LCP as MIPPO vs LCP as external fixator (supracutanoeus mode) in open grade 1 fractures of distal tibia: A comparison study from hills of northern India
Received: 24-Jun-2021 Accepted Date: Jul 18, 2021 ; Published: 30-Jul-2021, DOI: 10.37532/1897-2276.2021.16(1).29
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Introduction: Fracture to tibia is one of the most common fracture encountered in a career of an orthopaedic surgeon. Because of the often high energy involved and the precarious soft tissue cover that surrounds the distal tibia, such fractures command watchful attention to the soft tissue cover for timing and method of surgical fixation. In recent years, the concept of biological osteosynthesis has gained a reputation in fracture treatment. And in order to maintain biology of the fracture and to expedite the healing process many institutions and surgeons are using minimal invasive methods for distal tibial fixation. However till date no comparison is being made between the use of MIPPO and supracutaneous plating for distal tibial fractures. We are the first one to show our experience and results with these two biological methods in 40 cases of grade 1 Gustilo and Anderson fractures of distal tibia in a tertiary care centre situated in hilly terrain of northern India.
Methods: The present study was carried out in the department of Orthopaedics from 1.01.2019 to 1.06.2021. 40 patients in age >18 yrs who had Gustilo and Anderson type 1 fracture of distal Tibia of both sexes were enrolled in this prospective study done at Pt. Jawahar Lal Nehru Govt medical college Chamba, Himachal Pradesh. They were randomized into 2 groups of 20 each according to the day of admission. In one group (MIPPO) mippo was done in gustilo and Anderson grade 1 distal tibial fractures and in antoher group Supracutaneous plating was done (SCP). In each determined follow up at and after 6 weeks, clinical assessment of range of motion, radiological evaluation for progression of fracture healing and complications were documented. The functional outcome of the ankle was assessed with the help of AOFAS (American Orthopedic Foot and Ankle Society Ankle Score) and Teeny and Wiss criteria (symptoms and functional evaluation of ankle) at 12 months. Complications like surgical site infection, deep infection, delayed union, non-union and ankle stiffness were documented.
Results: We found no difference in the time to union in weeks in the two groups (SCP-21 months, MIPPO 20 months). However, operating time was significantly longer in the MIPPO group (97.9 vs 81.2 minutes, p<0.001, respectively). Patients who had SCP had Less pain and a better function, alignment and total AOFAS score than the MIPPO group. These results were statistically significant. There were more wound problems both superficial and deep infections in the MIPPO group. Total duration of stay was significantly shorter in SCP group {10 vs 22 days (inclusive of implant removal). Radiological outcome using Teeny Wiss radiological score was almost similar in both the groups. AOFAS Score including pain and function score was better in SCP group as compared to MIPPO group.
Conclusion: The high percentage of unions, the low rate of complications, comparatively less surgical time, easy implant removal and better functional scores suggest that using LCP in supracutanoeus mode can be a reasonable alternative to MIPPO for treating distal tibia fractures. Future prospective randomized studies may be able to clarify these issues.
Keywords
fracture of tibia, osteoarthritis, distal tibia, MIPPO
Introduction
Fracture to tibia is one of the most common fracture encountered in a career of an orthopaedic surgeon. Since it is a major weight bearing bone every 2 in 1000 individual has a fracture of tibia [1].
As long as the fracture is in diaphyseal region there is no major controversy. Historically undisplaced or mildly displaced fractures of shaft tibia have been managed conservatively with good union rates.
Problem arises when fracture is in distal tibia in metaphyseal area around the ankle joint.These fractures constitute about 10%-13% of all tibial fractures and are mostly associated with soft tissue injury [1].
Tibia Pilon fractures are caused mainly by an axial load on the tibia, usually due to high energy trauma which may have an associated rotational component [2]. Because of the often high energy involved and the precarious soft tissue cover that surrounds the distal tibia, such fractures command watchful attention to the soft tissue covers for timing and method of surgical fixation [3].
Many methods are available for the management of such fractures and extensive literature is available on these techniques.
These are plaster immobilization, traction, Open Reduction and Internal Fixation (ORIF) with plates, closed intramedullary, Minimally Invasive Plate Osteosynthesis (MIPO), and external fixation.
Non operative treatment is possible for stable fractures with minimal shortening, but malunion, shortening of affected leg, limitation of range of motion, and early osteoarthritis of the ankle have all been reported following treatment of these fractures particularly pilon fractures [4].
Classic open reduction and internal plate fixation require extensive soft tissue dissection and periosteal stripping even in expert hands, with high rates of complications, including infection (range, 8.3%-23%) [5,6] and delayed union and non-unions (range, 8.3%-35%).
There has been a constant thinking and evaluation to fix these fractures more biologically with indirect close reduction and applying stable fixation to achieve early union and maximal function.
In current orthopedic scenario two techniques have been extensively studied and also compared and various metanalysis are available. These are IMLN and minimal invasive plating osteosynthesis. Various authors and studies have shown different benefits and complication of one method over the other. These are the techniques most widely used nowadays for distal tibial fractures.
In recent years, the concept of biological osteosynthesis has gained a reputation in fracture treatment. And in order to maintain biology of the fracture and to expedite the healing process many institutions and surgeons are using Locking compression plate as an external fixator which is fondly called as supracutaneous plating [7-10].
The use of this technique was reported in literature as early as 1991, [11] but for two decades there were only sporadic reports with small number of patient’s series. In this technique the anatomical contoured LCP with angular stable screw is applied as an external fixator supracutaneously which maintains the stabilization without violating the biology of soft tissue.
However till date no comparison is being made between the use of MIPPO and supracutaneous plating for distal tibial fractures. We are the first one to show our experience and results with these two biological methods in 40 cases of grade 1 Gustilo and Anderson [12] fractures of distal tibia in a tertiary care centre situated in hilly terrain of northern India.
Materials and Methods
The present study was carried out in the department of Orthopaedics from 1.01.2019 to 1.06.2021. 40 patients in age >18 yrs who had Gustilo and Anderson type 1 fracture of distal Tibia of both sexes were enrolled in this prospective study done at Pt. Jawahar Lal Nehru Govt medical college Chamba, Himachal Pradesh. They were randomized into 2 groups of 20 each according to the day of admission. Consultants looking after Tuesday Thursday and Saturday performed MIPPO on these patients. Author looking after Monday Wednesday and Friday performed supracutaneous plating.
The patients were allocated a sequential study number and there were no exclusions after randomization. Patients with pathological fractures, non-osteoporotic osteopathies such as endocrine disorders, rheumatologic disorders, diabetes mellitus, renal disease, immunodeficiency states, mental impairment or difficulty in communication were excluded. Those with open fractures according to Gustilo and Anderson type II [12] or type III or fractures with a displaced intraarticular fragment were also excluded.
Approval for the study was given by the Ethics Committee of our hospital and informed consent was obtained from all patients before operation The patients were selected based on those satisfying the inclusion criteria and were followed up in Post-operative period immediately and for one year.
The distal tibia was defined as the area within two Müller squares of the ankle joint, in which the proximal and the distal segments of long bones are defined by a square whose sides have the same length as the widest part of the epiphysis [13].
The general data of patients are illustrated in Table 1.
|
Group |
||||||
|---|---|---|---|---|---|---|---|
Supracutaneous Plating |
MIPPO |
Total |
|||||
Count |
% |
Count |
% |
Count |
% |
||
Age |
<30 years |
7 |
35 |
6 |
30 |
13 |
32.5 |
31-45 years |
4 |
20 |
7 |
35 |
11 |
27.5 |
|
46-55 years |
7 |
35 |
4 |
20 |
11 |
27.5 |
|
>56years |
2 |
10 |
3 |
15 |
5 |
12.5 |
|
total |
20 |
100 |
20 |
100 |
40 |
100 |
|
Table 1. General data of patients
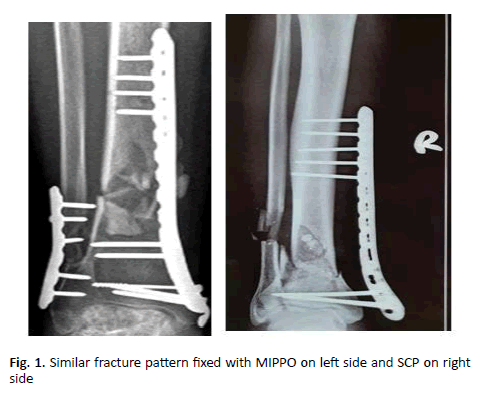
After Initial Toileting and debridement all patients were immobilized to relieve swelling. Intravenous antibiotics were started on admission and continued till 4th post operative day. Pneumatic tourniquets were used in both groups. Talar shift caused by an external rotation force was considered to be a sign of syndesmotic instability [5]. If syndesmotic instability was present the associated fibular fracture was fixed in both the groups (Figure 1).
Surgical Steps For Supracutaneous Plating
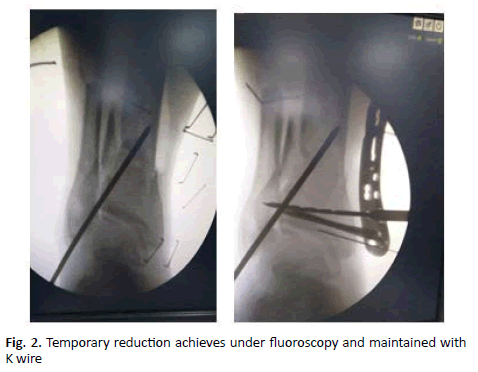
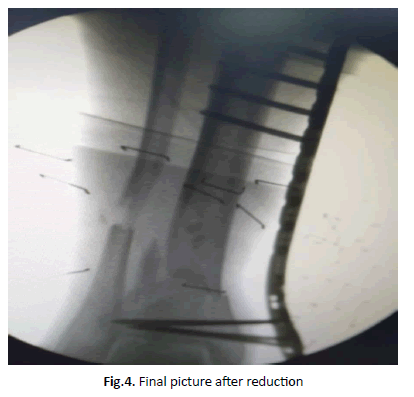
Fracture reduction is done prior to application of plate. LCP metaphyseal plate of appropriate length is chosen. The plate is initially fixed to the proximal and distal fragments with a k-wire after certaining fracture reduction under fluoroscopy guidance (Figure 2). LCP is placed as close to the bone as possible, yet still allowing some space for swelling and regular wound care, to increase the mechanical stability of fixation (Figure 3). It is separated from the skin surface by a spacer of uniform thickness. For the distal tibia, at least four screws proximally and three to four screws distally is recommended (Figure 4). Successive holes are drilled over locking drill-guides through stab incisions made over the intact soft tissue envelope and screws are placed first distally and later in proximal fragment after ensuing good reduction. Screw tract and wound dressing is done.
Steps For Mipo Technique
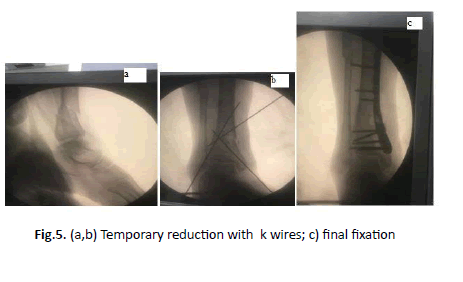
The patient was supine on the radiolucent operative table. An indirect reduction technique was carried out and alignment checked by fluoroscopy. Reduction was temporary stabilized with multiple k wires (Figure 5)
An anterior-medial curved incision (about 3 cm-6 cm), exposing and protecting the saphenous vein. A proximal incision was made under fluoroscope for at least 3 screws in the proximal fragment (Figure 6). A subcutaneous extraperiosteal tunnel was created and follows by the insertion of a plate from the distal to proximal incision. The plate was tunneled proximally across the fracture site using the locking sleeve as a handle for insertion of the plate [14,15].
The plate was centered on the tibia, confirmed on AP and lateral views; cortical screws were inserted first depending on the need for reduction in proximal or distal fragment. After the reduction was confirmed, locking screws were inserted with aim of achieving a minimum of 6 cortices on either side of the fracture. Wound dressing is done.
The duration of surgery was recorded from the incision to wound closure. Postoperatively, IV 2nd generation cephalosporins and aminoglycoside antibiotics were continued for 4 days followed by oral antibiotics for 5 days along with limb elevation, analgesics, antacids and trypsin chymotrypsin. Post operatively below knee posterior slab was given which was removed on second postoperative day and passive ankle range of motion exercises were initiated. Weight-bearing was restricted for 6 weeks.
Average stay in the hospital was recorded. Delayed wound healing and superficial infection were defined as persistent drainage from the wound for at least two days, or separation of wound edges to a width >1 cm and a length >1 cm [18].
Since implant removal in supracutaneous group was on outdoor basis no second surgery/hospital stay was needed. Stay for the subsequent implant removal in MIPPO group was added to total duration. Follow-up was done at 2 weeks, 6 weeks, 3 months and 6 months after discharge till the fracture united. In each determined follow up at and after 6 weeks, clinical assessment of range of motion, radiological evaluation for progression of fracture healing and complications were documented. The functional outcome of the ankle was assessed with the help of AOFAS (American Orthopedic Foot and Ankle Society Ankle Score) and Teeny and Wiss criteria (symptoms and functional evaluation of ankle) at 12 months. Complications like surgical site infection, deep infection, delayed union, non-union and ankle stiffness were documented. The radiological outcome was assessed using the Teeny-Wiss scoring system and fracture union [19]. Fracture union was subject to radiographic evidence of union and pain-free weight bearing.
Results
Data collected from the study of 40 cases; with follow up range from 6-24 months (mean 15 months) and results were recorded; it was evaluated for demographic, injury characteristics, functional outcome, radiological outcome and complications.
In SCP Group, majority of subjects were in the age group <30 years and 31 to 45 years (35%) respectively and in MIPPO group majority of subjects were in the age group 31 to 40 years (35%). There was no difference in age distribution between two groups (Table 1).
In our study 13 patients had associated bony injuries- femur (2), rib fracture (2), patella (1), head injury (2), humerus (1), forearm (2), IT(1) and ilium (2)
We found no difference in the time to union in weeks in the two groups (SCP-21 months, MIPPO 20 months). However,operating time was significantly longer in the MIPPO group (97.9 vs 81.2 minutes, p<0.001, respectively).
Patients who had SCP had less pain and a better function, alignment and total AOFAS score (Table 2) than the MIPPO group .These results were statistically significant.
| SCP * | MIPPO† | P value | |
|---|---|---|---|
| Mean (95% CI‡) operating time in minutes | 81.23 (77.72 to 84.73) | 97.9 (94.76 to 100.95) | 0.001 |
| Mean (95% CI) time to union in weeks | 21(14-28) | 20(12-28) | 0.54 |
| Patients with wound problems (%) | 3(15) | 6(30) | < 0.05 |
| AOFAS§ mean (95% CI) score at one year | 86.1 (83.7 to 88.6) | 83.9 (81.7 to 86.1) | < 0.05 |
| Pain | 32.5 | 30.5 | < 0.05 |
| Function | 44.3 | 42.2 | < 0.05 |
| Alignment | 9.1 | 9.1 | <0.05 |
| Teeny and Wiss criteria (symptoms and functional evaluation of ankle) | |||
| Excellent | 18(80%) | 14(65) | <0.05 |
| Good | 2(20%) | 3(15) | >0.05 |
| Fair | 3(15) | - | |
| Duration of hospital stay (including implant removal) | 10 (6-14) | 12(8-16)+ 10(6-14) | |
*SCP: Supracutaneous Plating
† MIPPO: minimal invasive plating osteosynthesis
‡ CI: confidence interval
§ AOFAS: American Orthopaedic Foot And Ankle Surgery
Table 2. Alignment and total AOFAS score of patients
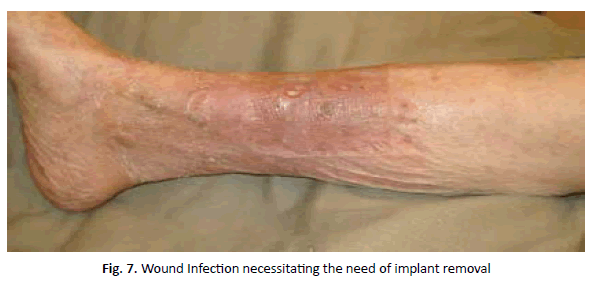
There were more wound problems both superficial and deep infections in the MIPPO group. 2 patients in MIPPO group had deep infections. One had infection before fracture union so implant has to be removed and debrided thoroughly (Figure 7). Antibiotic beads were inserted and supracutaneous plate was applied for stabilization. After settling of infection, bone grafting and supracutaneous plating was done (Table 3).
| Group | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Supracutaneous Plating | MIPPO | Total | P value | ||||||
| Count | % | Count | % | Count | % | ||||
| Superficial Infection | yes | 3 | 15 | 4 | 20 | 7 | 17.5 | 0.012 | |
| No | 17 | 85 | 16 | 80 | 33 | 82.5 | |||
| Deep Infection | yes | 0 | 0 | 2 | 10 | 2 | 10 | 0.013 | |
| mo | 20 | 100 | 18 | 90 | 38 | 90 | |||
| Non-Union | yes | 0 | 0 | 0 | 0 | 0 | 0 | 0.14 | |
| no | 20 | 20 | 20 | 20 | 40 | 100 | |||
| Malunion | yes | 1 | 5 | 1 | 5 | 2 | 5 | 0.147 | |
| no | 19 | 95 | 19 | 95 | 38 | 95 | |||
| Delayed union | no | 0 | 0 | 2 | 10 | 2 | 5 | ||
| yes | 20 | 100 | 18 | 90 | 40 | 95 | |||
Table 3. Details of bone grafting and supracutaneous plating
One patient in MIPPO group developed cellulitis and one another developed wound dehiscence.
A total of 18 (90%) patients in LCP group had wished to have the implant removed (Table 3). Only two patients decided against removal. Several factors contributed to the decision for removal, principally prominence of the plate at its distal end and pain.
Total duration of stay was significantly shorter in SCP group {10 vs 22 days (inclusive of implant removal) } (Table 2)
According to the Teeny and Wiss criteria 18 patients (80%) had excellent/good outcome in SCP group whereas 14 (65%) patients had good outcome in MIPPO group. Three cases with complications in MIPPO Group had fair outcome (Table 2).
AOFAS Score including pain and function score was better in SCP group as compared to MIPPO group.
Radiological outcome using Teeny Wiss radiological score was almost simila in both the groups (Table 4).
|
Supracutaneous Plating |
MIPPO |
||
|---|---|---|---|---|
No of Cases |
Percentage |
No of cases |
Percentage |
|
Radiological Outcome |
|
|
|
|
Anatomical |
15 |
75 |
16 |
80 |
good |
3 |
15 |
2 |
10 |
fair |
2 |
10 |
2 |
10 |
poor |
0 |
0 |
0 |
0 |
Table 4. Radiological outcome using Teeny Wiss radiological score
Discussion
Controversy is still present about the surgical merits of the different lines for treating distal tibia fractures; decision making is difficult, and no best treatment has been determined.
It is the precarious soft tissue around the distal tibia that dictates the choice of reduction technique, choice of implant and mode of application of the implant so as to provide minimum insult to already depleted blood supply.
In the meta-analysis done by Wang et al. [16] in 2019 of MIPPO versus IMN for distal tibial fractures, 13 RCTs with 924 patients were included. Compared with MIPPO, IMN was associated with less operation time and time to reunion. MIPPO significantly increased the rate of wound complications and the overall rate of union complications and deep infections were similar between the two groups. Similar functional outcomes were observed when evaluating the outcomes by AOFAS.
Many studies have shown good results of locked plating with MIPO technique in distal tibial fractures with complication rates comparable to intramedullary nailing [20,21]. However, a few studies in recent literature have shown a high rate of soft tissue complications associated with the use of locked plates in distal tibial fractures [22].
Kerkhoff et al. used Lcp as external fixator and found that a standard AO-plate as an external fixator is an elegant alternative in exceptional situations. This method is convenient for the patient and always available. Using commonplace equipment, it is relatively easy to provide stable fixation [8].
So since newer studies are coming with high complication rates attributed to most commonly use procedure (MIPPO) in distal tibial fractures, and also emerging of literature regarding use of LCP in supracutaneous mode for distal tibial fractures we decided to compare these two methods of fixation in our study.
To the best of our knowledge, no previous prospective study has been performed to compare these two methods.
In our study all the fractures in both groups went into union. However in MIPPO group one case had deep infection before fracture union which necessitated implant removal and secondary surgeries.
Average union occurred at 21 weeks for SCP group and 20 weeks for MIPPO group. In our study union occurred earlier than MIPPO group in studies done by Cory Collinge et al. [23] (27 weeks) and Abidmushtaq et al. [24] (24 weeks).
One significant finding in our study was higher operative time in MIPPO group 97.9 minutes’ vs 81.2 in SCP Group. This is due to need of creating proximal and distal entry ports and also time taking in suturing them back. This is in Accordance to Guo et al. [18] who concluded that surgical time is more in their MIPPO group vs IMLN group.
There were more wound problems both superficial and deep infections in the MIPPO group. 2 patients in MIPPO group had deep infections. One had infection before fracture union so implant has to be removed and debrided thoroughly (Figure 7). Antibiotic beads were inserted and supracutaneous plate was applied for stabilization. After settling of infection bone grafting and supracutaneous plating was done (Table 3).
Incidence of deep infection was 10% in MIPPO group while no deep infection was seen in SCP group. This is in Accordance with a study conducted in Hong Kong, China [24], reported a late infection rate of 15% in patients undergoing MIPPO fixation for distal tibial fractures, and the implant was removed in 52% of patients due to skin impingement. Moreover, in the present study, MIPPO was associated with a longer operative time, due to complicated indirect reduction techniques of MIPPO. A minimal incision cannot ensure minimal invasion because surgeons who are unfamiliar with the technique may repeatedly insert and pull out the plate, which will induce a dead space and increase infection risk or delayed union. Therefore, overall preoperative evaluation of the risks to soft tissue is very important, especially for those with high energy injury.
Another highlight or benefit of using SCP is that Implant removal can occur as an outdoor procedure and no need for addition hospital stay or admission is required for implant removal surgery. This is of paramount importance in developing countries like India especially in our teaching institution which is situated in one of the 115 backward districts of India. This tremendously brings down the cost factor associated.(Table 5).
| Removal | SCP* (%) | LCP† (%) |
|---|---|---|
| Yes | 20(100) | 10(50) |
| Subject to doctor’s decision | 8 (40) | |
| NO | 2(10) |
Table 5. Implant removal Questionnare
90 percent of patients treated with MIPPO technique subsequently had removal of implant. Lau et al. [25] reported a rate of late infection of 15% in MIPO fixation of a locking plate in distal tibial fractures and 52% of their patients had the implant removed because of skin impingement. Our study also showed that pain caused by impingement of the implant on the skin was common cause for implant removal. Another reason in our population of tribal areas was the constant pressure by attendants and their relatives due to a superstition that implant present in their body can cause cancer.
AOFAS Score including pain and function score was better in SCP group as compared to MIPPO group. This signifies better functional outcome and better range of motion in patients operated with SCP plating. According to Teeny and Wiss criteria 18 patients (80%) had excellent/good outcome in SCP group whereas 14 (65%) patients had good outcome in MIPPO group. Collinge et al. [18] reported the only variable that influenced functional outcomes was the occurrence of a secondary surgery (34% of patients), which was associated with poor function results. This can be a reason for poor functional outcome in MIPPO group as 2 patients had secondary surgery and also 90% of MIPPO group Patients got their implant removed.
Radiological outcome using Teeny Wiss radiological score was similar in both SCP and MIPPO group which is comaparable to various mentioned studies [18,23,24]. In our study, no fixation loss or implant failure was encountered.
Conclusion
Given the small numbers of patients in our study, we cannot draw any definitive conclusions. The high percentage of unions, the low rate of complications, comparatively less surgical time, easy implant removal and better functional scores suggest that using LCP in supracutanoeus mode can be a reasonable alternative to MIPPO for treating distal tibia fractures. Future prospective randomized studies may be able to clarify these issues.
Conflict of Interest
The authors declare that they have no relevant financial or non-financial interests to report.
Funding
This research did not receive any specific funding.
Ethical Approval
Ethical approval was not required.
Informed Consent
Written informed consent was obtained from all patients and/our families.
REFERENCES
- Bucholz RW, Heckman JD, Court-Brown CM. Rockwood & Green's fractures in adults. 6th edn. Philadelphia: Lippincott Williams & Wilkins 2006.
- Egol KA, Wolinsky P, Koval KJ. Open reduction and internal fixation of tibial pilon fractures. Foot Ankle Clin [Internet]. 2000; 5(4):873-85. Available from: http://www.ncbi.nlm.nih.gov/pubmed/11232473
- Bonar S, Marsh J. Tibial Plafond Fractures: Changing Principles of Treatment. J Am AcadOrthop Surg [Internet]. 1994; 2(6):297-305.
- Sarmiento A, Latta LL. 450 closed fractures of the distal third of the tibia treated with a functional brace. Clin OrthopRelat Res. 2004;428:261–271.
- Im GI, Tae SK. Distal metaphyseal fractures of tibia: a prospective randomized trial of closed reduction and intramedullarynail versus open reduction and plate and screws fixation.J Trauma. 2005;59:1219–1223;
- Janssen KW, Biert J, van Kampen A. Treatment of distal tibial fractures: plate versus nail: a retrospective outcome analysis of matched pairs of patients. Int Orthop. 2007;31:709–714.
- Yang SW, Tzeng HM, Chou YJ, Teng HP, Liu HH, Wong CY. Treatment of distal tibial metaphyseal fractures: Plating versusshortened intramedullary nailing. Injury. 2006;37:531–535.
- Kerkhoffs GM, Kuipers MM, Marti RK, Van der Werken C. External fixation with standard AO-plates: technique, indications, and results in 31 cases. J Orthop Trauma. 2003 Jan;17(1):61-4.
- Kloen P. Supercutaneous plating: use of a locking compression plate as an external fixator. J Orthop Trauma. 2009 Jan;23(1):72-5.
- Woon CY, Wong MK, Howe TS. LCP external fixation—external application of an internal fixator: two cases and a review of the literature. J Orthop Surg Res. 2010;20(5):19.
- Marti RK, van der Werken C. he AO-plate for external fixation in 12 cases. Acta Orthop Scand. 1991 Feb;62(1):60-2.
- Gustilo RB, Anderson JT.Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones: retrospective and prospective analyses. J Bone Joint Surg [Am] 1976;58-A:453-8.
- Mauffrey C, McGuinness K, Parsons N, et al. Arandomised pilot trial of "locking plate" fixation versusintramedullary nailing for extra articular fractures of thedistal tibia. J Bone Joint Surg Br 2012;94(5):704-708
- Apivattahakakul T, Khong S. Tibia KS, Shaft F. In: Tong G, Bavonratanavech S, editor. AO manual of fracture management. Minimally invasive plate osteosynthesis (MIPO). Concepts and cases presented by AO East Asia. Stuttgard New York: Georg ThiemeVerlage; 2006. p. 208-302.
- Bavonratanavech S. Instruments. In: Tong G, Bavornatanavech S, editors. AO manual of fracture management. Minimally invasive plate osteosynthesis (MIPO). Concepte andcesea presented by AO East Asia. Stuttgart New York: GeorgThieme Verlag; 2006. p. 20-9.
- Wang B, Zhao Y, Wang Q, Hu B, Sun L, Ren C, Li Z, Zhang K, Hao D, Ma T, Lu Y. Minimally invasive percutaneous plate osteosynthesis versus intramedullary nail fixation for distal tibial fractures: a systematic review and meta-analysis. J Orthop Surg Res. 2019 Dec 21;14(1):456.
- Minhas SV, Ho BS, Switaj PJ, Ochenjele G, Kadakia AR. A comparison of 30-day complications following plate fixation versus intramedullary nailing of closed extra-articular tibia fractures. Injury. 2015;46:734–739.
- Guo JJ, Tang N, Yang HL, Tang TS. A prospective, randomized trial Comparing closed intramedullary nailing with percutaneous plating in the Treatment of distal metaphyseal fractures of the tibia. J Bone Joint Surg Br. 2010; 92(7): 984-8.
- Teeny SM, Wiss DA. Open reduction and internal fixation of tibial plafond fractures. Variables contributing to poor results and complications. Clin OrthopRelat Res. 1993; (292):108-17
- Bingol I, Yalcin N, Bicici V, Tulunay T, Yuksel K, Kilicarslan K. Minimally invasive percutaneous plate osteosynthesis does not increase complication rates inextra-articular distal tibial fractures. Open Orthop J. 2015;9:73–77.
- Viberg B, Kleven S, Hamborg-Petersen E, Skov O. Complications and functional outcome after fixation of distal tibia fractures with locking plate—a multicentre study. Injury. 2016;47:1514–1518.
- Mushtaq A, Shahid R, Asif M, Maqsood M. Distal tibial fracture fixation with Locking Compression Plate (LCP) using the Minimally Invasive Percutaneous Osteosynthesis (MIPO) technique. Eur J Trauma Emerg Surg, 2009.
- Collinge C, Kuper M, Larson K, Protzman R. Minimally invasive plating of high-energy metaphyseal distal tibia fractures. J Orthop Trauma, 2007.
- Nork SE, Schwartz AK, Julie A, Holt SK, Schrick JL, Winquist RA. Intramedullary nailing of distal metaphyseal tibial fractures. J Bone Joint Surg Am Vol. 2005;87:1213.
- Lau TW, Leung F, Chan CF, Chow SP. Wound complication of minimally invasive plate osteosynthesis in distal tibia fractures. Int Orthop2008;32:697-703.





 Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.
Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.