Limb preservation for osteosarcoma of femoral condylar: a clinical case of total knee replacement with microsurgical anterolateral thigh flap transfe
2 Saint Paul Hospital, Hanoi, Vietnam
3 Vietnam National Cancer Hospital, Hanoi, Vietnam
Received: 06-May-2020 Accepted Date: May 25, 2020 ; Published: 03-Jun-2020
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: Osteosarcoma is a high malignancy, early metastasis, and often leading to disability or limb amputation. Today, advances in science, technics, and materials, especially in joint replacement and reconstructive surgery with free flap transfer, open up hope for cancer patients in general, and bone cancer in particular about the preservation of limbs.
Case report: A 23-year-old woman with sarcoma of the right distal femur was undergone tumor resection and cement replacement one year ago. This time the patient was admitted to the hospital for a painful swollen right knee. She was diagnosed with recurrent femoral osteosarcoma. Additional wide resection of the tumor along with total knee replacement and pedicled medial gastrocnemius muscle flap for covering soft tissue defect was done. Two weeks after this operation, the muscle flap was necrosis, we decided to use an anterolateral thigh flap to cover soft tissue. Follow up 3 months after surgery showed good knee movement function: 90 degrees flexion, completely normally walking and painless.
Conclusion: In the surgical treatment of bone cancer, total joint replacement surgery combined with reconstructive technics is helpful to preserve the limb of patients. If complex cases where local flaps do not enough for covering, the Anterolateral Thigh (ALT) flap is a good choice to combine with a total joint replacement for preserving patients’ extremities
Keywords
Osteosarcoma, total knee arthroplasty, anterolateral thigh flap, pedicled gastrocnemius muscle
Introduction
Bone cancer is derived from mesenchymal cells and is the most common primary bone malignant disease [1]. Among childhood cancers, bone cancer ranks 8th in overall incidence. Bone cancer is common in two age groups: preadolescence (10-14 years) and late adulthood (>65 years). The most common place for bone cancer is “near the knee, far from the elbow”. Combinate chemotherapy treatment significantly improved the over-5-year patient’s extra-survivability reached 67.9%. Studies have so far found that limb conservation or amputation does not affect the patient’s extra time [2]. Therefore, limb preservation in bone cancer is increasingly widespread. Especially in developed countries, in which surgery is the most important role in preserving limbs for patients.
Surgery for bone cancer usually consists of cutting off widely the tumor, the cutting distance from the tumor margin is greater than 2 cm as measured on Magnetic Resonance Imaging (MRI) film, ensuring the cutting section is free of malignant cells [3,4]. After extensive resection of the tumor, it is necessary to preserve the limbs both in form and function, which require techniques to reconstruct bones, joints, and covering soft tissue. Methods to replace bone and joint structure: autograft, allograft, biological material grafting, total joint replacement with a long stem, etc. For covering soft tissue, with cases of not too complicated lesion, the majority of authors use adjacent muscle and skin flaps to help cover lesions, joints, or artificial bones. With lesion at the knee, authors often choose gastrocnemius muscular flap, combined with skin grafting. However, in cases of soft tissue invading tumors with too large lesions, a greater source of the material is required or when the gastrocnemius muscular flap fails, the microsurgical flap begins to be expected to help preserve the limb for the patient.
In Vietnam, the amputation rate in the treatment of bone cancer is still very high. Thanks to the improved facilities and qualifications, we have made significant progress in limb conservation surgery. In this article we would like to introduce a clinical case: Total knee joint replacement in combination with microsurgical plastic surgery to treat femoral cancer. This is an experience in the process of diagnosing, treating, and monitoring patients with bone cancer.
Case Report
In Female, age 23, history: knee traumatism one year ago without treatment. The patient was examined at another hospital because the swelling and pain of the right knee was gradually increased. Diagnosed: Giant cell tumor, pathologic surgical result was Osteosarcoma. Patients have undergone a tumor resection surgery, cement inserts. Postoperative adjuvant chemical treatment with 3-phase EOI regimen. The patient responded well, stable for the next 1 year.
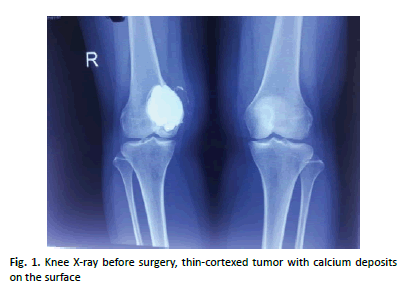
This time, the patient came to us because of pain, and swelling at the old tumor appeared, gradually increasing over the last 1 month. MRI of the right knee: tumors with clear boundaries, invading the localized soft tissue at the right knee medial, diagnosis: recurrent femur cancer (Fig. 1).
Female patients, young, recurrent tumors after one year, quite good chemical response, so conservative treatment is chosen. The question in treating cancer is the extensive cutting of both bone structure and surrounding invasive soft tissue. We expected to cut most of the right distal femoral and the extensive soft tissue defect is planned to be covered by pedicled medial gastrocnemius muscle flap.
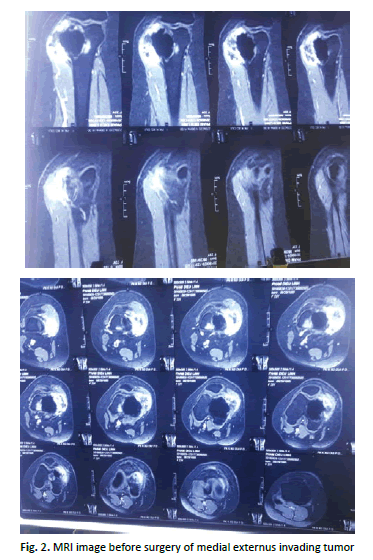
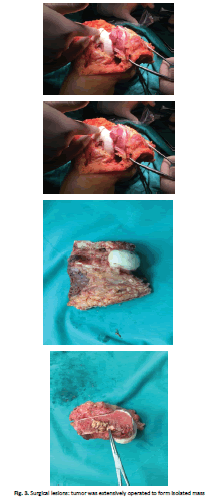
The orange segment incision is made through the tumor surface in the right medial face, coinciding with the inside way of the extended knee joint. Separate the skin flap to both sides of the right thigh tumor. Tumor releasing removal, cutting the soft tissue > 2 cm from the tumor, cutting the right distal extremity of femur, cut the first segment under the right femur. Cutting all the bony segment containing the tumor and the surrounding soft tissue forming a mass, following the principle of not touching the tumor (Fig. 2 and 3).
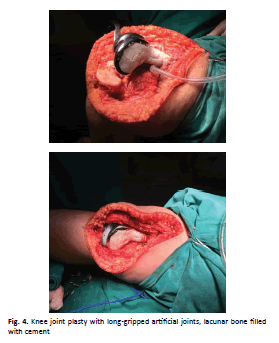
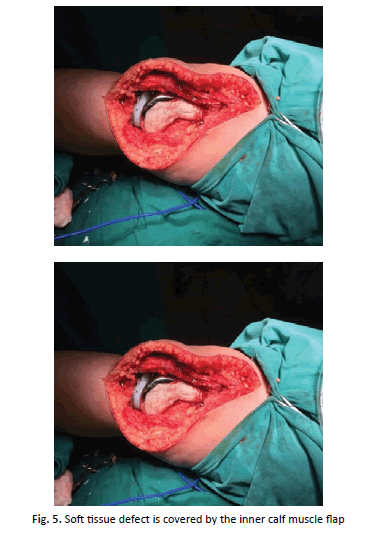
We biopsied bone resection, bone marrow, and the remaining soft tissue section in surgery, the result: negative. Then, we replaced long-gripped artificial knee joints and shaped lacunar bone with cement. After that, the medial gastrocnemius muscle flap was used to cover the soft-tissue defect (Fig. 4 and 5).
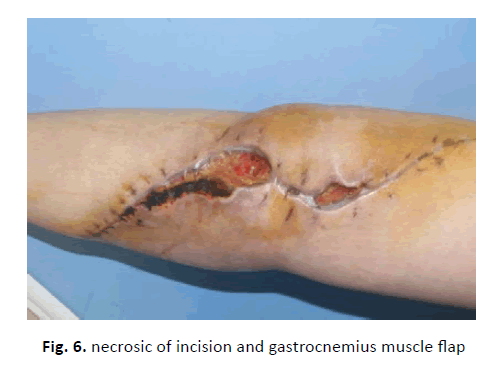
However, seven days after surgery, the surgical site showed discharge of reddish-brown fluid and slowly healing. A week later, the muscle flap was necrotic and a part of the prosthetic joint was exposed (Fig. 6).
The wound was washed by Dakin solution every day for 5 day and antibiotic treatment was restarted.
2nd Surgery: Covering the Prosthetic Knee Joint With Alt Flap
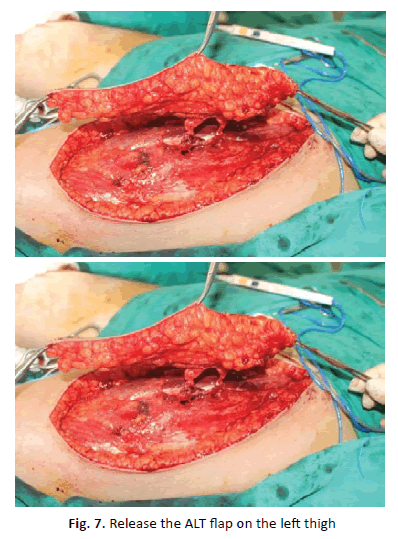
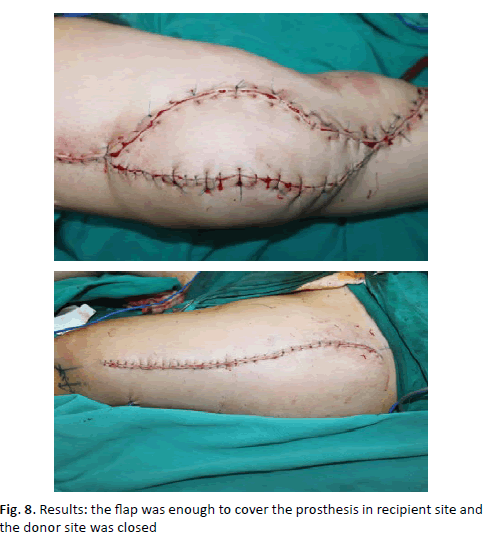
While reopening the surgical site, we saw that the gastrocnemius muscle flap covering the joint was necrotic. After removing the necrotic muscle flap and cleaning the joint cavity, leaving a defect in the inner knee region (R) to reveal an artificial joint measured 17 cm × 5 cm. An ALT flap was designed in the left medial thigh area with a size of 21 cm × 7 cm. Two perforators were located by using a handheld Doppler. The flap was dissected as a fasciocutaneous flap with two-centimeter thickness. Vascular pedicle from the descending branch of the lateral circumflex femoral artery, its length of 10 cm, and composed 2 musculocutaneous perforators. The flap was transferred to the receiving site to cover the exposed prosthetic of the knee joint. The artery and vein of the flap were anastomosed to the popliteal artery and vein. The donor site was directly closed (Fig. 7 and 8).
After the surgery, the flap survived, without necrosis or undernourishment, enough to cover the artificial knee joint. Practice passive knee flexion after 10 days, the patient exercised to walk in the straight knee with a support brace a week after surgery. 3 weeks after surgery, the skin flap was completely alive, the incision was well healed, suture cut off. Examination for 3 months after surgery performed good knee movement function: flexion of 90 degrees, walking completely normal, painless.
Discussion
Bone cancer is common in children, especially during puberty. High malignancy and early metastasis, is often in position “near the knee, far from the elbow”. The combination of multiple modalities in treating bone cancer, of surgery and chemotherapy significantly increases the extra-survival rate of patients. Formerly, the bone cancer surgery was mostly amputated, recently with the advancement in science the amputation is reduced, conservation rate is increased. In developed countries up to 80% of patients have conservation surgery. However, in Vietnam, the rate of conservation is low, the rate of amputation is still high. To ensure the most effective treatment, a cancer treatment plan is essential. Despite small initial lesions, surgery should not be performed by resection, although the cancer cells can be removed by a general assessment, the cancer cells can be spread out to surrounding soft tissue. Previous chemical treatment is essential to help shrink, necrose the tumor, and prevent metastases. However, it is necessary to have surgery to remove extensively the tumor, considered radical surgery. This patient is not treated as such, so the tumor recurs early and invades the surrounding soft tissue. According to author Wei Zhu et al., when studying 13 patients with a hip replacement and 3 patients with knee replacement due to a tumor of joint facet head, the author concluded that joint replacement is a safe and effective method for tumor at the bone head, spreading to the joints if the patient complies with the treatment regimen [5]. According to Levasic, studying on 8343 patients with joint replacement within 22 years, the authors concluded that the risk of cancer in patients with joint replacement is equal to the one in the community, meaning joint replacement does not increase the risk of cancer [6]. The required surgery for this patient is the extensive surgery to cut the tumor including the soft tissue and the bone. About the joint, we expected to replace the total knee joint with constrained implants, gap plasty with cement. During the surgery, we evaluated trying to conserve a part of the lateral condyle, helping to prevent rotation. It results in a good joint function.
However, according to the study of author Karam when studying 26415 patients with cancer being indicated a joint replacement, the author concluded that joint replacement increases the risk of surgical complications [7]. In this case, we have carefully followed the patient from before, during, and after surgery, she was completely healthy, no metastasis detected.
Discussion of Anterolateral Thigh Flap
After extensive removal of both bone and soft tissue to eliminate cancer formation for a total knee replacement, covering the defect and the prosthetic by a sufficient and well blood supplied source of the material is very important. The first option chosen by many authors is the vascular muscular flap, such as soleus muscle flap, or gastrocnemius muscle flap, due to its simplicity [8]. In this case, the initial choice was a gastrocnemius muscle flap. However, flap necrosis leads to ragged surgical incision. The reason was supposed that both the origin and insertion of the muscle had been cut with the tension of the closure leading to the pinched flap, anemia, and muscle necrosis, especially on the background of a patient undergoing chemotherapy, and changed vascular system also leading to muscular necrosis oligotrophy. Infection was not the main cause. Most of the authors used the opposite gastrocnemius muscle flap and in combination with skin grafts help reduce tension to increase the viability of the soleus muscle flap. In this case, if there was no well-vascularized tissue to cover the joint, it is very easy to lead to infection and have to remove the artificial joints and amputate lower extremity. The microsurgical flap is taken into account. Several free flaps have been mentioned in covering the soft tissue defects after knee replacement such as the anterolateral thigh flap, latissimus dorsi flap, the lateral arm skin flap [9]. In which the lateral arm skin flap is rarely used due to the short pedicle and the limited tissue volume, and the latissimus dorsi flap has the disadvantage of having to change the patient’s position during surgery. The anterolateral thigh flap was firstly introduced by Song et al in 1984, since then it has been used extensively in plastic surgery for various types of injuries, most of which are head, face, and neck cancer. With knee lesions due to bone or soft tissue cancer, some authors had reported clinical cases using ALT flap for difficult cases. Cécile Philandrianos reported 3 clinical cases of knee joint infection after total knee replacement in patients with osteosarcoma [10]. In these cases, the author used the ALT flap at the second surgery when revision total knee replacement. The author also found that the flap has a good vitality to meet the needs of covering the artificial joints. Miyamoto also described the case of using the ALT flap to cover the knee defect, while using the descending branch of the lateral femoral circumflex artery to regenerate the popliteal vessels that were also damaged by the sarcome [11]. Chien et al. described a complex case of knee injury due to cancer who had a joint replacement surgery with the use of ALT thigh flap [12]. In this case, because the vascular system in the knee joint was much damaged when the tumor was removed, the author used the receiver vessels to be the descending branch of the lateral femoral circumflex artery in the reverse pattern. The author argued that using the recipient artery farther away from the tumor site will be safer for the vascular connection, and avoiding damage to the blood supply to the distal limb. In our case, the lesion is large because the tumor invades the soft tissue, the gastrocnemius muscle flap used at the first operation failed, so the microsurgical flap was almost the last option to preserve the limb. The flap is taken from the opposite thigh and anastomosed to the femoral artery to ensure good blood pressure. The flap completely survives and covers the prosthesis. The flap is not stretched in the movements of the knee joint so that the range of movement of the knee joint is not limited. As with is providing a large source of material with good vitality, that can be used very flexibly, and can be taken with muscle if need to fill the gap. The long pedicle helps the flap easier to anastomose to healthy recipient vessels. The donor site can be closed directly, and scars will be wellhidden with clothes. This is a good option for cases of the extensive knee and popliteal lesion after cancer surgery. The combination of total knee replacement increases the chances of preserving extremity for the patients, especially for very young patients.
Conclusion
Bone cancer is a very common malignancy in young people, especially at puberty. These lesions previously were most indicated to be amputated, limb conservation is very limited, which has a serious impact on the daily activities and psychology of patients. With the development of chemicals, joint replacement surgery, and soft tissue reconstruction with plastic methods help increase the ability to preserve limbs for patients. In particular, the use of the microsurgical anterolateral thigh combined with joint replacement is a good choice for complex cases of much soft tissue invading tumor, where the local flaps are not appropriate.
Compliance with Ethical Standards
Funding
This study does not receive funding from any organization.
Conflict of Interest
The authors have no conflict.
Ethical Approval
Ethical approval has been granted in this study.
Informed Consent
The consent and commitment were signed by the patient.
REFERENCES
- Sobti A., Agrawal P., Agarwala S., et al.: Giant cell tumor of bone- an overview. Arch Bone Jt Surg. 2016;4:2-9.
- Anderson M.E.: Update on Survival in Osteosarcoma. Orthop Clin North Am. 2016;47:283-292.
- Tiwari A.: Current concepts in surgical treatment of osteosarcoma. J Clin Orthop Trauma. 2012;3:4-9.
- Pakos E.E., Nearchou A.D., Grimer R.J., et al.: Prognostic factors and outcomes for osteosarcoma: an international collaboration. Eur J Cancer. 2009;45:2367-2375.
- Zhu W., Ma Q., Bian Y., et al.; Total hip/knee arthroplasty in the treatment of tumor-induced osteomalacia patients: More than 1 year follow-up. Plos One. 2017;12.
- Levasic V., Milosev I., Zadnik V.: Risk of cancer after primary total hip replacement: The influence of bearings, cementation and the material of the stem. Acta Orthop. 2018;89:234-239.
- Karam J.A., Huang R.C., Abraham J.A., et al.: Total joint arthroplasty in cancer patients. J Arthroplasty. 2015;30;758-761.
- Cetrulo Jr C.L., Shiba T., Friel M.T., et al.: Management of exposed total knee prostheses with microvascular tissue transfer. Microsurg. 2008;28:617-622.
- Moebius B., Scheller E.E.: The pediculated gastrocnemius muscle flap as a treatment for soft tissue problems of the knee-indication, placement and results. GMS Interdisciplinary Plastic and Reconstructive Surgery DGPW. 2012;1.
- Philandrianos C., Mattei J.C., Rochwerger A., et al.: Free antero-lateral thigh flap for total knee prosthesis coverage after infection complicating malignant tumour resection. OTSR. 2018;104:713-717.
- Miyamoto S., Fujiki M., Nakatani F., et al.: Free flow-through anterolateral thigh flap for complex knee defect including the popliteal artery. Microsurg. 2015;35:485-488.
- Chien W.H., Chen I.C., Tan T.S., et al.: Salvage of knee joint tumor prosthesis using turnover reverse-flow descending branch of lateral circumflex femoral artery as recipient vessel for the free ALT flap: a case report. J Reconstr Microsurg. 2007;23:505-509.



 Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.
Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.