Maximum surgical blood ordering schedule for common orthopedic surgical procedures in a tertiary hospital in North Central Nigeria
2 Orthopedic Unit, Department of Surgery, General Hospital, Ilorin, Nigeria
Received: 21-Dec-2017 Accepted Date: Jan 08, 2018 ; Published: 10-Jan-2018
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: Blood transfusion is an important part of management of patients undergoing orthopedic surgeries. However frequently perioperative anticipated blood requirements overshoot the actual need resulting in unnecessary cross matching of blood. Therefore, it is important to formulate a maximum surgical blood ordering schedule (MSBOS) for common orthopedic surgeries.
Objective: To evaluate our blood utilization in various orthopedic surgeries and to develop a blood ordering schedule for various orthopedic surgeries.
Methodology: A 12-month (January-December 2016) retrospective study was carried out on patients undergoing orthopedic procedures. Data collected included number of patients transfused, number of units cross-matched and number of units transfused. The cross matched to transfusion ratio (CTR), transfusion probability and transfusion index were calculated and from the calculated values a MSBOS was proposed.
Results: A total of 224 units of blood were cross matched for 105 patients out of which only 97 units of blood was transfused to 55 patients. Nine out of 15 surgical procedures had CTR higher than 2, 4 had a low TI <0.5 and 12 had a blood utilization of <50%. Fracture of the forearm, total knee replacement (unilateral), tibiofibular and ankle fractures all had blood utilization of <30% and thus Type & Screen policy was recommended for these procedures.
Conclusion: The overall CTR was high with low percentage blood utilization and resultant significant blood wastage. To prevent unnecessary blood wastage, we suggest the implementation of the recommended MSBOS schedule.
Keywords
Blood transfusion, Orthopedic surgeries, Cross-matched to transfusion ratio (CTR), MSBOS
Introduction
In the United States, it is estimated that 24 million blood and products are used for the sick and injured yearly [1]. Chiavetta et al. [2] reported that over 31% of blood is utilized by the cardiac and orthopedic surgeons. Therefore, blood transfusion is an important part of management of patients undergoing orthopedic surgeries either as an elective or emergency procedure [3]. However, perioperative anticipated blood requirement and placement of blood request frequently overshoots the actual need thus resulting in unnecessary cross-matching of blood [4]. This imposes inventory problems for blood banks, financial loss to the patients, results in loss of shelf life and wastage of blood [5]. In South Africa 7% to 10% of blood is wasted annually due to over ordering of blood [6]. Despite all of these, there is very little literature on the utilization of blood in orthopedic and trauma surgery [3].
The cross-match to transfusion ratio (CTR), the transfusion index (TI), transfusion probability and blood utilization when used, are reliable indicators of accuracy of preoperative estimation of transfusion for a patient undergoing a surgical procedure. The (TI) is important in formulating the maximum surgical blood ordering schedule (MSBOS). MSBOS is a table of surgical procedures with the number of units of blood routinely cross-matched preoperatively. The implementation of MSBOS by Chawla et al. [7] resulted in about 60% reduction in cost to the patients. Hardy et al. [8] also found 35% reduction in the number of blood units crossmatched for elective surgical procedures after introducing MSBOS.
In our institution, we lack a policy on MSBOS. Therefore, our objective was to evaluate our blood utilization in various emergency and elective orthopedic surgeries, and to develop a blood ordering schedule for various orthopedic surgical procedures in our Centre.
Materials and Methods
This is retrospective analysis of medical records, anaesthetic records and blood transfusion records of all patients admitted between January 2016 and December 2016, who had orthopedic surgeries. Demographic data collected include age and sex. Other data collected were: type of surgery, elective or emergency, preoperative packed cell volume (PCV), estimated blood loss and postoperative PCV. For each orthopedic surgical procedure, we calculated the total number of patients, number of patients transfused, number of units cross-matched, and number of units transfused.
The cross-matched to transfusion ratio (CTR), transfusion probability (%T) and transfusion index (TI) were calculated as:
1. The formula for CTR:
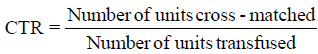
A ratio of > 2.5 indicates excessive cross-matching of blood for a specific procedure and a ratio of >2 is considered indicative of significant blood wastage.
2. Formula for transfusion probability (%)
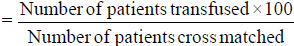
A value of < 30 was considered indicative of significant blood wastage.
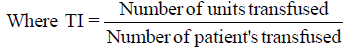
3. Transfusion Index
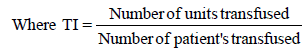
A value of < 0.5 signifies no need for cross-match
4. Blood Utilization (%)
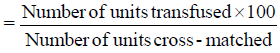
A value of < 50% indicates excessive cross-matching for the procedure.
5. MSBOS = 1.5 × TI
The MSBOS was formulated using Mead’s criterion which states that the number of red blood cells calculated was one and half times the TI for each surgical procedure. Thus, using the Mead’s criteria and clinical experience, the MSBOS was recommended for each surgical procedure.
Results
A total of 105 patients had 15 common orthopedic surgical procedures, for which requests for grouping and cross-matching were made. Sixty-eight (64.8%) were males while 37(35.2%) were females with ages ranging between 4-99 years. Eighty-four (80%) of the surgical procedures were done as elective while 21(20%) were emergencies.
A total of 224 units of blood were cross-matched for these patients but only 97 units (43.3%) were transfused. Table 1 shows the types of surgery with the number of cases, number of units cross-matched, number of patients cross-matched, number of units transfused, and number of patients transfused. Table 2 however, shows 6 indices that were calculated which are; CTR, Transfusion probability (%), Transfusion index, Blood utilization (%), MSBOS calculated using the Mead’s criteria and the Recommended MSBOS.
| Type of surgery | Number of patients | Unit cross matched | Patients Cross matched | Unit Transfused | Patient Transfused |
|---|---|---|---|---|---|
| Humeral Fracture (ORIF) | 7 | 13 | 7 | 5 | 4 |
| Forearm Fracture (ORIF) | 10 | 15 | 8 | 1 | 1 |
| Fracture of Femur (ORIF) | 30 | 62 | 30 | 29 | 19 |
| Spine | 2 | 4 | 2 | 0 | 0 |
| Pelvis + Acetabulum Reconstruction | 4 | 12 | 4 | 8 | 4 |
| Amputation (Upper Limb) | 4 | 12 | 4 | 4 | 2 |
| Amputation (Lower Limb) | 10 | 22 | 10 | 12 | 7 |
| Multiple Fractures | 7 | 21 | 7 | 18 | 7 |
| TKR | 3 | 6 | 3 | 0 | 0 |
| THR | 1 | 3 | 1 | 1 | 1 |
| Bone Tumors | 13 | 25 | 12 | 11 | 5 |
| Removal of Implants | 4 | 9 | 4 | 3 | 2 |
| Tibiofibular Fracture (ORIF) | 3 | 6 | 3 | 0 | 0 |
| Ankle fracture Reconstruction | 2 | 2 | 1 | 0 | 0 |
| Patella Fracture (ORIF) | 5 | 12 | 5 | 5 | 3 |
| Total | 105 | 224 | 101 | 97 | 55 |
Table 1. Number of patients, unit cross matched, patient’s cross matched, unit transfused, and patient transfused for the various orthopedic surgeries.
| Type of surgery | CTR | T (%) | TI | Blood Utilization (%) | MSBOS (M) | Recommended MSBOS |
|---|---|---|---|---|---|---|
| Humeral Fracture (ORIF) | 2.6 | 57.1 | 0.71 | 38.4 | 1.1 | 1 |
| Forearm Fracture (ORIF) | 15 | 12.5 | 0.12 | 6.7 | 0.9 | T & S |
| Fracture of Femur (ORIF) | 2.1 | 63.3 | 0.97 | 46.8 | 1.5 | 2 |
| Spine | 0 | 0 | 0 | 0 | 0 | T & S |
| Pelvis + Acetabulum Reconstruction | 1.5 | 100 | 2 | 66.7 | 3 | 3 |
| Amputation (upper limb) | 3 | 50 | 1 | 33.3 | 1.5 | 2 |
| Amputation (lower limb) | 1.8 | 70 | 1.2 | 54.5 | 1.8 | 2 |
| Multiple Fractures | 1.2 | 100 | 2.6 | 85.7 | 3.9 | 4 |
| TKR | 0 | 0 | 0 | 0 | 0 | T & S |
| THR | 3 | 100 | 1 | 33.3 | 1.5 | 2 |
| Bone Tumors | 2.3 | 41.7 | 0.92 | 44 | 1.4 | 1 |
| Removal of Implant | 3 | 50 | 0.75 | 33.3 | 1.1 | 1 |
| Tibiofibular Fracture (ORIF) | 0 | 0 | 0 | 0 | 0 | T & S |
| Ankle Reconstruction | 0 | 0 | 0 | 0 | 0 | T & S |
| Patella Fracture (ORIF) | 2.4 | 60 | 1 | 41.7 | 1.5 | 2 |
| Total | 2.3 | 54 | 0.9 | 43 |
Table 2. Crossmatch to transfusion ratio, transfusion probability, transfusion index, blood utilization, calculated MSBOS by Mead´s criteria and recommended MSBOS for orthopedic surgeries.
The CTR was >2 in 8 of the surgical procedures viz humeral fractures, forearm fractures, fractures of the Femur, upper limb amputations, total hip replacements (THR), bone tumors, removal of implants and patella fractures. The Transfusion probability (%) was < 30 in 5 of the surgical procedures namely; forearm fractures, spine surgery, total knee replacements (TKR), tibiofibular fractures and ankle fractures. The Transfusion index (TI) was < 0.5 in 5 of the surgical procedures which were; forearm fractures, spine surgery, TKR, tibiofibular fracture and ankle fracture. While percentage blood utilization was > 50% in only 3 surgical procedures viz; amputation of lower limbs, pelvis and acetabulum fracture and multiple fractures. Mead’s criteria and the Recommended (MSBOS) was calculated for all the fifteen surgical procedures using the Mead’s criteria and the MSBOS for our hospital was recommended, keeping in view clinical experience of the orthopedic surgeon and the patient’s variables. The type and screen (T&S) policy i.e., blood group and screening were recommended for forearm fracture, spine surgery, TKR, tibiofibular fracture and ankle fracture.
Discussion
One of the ways of evaluating blood transfusion practice is to determine the CTR and the closer the CTR approaches 1:1 the more likely the prediction that patients will need blood transfusion. In this study, the overall CTR was 2.3:1, which was similar to 2.4:1 reported by Olawumi and Bolaji [9] but was more than that of Kumari et al. [10] and Thimmaiah et al. [11] with CTR 2:1 each. Our overall CTR is indicative of significant blood wastage and therefore, the need for efforts to reduce the CTR to 1:1 [11].
Open reduction and internal fixation (ORIF) for fracture of the femur was the most common orthopedic surgery performed in our study, which was similar to that of the study conducted by Kumari et al. [10] and Thabah et al. [12]. The CTR for femoral fracture in this present study was 2.1 with Transfusion Probability T (%) of 63% and blood utilization of 46.8%. This was in keeping with that of Kumari et al. [10] with a CTR of 2.1, Tp of 53% and percentage blood utilization of 46.7% as against the CTR of 3.5 by Thabah et al. [12]. Of all the surgical procedures, forearm fractures had the highest CTR value of 15, a Tp of 12.5% and insignificant blood utilization of 6.7%. These results were similar to those of Kumari et al. [10] with a CTR of 5, T (%) of 25% and insignificant blood utilization of 20%. Subramanian et al. [4] also reported insignificant blood utilization in fracture of the forearm surgeries. In view of this, our MSBOS recommendation for fracture of the forearm was type and screen policy.
In this study, THR had a CTR of 3, a Tp of 100% and a recommended MSBOS of 2 units of blood which was the same as recommended by Challand et al. [13] and Kumari et al. [10] All the TKR cases done however were primary and unilateral, and the probability for blood transfusion was zero percent. This is similar to that of Thimmaiah et al. [11] with 5% and Kumari et al. [10] with 20% and thus informed our recommendation of type and screen policy for unilateral TKR in our Centre.
The patient’s pre-operative condition affects the CTR because the MSBOS algorithm uses the surgical procedure alone [14]. Blood wastage also depends on the surgeon’s expertise for a particular surgery as well as the anaesthetists preset higher transfusion triggers. Despite much studies and evidence based guidelines for transfusion, inappropriate transfusion still occurs [15].
In establishment of a schedule of MSBOS, emphasis should be laid on local circumstances, clinical practice and patient’s variables. The schedule should to be reviewed regularly and adjustments made as necessary for the recommended MSBOS schedule to be effective [6,16].
Conclusion
The overall CTR in this study was high with a low percentage blood utilization and resultant significant blood wastage. Implementation of the recommended MSBOS schedule in this will prevent unnecessary blood wastage, help standardize the blood ordering schedule, reduce workload on blood-bank personnel as well as reduce cost of treatment to the patient in our resource constrained environment.
REFERENCES
- Healthcare Cost and Utilization Project. HCUP facts and Figures 2009. Section 3: Inpatient hospital stays by procedure. Available from: http://www.hcup us.ahrq.gov/reports/facts and figures/2009/section3_TOC.jsp. [Last accessed on 2013 Oct 30].
- Chiavetta J.A., Herst R., Freedman J., et al.: A survey of red cell use in 45 hospitals in central Ontario, Canada. Transfusion. 1996;36:699-706.
- Mahadevan D., Challand C., Clarke A., et al.: Maximum surgical blood ordering schedules for revision lower limb arthroplasty. Arch Orthop Trauma Surg. 2011;131:663-667.
- Subramanian A., Rangarajan K., Kumar S., et al.: Reviewing the blood ordering schedule for elective orthopedic surgeries at a level one trauma care center. J Emerg Trauma Shock. 2010;3:225-230.
- Vibhute M., Kamath S.K., Shetty A.: Blood utilization in elective general surgery cases: Requirements, ordering and transfusion practices. J Postgrad Med. 2000;46:13-17.
- Efraim K.: Blood conservation in South Africa. A vital need. Bloodless Medicine and Surgery. 2001;43:7.
- Chawla T., Kakepoto G.N., Khan M.A.: An audit of blood cross-match ordering practices at the Aga Khan University Hospital: First step towards a maximum surgical blood ordering schedule. J Pak Med Assoc. 2001;51:251-254.
- Hardy N.M., Bolen F.H., Shatney C.H.: Maximum surgical blood order schedule reduces hospital costs. Am Surg. 1987;53:223-225.
- Olawunmi H.O., Bolaji B.O.: Blood utilization in elective surgical procedures in Ilorin. Trop Jr Health Sci. 2006;13:15-17.
- Kumari S., Kansay R.K., Kumar S.: Proposed maximum surgical blood ordering schedule for common orthopedic surgeries in a Tertiary Health - Care Center in Northern India. J Orthop Allied Sci. 2017;5:21-26.
- Thimmaiah R., Peter V.: Blood transfusion in hip and knee joint replacement surgery. Int J Orthop Surg. 2009;17:1.
- Thabah R., Sailo L.T., Bardoloi J., et al.: Maximum surgical blood order schedule’ in a newly set-up tertiary care hospital. Anaesth Pain Intensive Care. 2013;17:28-32.
- Challand C.P., Mahadevan D., Clarke A., et al.: Maximum surgical blood ordering schedule for revision hip and knee arthroplasty. J Bone Joint Surg Br. 2011;93:527-532.
- Palmer T., Wahr J.A., O’Reilly M., et al.: Reducing unnecessary cross-matching: A patient-specific blood ordering system is more accurate in predicting who will receive a blood transfusion than the maximum blood ordering system. Anesth Analg. 2003;96:369-375.
- Hasley P.B., Lave J.R., Kapoor W.N.: The necessary and the unnecessary transfusion: A critical review of reported appropriateness rates and criteria for red cell transfusions. Transfusion. 1994;34:110-115.
- Friedman B.A., Oberman H.A., Chadwick A.R., et al.: The maximum surgical blood order schedule and surgical blood use in the United States. Transfusion. 1976;16:380-387.



 Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.
Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.