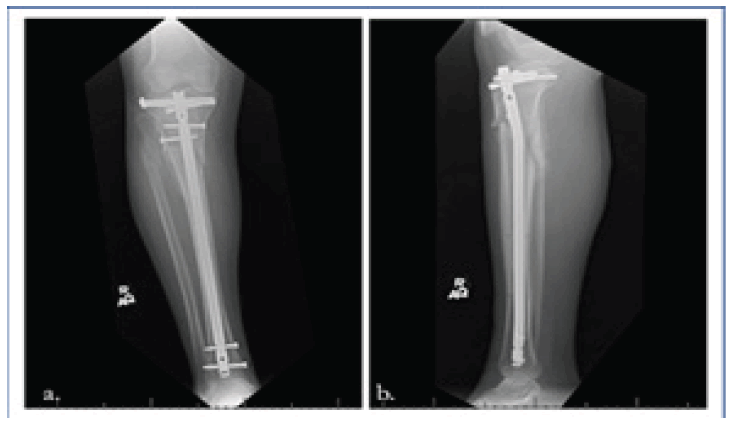
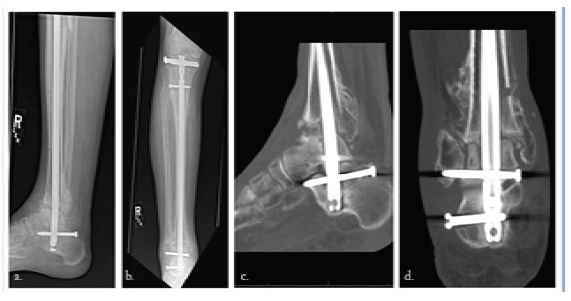
The patient is a 53-year-old neuropathic female with a history of type II diabetes who presented to University of South Alabama Hospital with a right, comminuted tibial shaft fracture and displaced lateral tibial plateau fracture after a ground-level fall in March, 2021 (Fig. 1a, b and Fig.2a, b and c). Soon after presentation, she underwent open reduction and intramedullary fixation of her injurie (Fig. 3a, b).
The patient presented for scheduled routine follow-up visits without complication. At her six-week follow-up visit in late April, 2021, radiographs demonstrated favorable callus formation at her fracture sites. She was advised to slowly advance to weight-bearing as tolerated at this time.
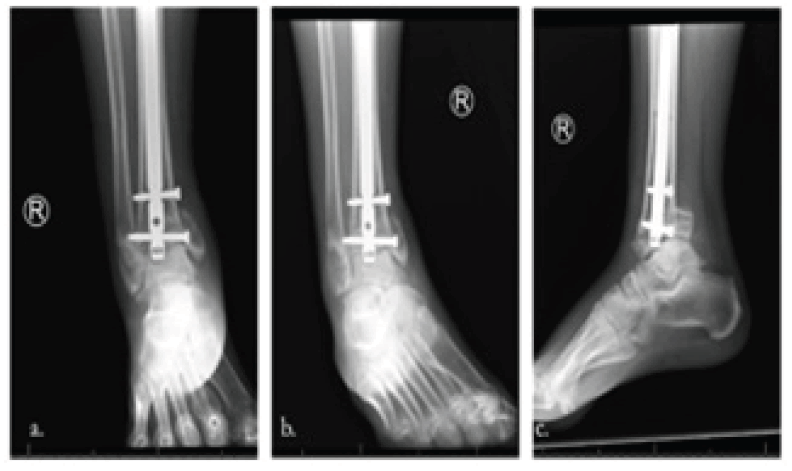
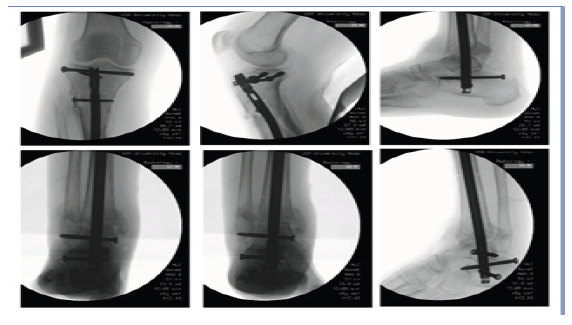
She presented one week later with complaints of severe swelling around her right ankle, and radiographs demonstrated an acute pilon fracture with tibial nail intrusion resulting in varus deformity and talar impaction (Fig 4a, b and c, 5a-g). She was instructed to present promptly back to University Hospital for further surgical intervention. Upon arrival, the patient’s primary complaint was right ankle swelling and pain. 14-point cursory review of systems was otherwise negative for constitutional symptoms, respiratory, cardiovascular, neurologic, psychiatric, or other musculoskeletal complaints. Exam revealed swelling of the right lower extremity from the level of the knee distally, more prominent about the ankle, soft and compressible compartments, limited ankle range of motion secondary to pain and an unchanged global decrease in foot sensation related to her neuropathy. She was admitted and the following morning underwent anterograde intramedullary fixation of the right tibia and ankle to support her initial tibial plateau and shaft fractures and provide salvage TTC arthrodesis, respectively (Fig. 6). She tolerated the procedure well and was discharged without complication.
The patient presented for scheduled routine follow-up visits without complication. At her six-week follow-up visit in late April, 2021, radiographs demonstrated favorable callus formation at her fracture sites. She was advised to slowly advance to weightbearing as tolerated at this time.
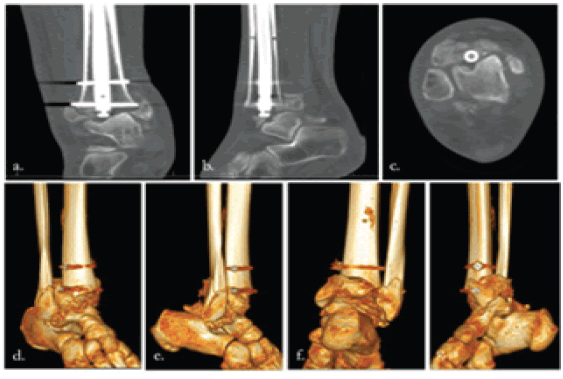
Radiographs at her three-week follow-up demonstrated hardware to be in good position (Fig. 7). Repeat radiographs and CT scan at five months demonstrated proper hardware alignment but minimal tibiotalar fusion (Fig. 8a-d). At this time the patient was allowed to bear weight in a cam walker boot, encouraged to optimize her nutrition, and begun on a bone stimulator. Follow-up three months later revealed improved interval tibiotalar fusion and bone healing (Fig. 9). She was ambulating without pain.
Surgical Technique
The patient was placed in the supine position on the operative table. Bony prominences were padded. The operative site was prepped and draped in the usual sterile fashion. An operative timeout was performed with all members of the surgical team at attention to identify the appropriate patient, surgical site, safety concerns and procedure.
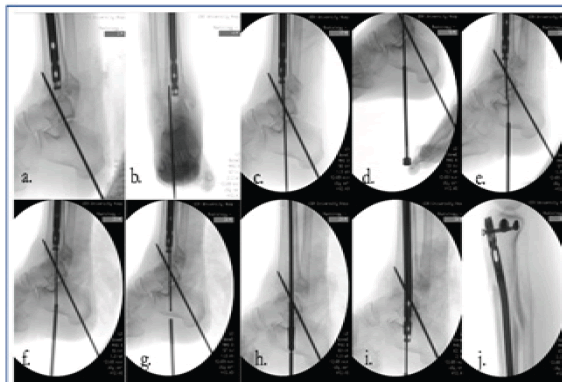
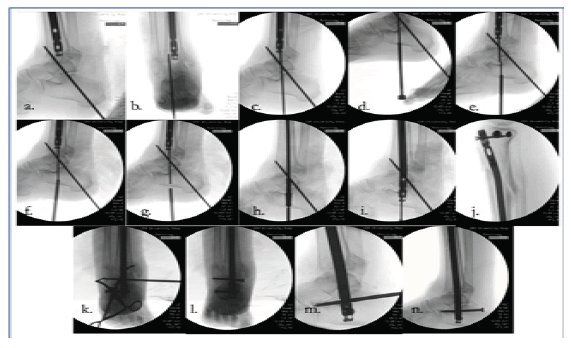
We began the procedure with unlocking of the tibial nail. The screws were first removed from the tibial nail under fluoroscopic imaging using small incisions. We then placed the insertion cannula and trocar for the suprapatellar nail. Through the cannula the extraction device was inserted allowing us to backslap the nail for removal. The insertion handle was then placed back onto the tibial nail, and it was reinserted into the tibia. We then passed a 3.2 mm guidewire which had been fashioned to a sharp point anterograde down the tibial nail. A direct anterior approach to the tibial plafond was performed where we debrided the fracture fragments and cleaned them of cartilage on the back table to later use for bone grafting. The cartilage was debrided from the talar dome. Drill holes were placed into the subchondral bone of the talus. We then placed the ankle in a neutral dorsiflexion position with slight hindfoot eversion and external rotation. A 3.2 mm terminally threaded guidewire was placed from the calcaneus retrograde into the distal tibia under fluoroscopic imaging for provisional hindfoot fixation (Fig 10a, b). With the ankle in appropriate position the anterograde guidewire was advanced to the plantar aspect of the calcaneus. This point was marked fluoroscopically. We then advanced the wire out the plantar aspect of the hindfoot (Fig. 10c). An exchange cannula was placed through a small incision on the plantar aspect of the foot (Fig 10d). A 2.5 mm bead tip guidewire was advanced in a retrograde fashion through the same wire tract and into the tibial nail (Fig 10e-g). The wire was advanced out the proximal portion of the tibial nail. Measurement for nail length was taken. The original nail was then removed. In anterograde fashion we reamed the tibia, talus and calcaneus to a diameter of 12 mm (Fig 10h). A Synthes 11 mm x 405 mm tibial nail was inserted (Fig 10i). Two proximal interlocking screws were placed in prior tracts (Fig 10j). We compressed distally with a mallet and placed three distal interlocking screws with perfect circle freehand technique (Fig 10k-n). Initial provisional hindfoot fixation pin was removed. Fluoroscopic evaluation and direct visualization confirmed appropriate reduction and hardware placement (Fig. 6). The nail was used to fixate the proximal tibia and fuse the tibiotalar and subtalar articulations. We packed the tibiotalar fusion site with bone graft. Wounds were irrigated with normal saline. The extensor retinaculum was closed with #1 Vicryl in interrupted fashion. The dermis was closed with 2-0 Vicryl in buried, interrupted fashion. Skin was closed with 3-0 nylon suture. Clean sterile dressings and a short leg splint were applied. The patient was awakened by anesthesia and taken to recovery in stable condition. Postoperatively, she was made non-weightbearing on the right lower extremity with recommended chemical DVT prophylaxis and 24 hours of scheduled antibiotics.
Figure 10: Technique radiographs showing provisional hind foot fixation (a,b), anterograde exchange guidewire passage(c), Exchange cannula(d), Retrograde guidewire passage (e,f,g), Reaming(h), Nail placement(i), Two proximal locking screws (j), Three distal talocalcaneal interlocking screws(k,l,m,n).
Discussion
As previously mentioned, TTC arthrodesis is employed for a myriad of complex hindfoot problems. Acute trauma with bone loss, various forms of arthritis, Charcot arthropathy, talar pathologies including AVN and traumatic destruction, failed ankle arthroplasty or fusion, and even mechanical stabilization status-post chopart amputation have been listed as indications [1-27]. More recently, primary treatment of fragility ankle fractures in the elderly and revision fixation for failed ORIF or malunited fractures in insensate, diabetic patients have emerged as further potential indications [21,29-31-35]. Here, we present a case perhaps detailing a new potential use for intramedullary hindfoot fusion; an insensate, diabetic patient with an acute plafond fracture and associated talar injury following osseous failure and bimalleolar collapse around her existing tibial nail. This patient also had recent proximal tibial shaft and lateral plateau fractures to be considered in her final fixation construct. To our knowledge, literature has yet to describe, not only this injury pattern from spontaneous failure around tibial hardware, but also concomitant tibial plateau and shaft fixation with hindfoot arthrodesis in a single construct, the focus of our report.
Intramedullary nails used for TTC arthrodesis provide many benefits over pins, screws and plates, or external fixators. Nails are loadsharing devices that offer additional mechanical advantages of higher bending stiffness, increased rotational stability and compression capabilities [3-5,7-8,10,20,22]. It has been established that nail systems provide more rigid and stable fixation than other constructs in patients with impaired bone quality (e.g. rheumatoid, diabetic, and neuropathic patients) [3]. In addition to mechanical advantages, minimally invasive intramedullary devices preserve soft tissue, enhancing biology for fracture healing and thereby also reduce infection risks related to wound breakdown. [12,14,21]. Tarkin and Fourman point out that reaming a path for the nail also creates cancellous autograft further adding to favorable surrounding biology for fracture healing. [14]. Another important consideration regarding wound healing is anterograde versus retrograde nailing. The majority of intramedullary hindfoot fusions are performed in retrograde fashion with few reported exceptions [12,26]. Jain et al. opted for a retrograde technique where tibial shaft fixation and ankle arthrodesis were required due to perceived difficulty of antegrade tibiocalcaneal fixation. In German literature both anterograde and retrograde intramedullary TTC arthrodesis have been described, however, Günter and Heller suggest inserting the nail in an anterograde manner to protect soft tissues and allow earlier load bearing [12,18]. Given our patient’s initial injury having both tibial plateau and shaft fractures with a concomitant acute pilon fracture, anterograde fixation was warranted and afforded our patient this plantar soft tissue benefit.
The use of a long nail in our patient, as opposed to the commonly used standard TTC nail, may also prevent future complications of a periprosthetic fracture which is reported to occur at the proximal tip of standard short nails [23,27,28,35]. Current literature suggests periprosthetic, mid-tibial fractures related to short TTC nails occur at rates of between 6%-14% in elective cases and up to 10% in trauma cases. Use of longer nails in elderly and neuropathic patients that cross the tibial isthmus have been shown to potentially avoid this problem [23,27,35]. In a cadaveric, biomechanical study by Noonan et al., an area of strain on the posterior cortex of the tibia was identified at the level of proximal screw holes in standard-length (“short”) locked nails that was 5.3 times higher than that of locked “long” nails [28]. This concentrated stress was shown to dissipate with use of nails terminating in the proximal tibial metaphysis. In two separate studies by Baker et al. and Al-Nammari et al. treatment of fragility ankle fractures with use of long intramedullary nails crossing the isthmus led to no reports of peri-prosthetic fracture at follow-up, presumably related to absence of a stress riser [23, 35]. We may have also afforded our patient this benefit by use of a long nail which again was already warranted by her injuries.
Complications related to intramedullary TTC arthrodesis include nonunion, delayed union, malunion, infection, periprosthetic fracture, hardware failure, lateral plantar nerve injuries and wound healing difficulties, the latter two of which we have reduced the risk of by way of anterograde technique [1]. Fusion rates for intramedullary TTC arthrodesis of 76% to 100% are reported with time to fusion being roughly 16 weeks [4]. One of the largest systematic literature reviews for intramedullary TTC arthrodesis by Jehan et al. included 33 studies and 659 procedures and found average union rate to be 86.7% with average union time of 4.5 months [8]. Diabetes, neuropathy, osteopenia, smoking, and use of methotrexate or NSAIDS are factors that can negatively affect TTC arthrodesis outcomes [4,7,32,36] . Our patient had both neuropathy and diabetes, possibly resulting in her delayed union at 20 weeks (Fig. 6). With implementation of mechanical loading by way of weight-bearing and use of a bone stimulator, interval hindfoot fusion resulted.
Conclusion
While diabetes is a risk factor for hardware migration, it is unclear why our patient failed around her index tibial nail resulting in an acute pilon fracture and talar injury at only six weeks post-operatively. In the setting of this unfortunate hardware failure, we have shown that tibial nailing is a viable treatment option to provide tibial plateau and shaft fixation and hindfoot arthrodesis in neuropathic patients with pre-existing proximal tibial injuries that have experienced failure around intramedullary hardware. In the absence of tibial plateau and shaft injuries, we would still suggest use of a long nail to avoid potential future stress fractures which have been reported by other authors. When possible, we recommend antegrade nail passage to potentially reduce the risk of plantar wound complications, particularly in diabetic patients.
Acknowledgements
Consent was obtained by patient for publication of the study.
Conflicts Of Interest Statement
The authors have no competing interests or relationships that could inappropriately influence their work.
References
- Woods JB, Burns PR. Advances in intramedullary nail fixation in foot and ankle surgery. Clinics in Podiatric Medicine and Surgery. 2011; 28(4):633-648. [Google Scholar] [CrossRef]
- Franceschi F, Franceschetti E, Torre G, et al. Tibiotalocalcaneal arthrodesis using an intramedullary nail: a systematic review. Knee Surgery, Sports Traumatology, Arthroscopy. 2016;24(4):1316-1325. [Google Scholar] [CrossRef]
- Shah KS, Younger AS. Primary tibiotalocalcaneal arthrodesis. Foot Ankle Clinics. 2011;16(1):115-136. [Google Scholar] [CrossRef]
- Thomas RL, Sathe V, Habib SI. The use of intramedullary nails in tibiotalocalcaneal arthrodesis. JAAOS-J American Academy Orthopaedic Surg. 2012;20(1):1-7. [Google Scholar] [CrossRef]
- Steele JR, Lazarides AL, DeOrio JK. Tibiotalocalcaneal arthrodesis using a novel retrograde intramedullary nail. Foot Ankle Specialist. 2020;13(6):463-469. [Google Scholar] [CrossRef]
- Thomas AE, Guyver PM, Taylor JM, et al. Tibiotalocalcaneal arthrodesis with a compressive retrograde nail: a retrospective study of 59 nails. Foot Ankle Surgery. 2015;21(3):202-205. [Google Scholar] [CrossRef]
- Mendicino RW, Catanzariti AR, Saltrick KR, et al. Tibiotalocalcaneal arthrodesis with retrograde intramedullary nailing. J Foot Ankle Surg. 2004;43(2):82-86. [Google Scholar] [CrossRef]
- Jehan S, Shakeel M, Bing AJ, et al. The success of tibiotalocalcaneal arthrodesis with intramedullary nailing: A systematic review of the literature. Acta Orthopaedica Belgica. 2011;77(5):644. [Google Scholar]
- Burks JB. Tibiotalocalcaneal arthrodesis. Clinics Podiatric Medicine Surgery. 2012; 29(4):529-545. [Google Scholar] [CrossRef]
- Pelton K, Hofer JK, Thordarson DB. Tibiotalocalcaneal arthrodesis using a dynamically locked retrograde intramedullary nail. Foot ankle Intern. 2006 Oct; 27(10):759-763. [Google Scholar] [CrossRef]
- Rammelt S, Pyrc J, Ågren PH, et al. Tibiotalocalcaneal fusion using the hindfoot arthrodesis nail: a multicenter study. Foot & ankle international. 2013;34(9):1245-1255. [Google Scholar] [CrossRef]
- Günter U, Jentsch P, Heller G. Anterograde intramedullary tibio-talo calcaneus arthrodesis (aIMTCA) with spongiosaplasty in pseudarthrosis. Der Unfallchirurg. 2002;105(5):474-477. [Google Scholar] [CrossRef]
- Goebel M, Gerdesmeyer L, Mückley T, et al. Retrograde intramedullary nailing in tibiotalocalcaneal arthrodesis: a short-term, prospective study. Journal Foot Ankle Surg. 2006;45(2):98-106. [Google Scholar] [CrossRef]
- Tarkin IS, Fourman MS. Retrograde hindfoot nailing for acute trauma. Current Rev Musculoskel Med. 2018;11(3):439-444. [Google Scholar] [CrossRef]
- Mader K, Verheyen CC, Gausepohl T, et al. Minimally invasive ankle arthrodesis with a retrograde locking nail after failed fusion. Strategies Trauma Limb Reconstr. 2007;2(1):39-47. [Google Scholar] [CrossRef]
- Mohammad HR, A’Court J, Pillai A. Extruded talus treated with reimplantation and primary tibiotalocalcaneal arthrodesis. Annals Royal College Surg Eng. 2017;99(4):e125-127. [Google Scholar] [CrossRef]
- Tenenbaum S, Stockton KG, Bariteau JT, et al. Salvage of avascular necrosis of the talus by combined ankle and hindfoot arthrodesis without structural bone graft. Foot & Ankle International. 2015;36(3):282-287. [Google Scholar] [CrossRef]
- Klos K, Lange A, Matziolis G, et al. Tibia-Allograft-Kalkaneus-Arthrodese mit retrogradem Nagel. Der Orthopäde. 2013;42(5):364-370. [Google Scholar] [CrossRef]
- Asomugha EU, Den Hartog BD, Junko JT, et al. Tibiotalocalcaneal fusion for severe deformity and bone loss. JAAOS-Journal American Academy Orthopaedic Surg. 2016;24(3):125-134. [Google Scholar] [CrossRef]
- Brodsky JW, Verschae G, Tenenbaum S. Surgical correction of severe deformity of the ankle and hindfoot by arthrodesis using a compressing retrograde intramedullary nail. Foot & Ankle Intern. 2014; 35(4):360-367. [Google Scholar] [CrossRef]
- Kulakli-Inceleme E, Tas DB, Smeeing DP, et al. Tibiotalocalcaneal intramedullary nailing for unstable geriatric ankle fractures. Geriatric Orthopaedic Surgery & Rehabilitation. 2021;12. [Google Scholar] [CrossRef]
- Zak L, Wozasek GE. Tibio-talo-calcaneal fusion after limb salvage procedures—a retrospective study. Injury. 2017;48(7):1684-8. [Google Scholar] [CrossRef]
- Baker G, Mayne AI, Andrews C. Fixation of unstable ankle fractures using a long hindfoot nail. Injury. 2018;49(11):2083-6. [Google Scholar] [CrossRef]
- Schepers T, Hagenaars T, Den Hartog D. An irreducible ankle fracture dislocation: the Bosworth injury. The Journal Foot Ankle surg. 2012;51(4):501-503. [Google Scholar] [CrossRef]
- Jain NS, Lopez GD, Bederman SS, et al. Surgical management of complex lower-extremity trauma with a long hindfoot fusion nail: a case report. Foot & Ankle Specialist. 2016;9(4):354-60. [Google Scholar] [CrossRef]
- Andrea CD, Scoccianti G, Beltrami G, et al. Ankle arthrodesis with bone graft after distal tibia resection for bone tumors. [Google Scholar] [CrossRef]
- Pinzur MS, Noonan T. Ankle arthrodesis with a retrograde femoral nail for Charcot ankle arthropathy. Foot & ankle international. 2005;26(7):545-549. [Google Scholar] [CrossRef]
- Noonan T, Pinzur M, Paxinos O, et al. Tibiotalocalcaneal arthrodesis with a retrograde intramedullary nail: a biomechanical analysis of the effect of nail length. Foot & Ankle International. 2005;26(4):304-308. [Google Scholar] [CrossRef]
- Vaudreuil NJ, Fourman MS, Wukich DK. Limb salvage after failed initial operative management of bimalleolar ankle fractures in diabetic neuropathy. Foot Ankle International. 2017;38(3):248-254. [Google Scholar] [CrossRef]
- Wallace SJ, Liskutin TE, Schiff AP, et al. Ankle fusion following failed initial treatment of complex ankle fractures in neuropathic diabetics. Foot and Ankle Surgery. 2020;26(2):189-92. [Google Scholar] [CrossRef]
- Pinzur MS. Transarticular stabilization for malunited fracture of the distal tibia in diabetics with loss of protective sensation. Foot & Ankle International. 2001;22(9):706-10. [Google Scholar] [CrossRef]
- Manon J, Detrembleur C, Van de Veyver S, et al. Predictors of mechanical complications after intramedullary nailing of tibial fractures. Orthopaedics Traumatology: Surgery Research. 2019;105(3):523-527. [Google Scholar] [CrossRef]
- Georgiannos D, Lampridis V, Bisbinas I. Fragility fractures of the ankle in the elderly: open reduction and internal fixation versus tibio-talo-calcaneal nailing: short-term results of a prospective randomized-controlled study. Injury. 2017;48(2):519-24. [Google Scholar] [CrossRef]
- Raunest J, Kynast W, Lesch V, et al. Geometric properties of the fractured tibia stabilized by unreamed interlocking nail: development of a three-dimensional finite element model. Computers Biomedical Research. 1996;29(4):259-70. [Google Scholar] [CrossRef]
- Al-Nammari SS, Dawson-Bowling S, Amin A, et al. Fragility fractures of the ankle in the frail elderly patient: treatment with a long calcaneotalotibial nail. Bone Joint Jl. 2014;96(6):817-22. [Google Scholar] [CrossRef]
- Niikura T, Miwa M, Sakai Y, et al. Ankle arthrodesis using antegrade intramedullary nail for salvage of nonreconstructable tibial pilon fractures. Orthopedics (Online). 2009;1;32(8):611. [Google Scholar] [CrossRef]





 Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.
Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.