Intramedullary versus extramedullary minimally invasive fixation for tibial shaft fractures: A prospective long-term follow-up of 81 cohort
2 Al-Fayhaa Teaching Hospital, Basrah Health Directorate, Ministry of Health, Basrah, Iraq
3 Al-Zubair General Hospital, Basrah Health Directorate, Ministry of Health, Basrah, Iraq
Received: 29-May-2025, Manuscript No. jotsrr-25-166609; Editor assigned: 02-Jun-2025, Pre QC No. jotsrr-25-166609 (PQ); Reviewed: 16-Jun-2025 QC No. jotsrr-25-166609; Revised: 29-Jul-2025, Manuscript No. jotsrr-25-166609 (R); Published: 04-Aug-2025
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: Tibial shaft fractures are a common injury, with various fixation techniques available. This study aims to compare two minimally invasive methods of fracture fixation MIPO (Minimally Invasive Plate Osteosynthesis) and IMN (Intramedullary Nail) and evaluate their impact on clinical outcomes, complications and cost-effectiveness.
Materials and methods: A prospective cohort study was conducted in Basra from 2013-2023. In this timeframe, 81 skeletally mature patients, had tibial shaft fractures due to different mechanisms. All were treated with minimally invasive methods of fracture fixation (MIPO and IMN). Patients were followed for a period ranging from (6 to 24 months) regarding union rate and functional outcome, and monitoring of any complication.
Results: Eighty-one patients (68 males and 13 females), aged 17-72 years their mean age was 36.14 ± 12.86 years. 39 patients with MIPO and 42 with IMN. The time spent during surgery was longer among the IMN group, (p=0.035). The length of surgical incision was longer among the MIPO group 4.36 cm and more blood loss was noticed during the IMN surgery. The number of screws used during operation was higher in the MIPO group. The mean healing time was better among the IMN group. Regarding the post-op complications, no significant difference between the two types of surgery.
Conclusion: Both MIPO and IMN offer effective treatment for tibial shaft fractures, with their choice depending on various factors. While IMN may be more cost-effective and result in faster healing times and fewer hardware requirements, MIPO may still be preferred in certain cases based on individual patient needs.
Introduction
Tibial shaft fractures are one of the most formidable injuries to repair due to the perilous blood supply and thin soft tissue protecting the tibia due to its subcutaneous position. These injuries frequently result in open fractures, serious sequel, and significant impairments [1]. It is extremely common, representing 16.9/100,000/year. The incidence is higher in males in their 1st decade compared to females in their 3rd decade [2].
Minimal-Invasive Surgery (MIS) in orthopaedics became an essential procedure. It aims to reduce the bleeding by minimizing soft tissue damage, preserve periosteal vascularity and minimally disrupting the fracture hematoma. The fracture is stabilized internally, by an indirect reduction technique. This ensures early mobilization without bracing or casting, fast healing, early weight-bearing and self-care assignments; so, convalescence duration together with the hospital length of stay and postoperative morbidities kept to a minimum as well. Wounds heal cosmetically with remarkably reduced complications in areas with thin soft tissue envelopes without affecting the surgical goals. The same minimally invasive route may be followed to remove implants as necessary [3].
Intramedullary Nailing (IMN) had been patented by Küntscher in 1939 [4]. It speeds up weight-bearing and union while reducing the risk of various complications [5-8]. However, anterior knee pain and malunion are real concerns [9].
On the other hand, Open Reduction and Internal Fixation (ORIF) or Minimally Invasive Percutaneous Plate Osteosynthesis (MIPO) are the two methods utilized plate fixation. Whereas, MIPO (introduced by Krettek in the Nineties), a variation of ORIF, uses an indirect bridge reduction strategy and causes less damage to the blood supply, which may help to mitigate the disadvantages of ORIF [10,11].
Screws are inserted through perforated holes, and plates are "slipped" beneath the sub-muscular plane using tiny incisions. In osteoporotic bone, low-contact anatomical plates with angular stable locking screws have significantly improved anchoring and reduced prominence [12].
The choice of the best surgical technique for tibia fractures is up for debate since there is no coexistence between the dominance of IMN and plate fixation. Because of their methodology, many retrospective studies that compare the two surgical techniques give low evidence levels [13-18].
This study aims to compare two minimally invasive methods of fracture fixation MIPO (Minimally Invasive Plate Osteosynthesis) and IMN (Intramedullary Nail) and evaluate their impact on clinical outcomes, complications, and cost-effectiveness.
Materials and Methods
A prospective cohort study was conducted in Basra from 2013-2023. In this timeframe 81 skeletally mature patients (68 males and 13 females), aged 17-72 years (36.14 ± 12.86) had tibial shaft fractures due to different mechanisms (59 due to RTA, 16 due to falling accidents,5 athletes due to sports activities and 1 due to occupational injuries) all were treated with minimally invasive methods of fracture fixation (39 with MIPO” Minimally Invasive Plate Osteosynthesis” and 42 with IMN” Intramedullary Nail”). Patients with open fractures of bullets, fractures of advanced Gustilo stage (III and its subdivisions), pathological fractures, intraarticular fractures, uncontrolled diabetes, incomplete or insufficient (<6 months) follow-up and fractures associated with traumatic brain injuries or peripheral nerves and/or vascular injuries were excluded from the study.
After getting written and/or verbal consent. Those cases were enrolled for follow-up of a minimum of 6 months and maximum of 24 months duration regarding union rate and functional outcome using a Jeju Lower Extremity Trauma Score (JLETS) in hand with modified Radiological Union Score of Tibia (MRUST); also monitoring of any complication(s) in regard of delayed union, malunion, infection, thromboembolism, compartment syndrome, fracture disease (Sudeck’s dystrophy) and reoperation. Time of surgery and amount of radiation (number of fluoroscopy images, perspective time of fluoroscopy) were examined as well. The difference in the cost between the two fixation modalities was also evaluated, weight-bearing and return to normal daily activity and occupational life.
Surgeries were conducted under general, regional and spinal anesthesia depending on patients’ general conditions, comorbidities and associated injuries;therefore, the time to surgery differed accordingly.
Antibiotics (3rd or 4th generation cephalosporin) were given routinely to all patients at the time of anaesthesia induction. Then extended for the subsequent 3-5 days postoperatively.
MIPO group
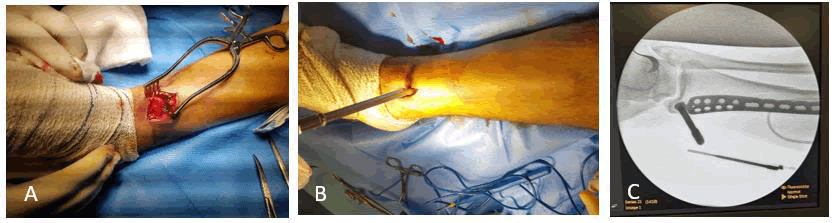
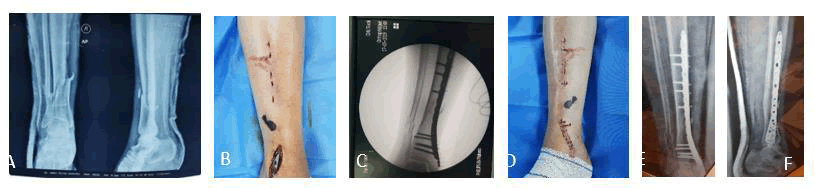
Patients in the supine position, draping done, 4-5 cm incisions proximal and distal far away from fracture site (without disrupting the fracture milieu). The locked plate was inserted in the submuscular plane after fracture reduction and external manipulation to gain rather anatomical alignment than anatomical reduction under fluoroscopy imaging; the anatomical plates were introduced from its straight (non-anatomical arm; for easy insertion with minimal fracture fragments’ disruption). Usually, the first screw(s)on either side of the fracture were nonlocked to achieve a reduction in a way that made the plate in close contact with the bone. Then the rest locked screws tightened in place, leaving the fracture area not fixed nor penetrated even with an inter fragmentary screw. Formal closure in layers, skin closed with stapler (Figures 1 and 2).
Fig. 1. Presents some operative steps; A) Preparing the tunnel for plate insertion. B) Insertion of the anatomical locked plate with the aid of a sleeve tightened to the most distal plate hole. C) Fluoroscopy checking image for proper plate insertion and bone alignment.
Fig. 2. A) Radiograph of right tibia showing fracture at lower shaft. B) Distal medial 3 cm incision for insertion of distal tibial medial anatomical locked plate and proximal punctures for insertion of proximal screws. C) Fluoroscopy image for the fracture after reduction and fixation. D) Closure of the incision and punctures with staples. E and F) AP and lateral postoperative radiographs.
IMN group
Patients in the supine position, draping done, the leg rested on a radiolucent sterile frame (plastic or wooden) knee flexed 45°, or the leg hang over the operating table (90° knee flexion). Three cm incision (from the lower pole of the patella to tibia tuberosity), then passing medial to or through the patellar tendon. Then the guide wire anterior to the tibial spine (eminence) as a pilot hole under fluoroscopy image intensification both anteroposterior and lateral view to guarantee the proper site of entrance for the subsequent steps; introducing the awl then the ball-tipped guide wire to continue the steps of reduction then reaming of the intramedullary canal. The reaming started with the smallest reamer size to reach the optimum size of reaming in a step manner, then choosing an intramedullary nail 1 cm smaller than the last reamer size. Further check for the nail size and length was also done, introducing the nail smoothly into the bone. Distal locking screws tightened (either freehand or with the assistance of a locking device). The fracture was checked with imaging about the reduction (which sometimes required a step of fracture impaction when there is displacement). Proximal screws then tightened. Closure in layers of the main incision skin and other punctures closed with a stapler (Figure 3).
Fig. 3. A) Radiograph showing fracture lower shaft of right tibia. B) 3 cm anterior right knee incision (lower pole of patella to tibial tuberosity) with proximal and distal 2 x 2 punctures for insertion of derotation locked screws. C) Postoperative radiograph AP and lateral. D) The way of hanging the leg on the regular operating table.
All surgeries were fluoroscopy-assisted. All patients were sent for radiography immediately postoperatively, then after two weeks at the time of skin staples removal, then monthly for the first three months (almost fractures united at this period) and every three months for the rest of the first year.
Analgesics were paracetamol 1-gram X4, narcotics used for day 0 and day 1 postoperatively. No nonsteroidals were used at all (delay both the wounds and the fracture healing).
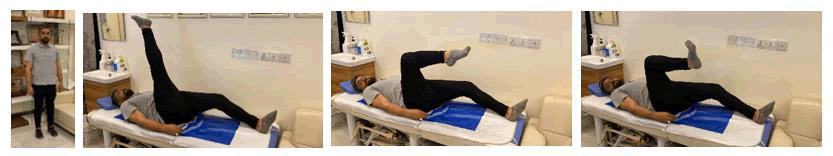
All patients were involved in active and passive exercises and rehabilitation programs. We examined the functional outcome using JLETS (Jeju lower extremity trauma score) while the radiological union was evaluated using a modified Radiological Union Score of Tibia (mRUST) (Figures 4 and 5).
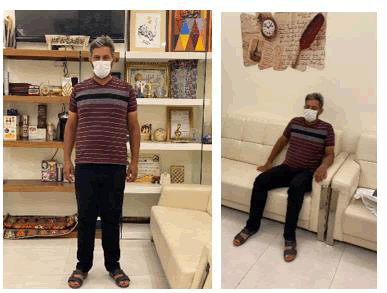
Fig. 4. Patient with MIPO of right tibia fracture bearing weight 12 weeks postoperatively, with full range of movement of ankle and knee joints.
Fig. 5. Patient with IMN of right tibia; bearing weight 8 weeks postoperatively and sitting comfortably.
The data were analyzed using SPSS version 26. Quantitative variables were expressed as mean standard deviation and the qualitative variables were presented as numbers and percentages. A p-value of ≤ 0.05 was considered as significant statistically.
Results
A total of 81 patients with extra-articular tibial fractures were enrolled in this study sustaining two types of minimally invasive surgeries; 42 patients underwent IMN and 39 patients treated with MIPO. There were no significant differences regarding the age, sex, mechanism of injury, duration of follow-up and side of injury between the patients randomized to each group since the pvalue> 0.05. these data are presented in Table 1.
The fibula status was recorded, it was intact in 14 cases only, the other 67 cases had fractured fibula and only one of them needed fixation of the fibula.
The fractures were classified according to the AO/OTA classification system showing that 27 of the cases were 42A3, 23 were 42A2, then 17 were 42B3 and only one case was 42C1.
The Gustillo classification of open fractures was assessed also and showed that the majority of patients had closed fractures, only 10 cases were class two open fractures.
Regarding the associated fractures present among 4 cases in the first group and 5 cases in the second group.
|
Variables |
IMN (n =42) |
MIPO (n=39) |
p-value |
|
|
Age |
34.95 ± 11.36 |
37.41 ± 14.38 |
0.394 |
|
|
Sex |
Male |
36 (85.7) |
32 (82.1) |
0.654 |
|
Female |
6 (14.3) |
7 (17.9) |
||
|
Mechanism of injury |
Fall |
7 (16.7) |
9 (32.1) |
0.537 |
|
Occupational injury |
0 |
1 (2.6) |
||
|
RTA |
33 (78.6) |
26 (66.7) |
||
|
Sport injury |
2 (4.8) |
3 (7.7) |
||
|
Duration of follow-up (years) |
5.09 ± 2.7 |
5.28 ± 2.72 |
0.758 |
|
|
Side of injury |
Right |
29 (69.0) |
25 (64.1) |
0.637 |
|
Left |
13 (31.0) |
14 (35.9) |
||
|
AO/OTA class system |
42A1 |
1 (2.4) |
1 (2.6) |
0.391 |
|
42 A2 |
9 (21.4) |
14 (35.9) |
||
|
42 A3 |
14 (33.3) |
13 (33.3) |
||
|
42 B1 |
1 (2.4) |
2 (5.1) |
||
|
42 B2 |
1 (2.4) |
2 (5.1) |
||
|
42 B3 |
12 (28.6) |
5 (12.8) |
||
|
42 C1 |
0 (0.0) |
1 (2.6) |
||
|
42 C2 |
4 (9.5) |
1 (2.6) |
||
|
Gustillo's classification of open fractures |
0 |
21 (50.0) |
22 (56.4) |
0.483 |
|
1 |
15 (35.7) |
13 (33.3) |
||
|
2 |
6 (14.3) |
4 (10.3) |
||
|
Associated fracture |
No |
38 (90.5) |
34 (87.2) |
0.637 |
|
Yes |
4 (9.5) |
5 (12.8) |
||
Table 1. The demographic and fracture-related characteristics concerning the type of surgery.
The surgery-related characteristics are presented in Tables 2 and 3. The mean time between injury to surgery was higher in the IMN group (27.67 hours) in comparison to (23.64 hours) in the MIPO group. Still, there is no significant statistical difference between them (p=0.486).
The mean time spent during surgery was longer among the IMN group 72.28 minutes vs. 65.23 minutes in the MIPO group and the p-value was significant (p=0.035).
The length of surgical incision was longer among the MIPO group in comparison to the IMN group (4.36 vs. 3.21 cm for both groups respectively) (p=0.001).
The mean blood loss during surgery was estimated, and more blood loss was noticed during the IMN surgery, and this difference is of a statistically significant (p=0.001).
The site of the plate used in MIPO surgery was also recorded, with its medial plate at 51.6% and lateral at 48.4% of patients. The number of screws used during operation was higher in the MIPO group, around 8 screws vs. nearly 4 in IMN and the difference was significant (p=0.001).
The mean number of fluoroscopy images needed during surgery was nearly similar among both groups and the p-value=0.731. regarding the perspective time of fluoroscopy was significantly higher among the IMN group (p=0.001).
| Variables | IMN (n =42) | MIPO (n=39) | p-value |
| Time to surgery (hrs) | 27.67 ± 4.37 | 23.64 ± 3.67 | 0.486 |
| Time of surgery (min.) | 72.28 ±17.7 | 65.23 ± 10.84 | 0.035 |
Table 2. The chronological comparison of time from injury to surgery and the duration of surgery among patients (mean ± SD).
| Variables | IMN (n =42) | MIPO (n=39) | p-value | |
| Length of incision (cm) | 3.21 ± 0.47 | 4.36 ± 0.48 | 0.001 | |
| Estimated bleeding (ml) | 197.5 ± 65.64 | 76.36 ± 21.02 | 0.001 | |
| Plate location regarding tibia | Medial | 0 | 16 (51.6) | NA |
| Lateral | 0 | 15 (48.4) | ||
| Number of screws* | 4.02 ± 0.15 | 8.36 ± 1.44 | 0.001 | |
| Number of fluoroscopy images | 56.36 ±13.87 | 55.15 ±15.02 | 0.731 | |
| perspective time of fluoroscopy | 32.85 ± 4.89 | 24.15 ± 5.37 | 0.001 | |
| Note: mean ± SD/ No.(%) | ||||
Table 3. The surgery related characteristics.
Table 4 presents the postoperative results concerning healing and complications in the two groups. The mean healing time was better among the IMN group than MIPO and the difference was significant (p=0.011).
The mean time of weight bearing was better in the IMN group and the difference was significant (p=0.001).
No significant difference between groups regarding the Jeju Lower Extremity Trauma Score (JLETS) and its components (p>0.05).
The modified Radiological Union Score of Tibia (mRUST) shows a higher mean in the IMN group, and this difference is of statistical significance (p=0.001). The anterior knee pain was mentioned by 56.4% of patients in the IMN group only. Regarding the post-op complications, no significant difference between the two types of surgery.
| Variables | IMN (n=42) | MIPO (n=39) | p-value |
| Healing (week) | 10.95 ± 1.13 | 11.87 ± 1.98 | 0.011 |
| Weight bearing (week) | 6.86 ± 1.11 | 11.48 ± 2.32 | 0.001 |
| VAS | 8.23 ± 1.18 | 8.3 ± 1.41 | 0.811 |
| Activity | 27.09 ± 0.84 | 26.69 ± 1.00 | 0.054 |
| ROM | 8.19 ± 0.74 | 8.23 ± 0.9 | 0.826 |
| Tenderness | 2.8 ± 0.74 | 2.6 ± 1.41 | 0.429 |
| Jeju Lower Extremity Trauma Score (JLETS) | 46.33 ± 1.84 | 45.92 ± 2.69 | 0.424 |
| Medial callus | 2.66 ± 0.47 | 2.31 ± 0.52 | 0.002 |
| Lateral callus | 2.74 ± 0.44 | 2.21 ± 0.57 | 0.001 |
| Anterior callus | 2.76 ± 0.43 | 2.79 ± 0.41 | 0.725 |
| Posterior callus | 2.47 ± 0.52 | 2.53 ± 0.51 | 0.581 |
| modified Radiological Union Score of Tibia (mRUST) | 10.64 ± 0.98 | 9.84 ± 0.87 | 0.001 |
| Yes | 22 (56.4) | 0 (0.0) | 0.01 |
| No | 17 (43.6) | 42 (100.0) | |
| Recurvatum 3° | 0 (0.0) | 1 (2.6) | 0.293 |
| recurvatum°5 | 0 (0.0) | 1 (2.6) | |
| 3° valgus | 2 (4.8) | 0 (0.0) | |
| 5°valgus | 1 (2.4) | 0 (0.0) | |
| Note: mean ± SD/ No.(%) | |||
Table 4. The post-surgery characteristics.
Discussion
Tibial shaft fractures are common injuries with various fixation techniques available. This study aims to compare two minimally invasive methods of fracture fixation MIPO (Minimally Invasive Plate Osteosynthesis) and IMN (Intramedullary Nail) and evaluate their impact on clinical outcomes, complications and cost-effectiveness. While previous studies have investigated these methods, our research aims to provide further insight and do the comparative effectiveness, particularly in terms of healing time, functional outcome and cost consideration, which are critical in clinical practice and healthcare resource management.
The matching between two groups (IMN and MIPO) in this study appears to be appropriate as there were no significant differences in key baseline variables, including age, sex, mechanism of injury, duration of follow-up and fracture side with a value greater than 0.05. This indicates that both groups were well-balanced and comparable at baseline, minimizing the potential for confounding factors that could affect the outcome measures. Furthermore, the classification of fractures and the presence of associated fractures were similar between the two groups, which strengthens the validity of the comparison.
The time from injury to surgery “does it affect the outcome”, although longer in the IMN group (27.67 hours versus 23.64 hours in MIPO), didn't show a statistically significant difference; however, the time of surgery was significantly longer for the IMN group (p-value=0.035), which could potentially lead to higher demands in this type of surgery. This finding is consistent with another study by Kaya et al., which states that IMN may require a more extensive setup, which contributes to longer surgery times [19].
The significant difference in estimated bleeding between the two groups (IMN: 197.5 ± 65.64 ml vs. MIPO: 76.36 ± 21.02 ml, p=0.001) aligns with the finding from another study by Wang et al, which suggests that IMN typically results in higher blood losses due to sequential remaining of the intermittent canal, hence more osseous bleeding from the endosteal circulation. IMN was involved in the insertion of a metal rod into the tibial canal, contributing to higher blood loss. In contrast, MIPO is designed to minimise such disruption by ensuring minimal tissue separation and plate insertion through a tunnel rather than dissection, leading to reduced blood loss similar to what was mentioned by Kashyap et al. [20].
Our findings show that both MIPO and IMN resulted in satisfactory outcomes, a significant difference was observed between the two techniques, particularly in the number of screws used during surgery and the associated cost, Specifically, the MIPO group used an average of 8.36 screws, significantly more than the 4.02 screws in the IMN group (p-value=0.001). This discrepancy is consistent with previous research by Alberio et al. which states that MIPO often required more hardware, leading to higher procedure costs and an increased number of screws in MIPO can result in increased material costs, which may be a limiting factor when considering the economic feasibility of this technique, especially in settings with constrained resources [21,22]. In contrast, the IMN method uses fewer screws and might be a more cost-effective option in terms of hardware, which aligns with findings from Kang et al. indicating that IMN tends to be associated with lower implant-related costs.
The significant difference in perspective fluoroscopy time between the two groups (IMN: 32.85 ± 4.89 min vs. MIPO: 24.15 ± 5.37 min, p=0.001) reflects the differing requirements of each surgical technique. IMN surgery generally requires more fluoroscopic guidance, as the intramedullary rod must be accurately inserted into the tibial canal, which often necessitates multiple fluoroscopic images to confirm alignment, rotation, and proper positioning of the implant. This can result in longer fluoroscopy times, as seen in this study. Conversely, MIPO is a less invasive approach that may require fewer fluoroscopic images to confirm plate placement and alignment, contributing to shorter fluoroscopy times. This finding is consistent with other studies comparing fluoroscopy time in these two techniques. For example, a study by Liu XK et al. reported that IMN procedures often require more fluoroscopic guidance due to the complexity of rod placement [23]. In contrast, MIPO, being less invasive and involving less complex instrumentation, tends to require less fluoroscopy. Similarly, Hu et al. found that MIPO is associated with reduced fluoroscopy time compared to IMN. Therefore, the shorter fluoroscopy time in the MIPO group observed in this study is consistent with existing literature and may contribute to reduced radiation exposure for both patients and surgical staff.
Interestingly, despite the increased number of screws in MIPO and longer surgical times in the IMN group, both groups showed similar functional outcomes, as measured by the Jeju Lower Extremity Trauma Score (JLETS) and no significant difference was found in the complication rates between the two groups. This suggests that, at least from a clinical outcome perspective, the two techniques may be comparable. However, the IMN group showed a higher rate of anterior knee pain (56.4%), which could be related to the more extensive surgical approach and hardware used. This aligns with previous reports that indicate knee pain can be a common complication of IMN fixation, particularly when distal screws are involved.
Another important finding was the difference in the Radiological Union Score of Tibia (MRUST), where the IMN group showed significantly better results (p-value=0.001). This could reflect the more stable fixation provided by the intramedullary nail, which has been shown to offer superior mechanical support compared to plate osteosynthesis, particularly in terms of fracture union [24]. Moreover, the shorter time to weight-bearing and faster healing time in the IMN group may also contribute to its better mRUST scores. These findings are consistent with the biomechanical advantages of IMN, which is known for its load-sharing properties that promote faster fracture healing and they are in line with the findings of Liu J, et al. [25].
Cost-wise, the additional hardware required for the MIPO procedure means that, despite similar clinical outcomes, MIPO could be more expensive in terms of material costs. When considering healthcare economics, the cost difference between the two methods could be an important factor in decision-making. Several studies have suggested that, although IMN may require longer operating times, its lower cost in terms of hardware and the possibility of fewer postoperative complications may make it a more cost-effective option [26].
This study has several limitations that should be acknowledged. First, it was conducted at a single center, which may limit the generalizability of the findings to other populations or healthcare settings. Second, the allocation of patients to either the MIPO or IMN group was not randomized, introducing the possibility of selection bias based on surgeon preference or fracture characteristics. The relatively small sample size (81 patients) may also limit the statistical power to detect subtle differences in outcomes or complication rates. Additionally, the duration of follow-up varied from 6 to 24 months, which could affect the consistency of long-term outcome assessment. Functional outcomes were not measured using standardized scoring systems, limiting objective comparison of patient recovery. Although cost-effectiveness was mentioned, a formal economic analysis was not performed. Lastly, the inclusion of fractures resulting from different mechanisms of injury introduces heterogeneity that may have influenced healing times and complication profiles. Future studies with larger, randomized cohorts and standardized outcome measures are recommended to validate these findings.
The findings of this study suggest that both MIPO and IMN are effective minimally invasive options for the treatment of tibial shaft fractures, with comparable complication rates. IMN may offer advantages in terms of shorter healing time, reduced hardware use, and potential cost savings, making it a suitable choice in many clinical scenarios. However, MIPO remains a valuable alternative, particularly in cases where intramedullary nailing is contraindicated or when fracture anatomy favors plating. These results support the need for individualized treatment planning based on patient factors, fracture characteristics, and available resources. The study also highlights the importance of considering not only clinical outcomes but also surgical efficiency and resource utilization when selecting a fixation method. Future research should focus on long-term functional outcomes, patient satisfaction, and cost-effectiveness through multicenter randomized trials.
Conclusion
In conclusion, both MIPO and IMN offer effective treatment for tibial shaft fractures, with their choice depending on various factors including the surgeon's expertise, patient characteristics and financial considerations. While IMN may be more cost-effective and result in faster healing times and fewer hardware requirements, MIPO may still be preferred in certain cases based on individual patient needs. The results of this study contribute to the growing body of literature on the cost-effectiveness and clinical outcomes of minimally invasive fracture fixation methods. Future studies with larger sample sizes are recommended to validate these findings. Additionally, randomised controlled trials could help minimise potential biases and provide stronger evidence for the comparison of IMN and MIPO techniques.
References
- Kang H, Song JK, Rho JY, et al. Minimally invasive plate osteosynthesis (MIPO) for mid shaft fracture of the tibia (AO/OTA classification 42): A retrospective study. Ann Med Surg. 2020; 60:408-12.
- Larsen P, Elsoe R, Hansen SH, et al. Incidence and epidemiology of tibial shaft fractures. Injury. 2015; 46:746-50.
- Kline AJ, Anderson RB, Davis WH, et al. Minimally invasive technique versus an extensile lateral approach for intra articular calcaneal fractures. Foot Ankle Int. 2013; 34(6):773-80.
[Crossref] [Google Scholar] [PubMed]
- Saha P, Datta P, Ayan S, et al. Plate versus titanium elastic nail in treatment of displaced mid shaft clavicle fractures: A comparative study. Indian J Orthop. 2014; 48:587–93.
[Crossref] [Google Scholar] [PubMed]
- Ekman E, Lehtimäki K, Syvänen J, et al. Comparison between nailing and plating in the treatment of distal tibial fractures: A meta analysis. Scand J Surg. 2021; 110(2):115–22.
- Hu L, Xiong Y, Mi B, et al. Comparison of intramedullary nailing and plate fixation in distal tibial fractures with metaphyseal damage: A meta analysis of randomized controlled trials. J Orthop Surg Res.2019; 14(1):30.
[Crossref] [Google Scholar] [PubMed]
- Kim CY, Jang JW. The causes and management of asymmetrical double eyelids. Facial Plast Surg.2020; 36(5):575–83.
[Crossref] [Google Scholar] [PubMed]
- Kou F, Li T. Effects of intramedullary nailing and internal fixation plates on postoperative wound infection and pain in patients with distal tibia fractures: A metaâ??analysis. Int Wound J.2024; 21(3):e14479.
- Katsoulis E, Court Brown C, Giannoudis PV. Incidence and aetiology of anterior knee pain after intramedullary nailing of the femur and tibia. J Bone Joint Surg Br.2006; 88(5):576–80.
[Crossref] [Google Scholar] [PubMed]
- Borrelli Jr J, Prickett W, Song E, et al. Extraosseous blood supply of the tibia and the effects of different plating techniques: A human cadaveric study. J Orthop Trauma.2002; 16(10):691-5.
[Crossref] [Google Scholar] [PubMed]
- Vidovi D, Matej A, Ivica M, et al. Minimallyâ??invasive plate osteosynthesis in distal tibial fractures: Results and complications. Injury.2015; 46:S96-9.
[Crossref] [Google Scholar] [PubMed]
- Fang X, Yuen CP, Kwan KY. The current role of minimal invasive surgery in orthopaedics a general overview. Ann Musculoskelet Disord. 2017.
- Sohn HS, Jeon YS, Lee J, et al. Clinical comparison between open plating and minimally invasive plate osteosynthesis for displaced proximal humeral fractures: A prospective randomized controlled trial. Injury.2017; 48(6):1175-82.
[Crossref] [Google Scholar] [PubMed]
- Krettek C, Schandelmaier P, Miclau T, et al. Minimally invasive percutaneous plate osteosynthesis (MIPPO) using the DCS in proximal and distal femoral fractures. Injury.1997; 28:A20-30.
- Cole PA, Zlowodzki M, Kregor PJ. Treatment of proximal tibia fractures using the less invasive stabilization system: Surgical experience and early clinical results in 77 fractures. J Orthop Trauma.2004; 18(8):528–35.
[Crossref] [Google Scholar] [PubMed]
- Bleeker NJ, van Veelen NM, van de Wall BJM, et al. MIPO vs. intramedullary nailing for extraâ??articular distal tibia fractures and the efficacy of intra operative alignment control: A retrospective cohort of 135 patients. Eur J Trauma Emerg Surg. 2022; 48(5):3683–91.
[Crossref] [Google Scholar] [PubMed]
- Jang Y, Wilson N, Jones J, et al. Plating versus intramedullary nailing of OTA/AO 43C1 and C2 intra articular distal tibia fractures: A propensity score and multivariate analysis. J Orthop Trauma.2024; 38(1):e9–14.
- Wang JQ, Chen ZX, Guo WJ, et al. Comparison of plate and intramedullary nail fixation of extra particular tibial fractures: A retrospective study exploring hidden blood loss. Injury.2019; 50(2):546–50.
[Crossref] [Google Scholar] [PubMed]
- Kaya O, Tosun HB, Kürüm H, et al. Comparative study of minimally invasive plate osteosynthesis (MIPO) and intramedullary nailing (IMN) for treating extra articular distal tibial fractures: Clinical and radiological outcomes. Med Sci Monit. 2023; 29:e942154.
- Kashyap S, Ambade R, Landge S, et al. Impact of surgical timing on fracture healing in tibial shaft injuries: A comparative review of intramedullary nailing techniques. Cureus.2024; 16(10):e70978.
- Alberio RL, Del Re M, Grassi FA. Minimally invasive plate osteosynthesis for proximal humerus fractures: A retrospective study describing principles and advantages of the technique. Adv Orthop.2018; 5904028.
- Schade T, Khatri C, Nwankwo H, et al. The economic burden of open tibia fractures: A systematic review. Injury.2021; 52(6):1251–59.
- Liu XK, Xu WN, Xue QY, et al. Intramedullary nailing versus minimally invasive plate osteosynthesis for distal tibial fractures: A systematic review and meta analysis. Orthop Surg.2019; 11(6):954-65.
- Leow JM, Clement ND, Tawonsawatruk T, et al. The radiographic union scale in tibial (RUST) fractures: Reliability of the outcome measure at an independent centre. Bone Joint Res.2016; 5(4):116–21.
- Liu J, Xie L, Liu L, et al. Comparing external fixators and intramedullary nailing for treating open tibia fractures: A meta analysis of randomized controlled trials. J Orthop Surg Res.2023; 18:13.
- Marazzi C, Wittauer M, Hirschmann MT, et al. Minimally invasive plate osteosynthesis (MIPO) versus open reduction and internal fixation (ORIF) in the treatment of distal fibula Danis Weber types B and C fractures. J Orthop Surg Res.2020; 15(1):491.




 Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.
Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.