Medial Malleolus fracture fixation by Screw fixation and Tension band wiring methods
Received: 22-Sep-2022, Manuscript No. JOTSRR-22- 75664; Editor assigned: 23-Sep-2022, Pre QC No. JOTSRR-22- 75664;(PQ); Accepted Date: Oct 10, 2022 ; Reviewed: 04-Oct-2022 QC No. JOTSRR-22- 75664;(Q); Revised: 05-Oct-2022, Manuscript No. JOTSRR-22- 75664;(R); Published: 12-Oct-2022, DOI: DOI.10.37532/1897- 2276.2022.17(9).77
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Objectives: To compare the outcome of Internal fixations of Medial malleolus fracture by Simple screw fixation and Tension band wiring methods.
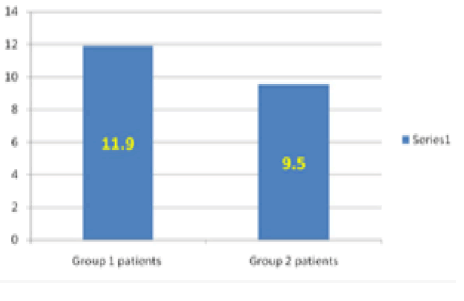
Patients and methods: This study was undertaken in 22 patients in two groups of 11 each, between 15 years-60 years. The first group patients were treated by Malleolar screw fixation while second one by Tension band wiring after matching for age, gender, fracture type, as well as the reasons of their fractured Medial Malleolus. Mean time for follow up was 15 months (9 months-21 months) Results: Radiological bone union took an average of 11.9 weeks in the first group, while 9.5 weeks in the second group (P=0.03)
The scores of the parameters like Pain, Stiffness, Swelling, Stair Climbing, Running, Jumping, Squatting, Support and Work or ADL were analyzed. Pain, Stiffness, Swelling, Stair Climbing was found significantly better in group 1 than group 2. While the scores of the parameters like Running, Jumping and Squatting did not show statistical significance (P>0.005), but their mean score were higher in group 2 as compared to Group 1.
None of the patients showed any sign of fixation failure or Kirschner wires migration
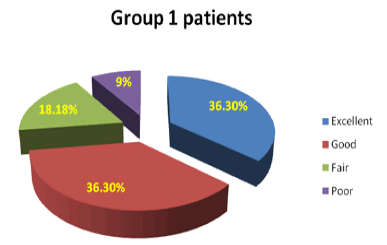
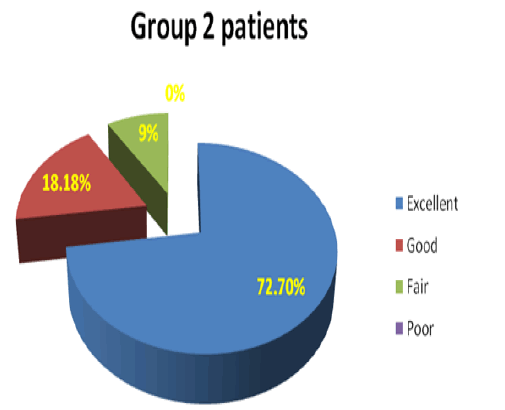
Excellent 4(36.3%), good 4 (36.3%), fair 2(18.1%) and poor 1(9%) scores were found in Malleolar screw fixation group patients while excellent 8 (72.7%), good 2 (18.18%), fair 1(9%) and poor 0 (0%) scores were found in Tension band wiring group according to modified ankle scoring system of Olerud and Molander. By applying test of significance, p was found to be not significant, P=0.388 by using Fisher’s Exact test in “R-Studio software”.
Conclusions: This comparative study showed that internal fixation of Medial Malleolar fractures result was better by tension wiring methods than screw fixation method if bone reunion is considered but by Modified ankle scoring system of Olerud and Molander no significant difference was observed by applying Fisher’s Exact test in “R-Studio software” p=0.388. But after comparing the scores of the parameters like Pain, Stiffness, Swelling, Stair Climbing, running, jumping, squatting, support and work or ADL, Pain, Stiffness, Swelling, Stair Climbing significantly better in group 1 than group 2. While the scores of the parameters like Running, Jumping and squatting did not show statistical significance (P>0.005), but their mean scores were higher in group 2 as compared to Group 1.
In Clinical and functional evaluation by Modified ankle scoring system of Olerud and Molander if we combine excellent (>90) good (81-90) scores, in Group 1, 90.88% showed execellent good score, while group 2 showed lesser percentage (72.6%) in this category. Fair (71-80) poor (<70) was found in 9% individuals in group 1 while 27.18% in group 2, according to modified ankle scoring system of Olerud and Molander. Recommendations: Further study is needed on a large number of cases for a longer duration of follow-up by allocation of the subjects through Randomized control trial, to arrive to the above conclusion.
Keywords
Fracture Ankle, Screw, Tension band.
Introduction
In orthopaedic and trauma surgery, Medial Malleolus fractures are one of the most common fractures. Screws, tension band wiring with suture materials, absorbable implants, and plate fixation are few accepted methods [1-5].
Ankle fractures are among the most common injuries of musculoskeletal system. It works like a close-fitting hinge with a mortise and tenon (distal ends of the tibia and fibula forming the box or mortise and upwards projecting talus as tenon). Between the dome of the talus and the tibial plafond, this joint works. These form congruent saddle-shaped weight-bearing surfaces. At the distal aspect of the tibia lateral facet of talus articulates with lateral malleolus and medial facet articulates with medial malleolus.
Fracture occurs due to combination of indirect rotational twist of the ankle (low-energy), and a tilt of talus and/or forceful rotation in the mortise of one or both malleoli, may or may not be associated with ligament injuries. Or it may be a more complicated, intense high energy fracture [6]. Cast immobilization is commonly done in nondisplaced fractures of the medial malleolus, but if there is more functional demand, internal fixation is the right choice to fasten healing and rehabilitation [6, 7].Ankle injuries can be simple closed fractures or may be complex open injuries. And hence surgery varies from non-operative casting to surgery, with the main aim of damage control procedures and finally definitive fixation.
Material and Methods
A Cross-sectional study was done on 22 patients with displaced closed medial malleolus fractures, from March 2020 to March 2022 in a tertiary care teaching hospital in the OPD as well as emergency of Orthopaedics department. Sample size was calculated as 4 pg/L2=11 (Keeping prevalence between 10%, allowable error 6%) [8-13]. Fixation in all the patients was done by internal fixation either by malleolar screw or with tension-band wiring were grouped accordingly in Group1 or Group 2 respectively after matching for age, gender, fracture type and causes of the fracture (twisting injury, fall, or motor vehicle accident) to remove selection bias (Table 1) [14].
Table.1 The classification of fracture that is used here is Danis-Weber classification of fractures.
| Type | Fracture | Tibiofibular ligaments |
|---|---|---|
| A | Distal to ankle joint | Intact, often avulsion. |
| B | At the level of the Tibiofibular ligaments | Intact in about 50% cases |
| C | Above the ankle joint | Torn |
INCLUSION CRITERIA
Weber type B&C Patient
Age 15 years-60 years.
Treatment: Surgery.
Six months follow up period.
EXCLUSION CRITERIA
Age <15 years and >60 years.
Weber type A patient
Pathological fractures
Open fractures
Follow up incomplete.
Inadequate data of the case
PRE-OPERATIVE EVALUATION
General health assessment Neurovascular status of the lower extremity. AP view mortise, and lateral views of the ankle: radiographic evaluation.
Evaluation of parameters like Pain, Stiffness, Swelling, Stair Climbing, running, jumping, squatting, support and work or ADL.
Surgical Technique
In supine posture, all the patients were given general anesthesia for operation. Pneumatic tourniquet was applied in the mid-thigh. An anteromedial incision was taken from 2 cm proximal to the fracture line to slightly posterior, 2 cm distal to the tip of the medial malleolus. Here the anteromedial aspect of articular surfaces is more visible to the surgeon and tibialis posterior tendon and its sheath are less likely to be damaged. Hence alignment of the fracture is more accurate. Reflect the flap with the skin and underlying subcutaneous tissue intact. Careful handling will prevent skin sloughing as the blood supply of this area is poor. Great Saphenous vein and its concomitant nerve are also protected. Between the fracture surfaces, a small fold of periosteum is commonly interposed. This was removed with periosteal elevator or a curet and small serrations of the fracture was exposed. Debridement was done for loose osseous or chondral fragments while preservation was done for large osteochondral fragments. Displaced malleolus was brought in normal position by small bone-holding clamp. Then it was fi xed internally there and then with malleolar screw or tension-bandwiring.
Case Presentation
GROUP 1 PATIENTS
In a superior posterior direction, a 3.2 mm hole was drilled. Then distal fragment was reduced with either a pointed clamp or two Kirschner wires bent to stay out of way as temporary fixation devices. Then whole length was measured along with insertion of malleolar screw without tapping till it approaches the other cortex. Then after ti ghtening th e screw kirschner wires were removed.
GROUP2 PATIENTS
Perpendicular to the fracture line, with two 2 mm smooth kirschner wires which were parallel were internally fixed. Then for prevention of slipping of the figure-of-eight over the exposed ends of the Kirschner wires, their ends should be bent at 90° angles and then the wire were tightened.
The super medial corner of the joint was inspected carefully to make sure that either the screw or Kirschner wires had not crossed the articular surfaces. To verify it and to avoid any faulty insertion, X-ray was done if image intensifier was available. In 3 cases, screen control was used in our study. The tourniquet was deflated at the end of operation; haemostasis was taken, and closed the wound with interrupted suture. To prevent necrosis of the skin edges, tight stitches were avoided. Then posterior plaster splint with thick padding was applied with in a neutral position of the ankle. After treatment: Immobilization of the ankle in elevated and neutral position was done in a posterior plaster splint. Anterior, lateral, and mortise views of X-ray was taken postoperatively.
Follow-Up
Follow-up was done at 2 weeks, 6 weeks, 3 months, and 6 months. After operation, at 6 weeks, and during subsequent visits, assessment of radiological healing as well as physical examination was done. Stitches were removed after 10 days -14 days, wound examined and complication if any was treated accordingly. Posterior plaster splint was changed as well as instructed to remove it daily. Also it was advised to start range-ofmotion exercises. Restriction of weight bearing was advised for 6 weeks then step by step splint was discarded and partial weight bearing was started by till 12 weeks after that time full weight bearing was allowed.
Evaluation
Patients who had undergone surgical treatment for ankle fractures from April 2019 to April 2022 in a tertiary care hospital in Pune. A total of 22 volunteer patients were evaluated.
All the patients were evaluated radiologically, clinically and functionally by a modification of the scoring system of Olerud and Molander It consists of 9 questions: pain (0 to 25), stiffness (0 to 10), swelling (0 to10), stair climbing (0 to 10), running (0 to 5), jumping (0 to 5), squatting (0 to 5), use of supports (0 to 10), and work/activity level (0 to 20), with higher scores indicating better outcomes [9].
A set of questionnaire was use to assess each component of this scale, along with objective clinical criteria: maximum of 100 points (>91 excellent results, 81-90 good results, 71-80 fair results, <70 poor results) [3] (Table 2).
Table: 2 Modification of the scoring system of Olerud and Moland.
| Parameters” | Degree | Score |
|---|---|---|
| “Pain” | “None”” | 25 |
| “While walking on uneven surface”” | 20 | |
| “While walking on even surface  outdoor”” | 10 | |
| “While walking indoor constant and severe”” | 5 | |
| “Stiffness” | “None”” | 10 |
| “Stiff”” | 0 | |
| “Swelling” | “None”” | 10 |
| “Only in the evening”” | 5 | |
| “Constant”” | 0 | |
| “Stair climbing” | “No problem” | 10 |
| “Impaired”” | 5 | |
| “Impossible”” | 0 | |
| “Running | “Possible” Â “” | 5 |
| “Impossible” | 0 | |
| “Jumping” | “Possible” | 5 |
| “Impaired” | 0 | |
| “Squatting” | “Possible” | 5 |
| “Impossible”” | 0 | |
| “Support” | “None”” | 10 |
| “Tapping or wrapping”” | 5 | |
| “Stick or crutch”” | 0 | |
| “Work or ADL” | “Same as before injury”” | 20 |
| “Reduced” ” | 15 | |
| “Change to simpler/ part time job”” | 15 | |
| “Severely impaired work capacity”” | 0 |
FLOW DIAGRAM
Medial Malleolar fractures patients included.
Inclusion criteria: Weber type B&C Patient, age 15 years–60 years, treatment: surgery, 6 months follow up period; Exclusion criteria Weber type A patient, age <15 and >60 years, pathological fractures, open fractures, follow up incomplete, inadequate data of the case.
Calculation of sample size
1Ζ−α /22 (p1− )p/D2 =1 (Keeping prevalence between 10%, allowable error 6%) 1Ζ−α / 22 =1.96 (at 5% type 1) P=Expected proportion in population based on previous studies 10%.
Result
Radiological finding: Group1 patients bone union took average 11.9 weeks (8 weeks-18 weeks) and in Group 2 patients 9.5 weeks (6 weeks-12 weeks) (P=0.03).
None of the patients showed any sign of fixation failure or Kirschner wires migration.
Group 2 showed better Clinical and functional evaluation by Modified ankle scoring system of Olerud and Molander with regard to Pain, Stiffness, Swelling and Stair Climbing while Running, Jumping and squatting was not statistically significant though their mean score of these also were higher in group 2 as compared to Group 1
Excellent 4(36.3%), good 4(36.3%), fair 2(18.1%) and poor 1(9%) scores were found in Malleolar screw fixation group patients while excellent 8(72.7%), good 2(18.18%), fair 1(9%) and poor 0 (0%) scores were found in Tension band wiring group according to modified ankle scoring system of Olerud and Molander. By applying test of significance, p was found to be not significant, P=0.388 by using Fisher’s Exact test in “R-Studio software”.
Level of significance was kept at CI of 95 %.( Table 3)
Table3: Demographic, clinical, social characteristics of study participants
| “Medial Malleolar fractures” | “Malleolar screw” | “Tension-band” |
|---|---|---|
| “Age” | 38 (24-65) | 39 (23-65) |
| “Male: female ratio” | 06:05 | 06:05 |
| “Right: left ratio” | 06:05 | 06:05 |
| “Weber B: Weber C” | 08:03 | 08:03 |
| “Causes of the fracture” | ||
| “Twist” | 6 | 6 |
| “Fall” | 2 | 1 |
| “Road traffic accident” | 3 | 4 |
No significant differences between the two groups were found in age with median 37 years rest all gender, fracture type (Weber type B and C), and aetiology (twisting, fall, or motor vehicle accident) were matched. For continuous variables t-test was used to analyse between the groups.
RADIOLOGICAL FINDING
• In the post-operative radiographs, anatomic reduction was confirmed in review of post-operative in all the twenty-two patients.
• Normal fracture healing was found in all the patients. No malunion, delayed union or non-union, or loss of reduction was found in any of the patients.
• Sign of fixation failure or Kirschner wires migration was not found in any of the patient in either of the group.
• Group1 patients bone union took average 11.9 weeks (8 weeks-18 weeks) and in group 2 patients 9.5 weeks (6 weeks-12 weeks) (P=0.03). This was the radiological finding (Fig 1).
The following table reveals mean comparison of Pain, Stiffness, Swelling, Stair Climbing, running, jumping, squatting, support and work or ADL Table 4-5.
Table 4: Statistical Analysis of parameters like Pain, Stiffness, Swelling, Stair Climbing, running, jumping, squatting, support and work or ADL
|
|
Treatment |
N | Mean | Std. Deviation | P Value | 95% Confidence Interval | |
|
Pain |
1 | 11 | 14.5455 | 7.56787 | 0.003 | -13.21692 | -3.14671 |
| 2 | 11 | 22.7273 | 2.61116 | ||||
|
Stiffness |
1 | 11 | 6.3636 | 5.04525 | 0.041 | -6.80953 | -0.4632 |
| 2 | 11 | 10 | 2.23607 | ||||
|
Swelling |
1 | 11 | 5 | 3.16228 | 0.006 | -7.10722 | -0.16551 |
| 2 | 11 | 8.6364 | 2.3355 | ||||
|
Stair climbing |
1 | 11 | 6.3636 | 2.3355 | 0.001 | -4.93015 | -1.43349 |
| 2 | 11 | 9.5455 | 1.50756 | ||||
|
Running |
1 | 11 | 4.0909 | 2.0226 | 1 | -1.79902 | 1.79902 |
| 2 | 11 | 4.0909 | 2.0226 | ||||
|
Jumping |
1 | 11 | 2.7273 | 2.61116 | 0.186 | -3.44096 | 0.71369 |
| 2 | 11 | 4.0909 | 2.0226 | ||||
|
Squatting |
1 | 11 | 2.2727 | 2.61116 | 0.083 | -3.89551 | 0.25914 |
| 2 | 11 | 4.0909 | 2.0226 | ||||
|
Support |
1 | 11 | 6.8182 | 2.52262 | 0.005 | -5.30198 |
-1.06166 |
| 2 | 11 | 10 | 2.23607 | ||||
|
Work or ADL |
1 | 11 | 16.8182 | 2.52262 | 0.03 | -4.30632 | -0.23914 |
| 2 | 11 | 19.0909 | 2.0226 | ||||
Table 5: Clinical and functional evaluation by Modified ankle scoring system of Olerud and Molander
| Group 1 patients | Group 2 patients | |
|---|---|---|
| Excellent (>91) | 4 (36.3%) | 8 (72.7%) |
| Good (81-90) | 4 (36.3 (%) | 2 (18.18%) |
| Fair (71-80) | 2 (18.18%) | 1(9%) |
| Poor (<70) | 1 (9%) | 0 (0%) |
The scores of the parameters Pain, Stiffness, Swel li ng, Stair Climbi ng was significantly better in group 1 than group 2. While the scores of the parameters like Running, Jumping and squatting did not show statistical significance (P>0.005), their mean score of these also were higher in group 2 as compared to Group 1.
Normality has been checked using the Kolmogorov Smirnov test (P<0.05). Independent t-test used to compare the mean score of various parameters at 95% level of confidence. Microsoft excels and Open EPI used for analysis.
Out of all only Running, Jumping and squatting was not statistically significant (P>0.005), whereas the mean score of Pain, Stiffness, S welling, Stair Climbing were higher in group 2 as compared to Group 1.
In Group1, 4 (36.3%) patient and in Group 2, 8 (72.72%) patients showed excellent score. Sign of fixation was found well in 4 (36.3%) patients in Group1 and 2 patients (18.18%) in Group 2. It was found fair in 2 (18.18%) patients in Group1 and 1 patient (9%) in Group 2 and poor in 1 (9 %) patients in Group1 and none of the patients in Group2 patients according to modified ankle scoring system of Olerud and Molander9 By applying test of significance, p was found to be p=0.388 by using Fisher’s Exact test in “R-Studio software” (Fig 2, 3).
Discussion
Subject material as well as assessment of the results was not uniform, so comparison of the reports is difficult with other studies.In our study, in Group1, i.e. Malleolar Screw group, and Group 2 i.e. Tension Band group, the Modified Ankle Score of Olerud and Molander, was found to be good and excellent in 72.6% and 90.9% of the cases respectively. This is similar to the finding of other studies. In Olerud Morland study it was 78% and 90% respectively while in Ayyoub A [15]. It was 89% and 90% respectively. And in case of Sang-Hanko M, Young-Jun Park D [16]. study, it was 78% and 89% respectively. But in our study applying test of significance, p was found to be p=0.388 by using Fisher’s Exact test in “R-Studio software”, that means both the groups are not significantly different at 95% CI, if we compared the two groups in excellent, good, fair and poor group.
The time taken for radiologic bone re-union in our study is 11.9 weeksand 9.5 weeks in Group 1 and Group 2 respectively, and P value was found to be p=0.03, that means group 2 having Tension-band wiring showed significantly faster bone re-union than Malleolar Screw group. This is in agreement with SK [17]. Where the meantime for malleolar screws and tension-band wiring was 12 and 9 weeks respectively [17].
In our study, no case of delayed union occurred, which is similar to the results of Kim SK [18].100% union rate in both groups without any case of delayed union). This may be due to stable anatomical structure and less soft tissue stripping. There was a loss of reduction with the use of tension-band technique because K wires become loose end and migrates proximally [19].
Though some authors believe wire migration was not a problem if there is a proper surgical technique [20]. The similar is observed in our study. Many authors have described Tension-band fixation method for medial malleolar fractures [21, 22]. observed biomechanics advantages of this technique. The faster union rate in group 2 (mean of 9.5 weeks) in comparison to Group 1 patients (mean of 11.9 weeks) is explained by this in our study [23].
Conclusion
For small fragment fixation of medial malleolar fractures, Tensionband wiring was found technically better. Tension-band wiring is costeffective as well as easily available, another positive point, especially for our country where the number of ankle fractures is too many. Tension-band wiring shows a faster radiological union and better Clinical and functional outcomes in comparison to malleolar screws.
References
- Frydrysek, K.; Sir, M.; Pleva, L. Strength Analyses of Screws for Femoral Neck Fractures. J. Med. Biol. Eng. 2018, 38, 816-834. [Google Scholar]
[CrossRef]
- Clyde J, Kosmopoulos V, Carpenter B. A biomechanical investigation of a knot-less tension band in medial malleolar fracture models in composite sawbones.J Foot Ankle Surg 2013;52:192-4. [Google Scholar][CrossRef]
- Georgiadis GM, White DB. Modified tension band wiring of medial malleolarankle fractures. Foot Ankle Int 1995;16:64-8. [Google Scholar][CrossRef]
- Fowler TT, Pugh KJ, Litsky AS, et al. Medial malleolar frac-tures: a biomechanical study of fixation techniques. Orthopedics 2011;34:349-55. [Google Scholar] [CrossRef]
- Varenne Y, Curado J, Asloum Y, et al. Analysis of risk factors of the postoperative complications of surgical treatment of anklefractures in the elderly: a series of 477 patients. Orthop Traumatol Surg Res2016;102:245-8. [Google Scholar] [CrossRef]
- Nieto H, Baroan C. Limits of internal fixation in long-bone fracture. OrthopTraumatol Surg Res 2017;103:61-6. [Google Scholar]
[CrossRef]
- Solomon L, Warwich D, Nayagam S. Apley system of orthopedics and fractures London: Arnold; 2010. pp. 733-744. [Google Scholar]
[CrossRef]
- Michelson JD. Fractures about the ankle. J Bone Joint Surg Am. 2006;77(1):142-149. [Google Scholar]
- Michelson J, Solocoff D, Waldman B, et al. Ankle fractures. The Lauge-Hansen classification revisited. Clin Orthop Relat Res 1997;345:198-205. [Google Scholar]
[CrossRef]
- Vander Griend R, Michelson JD, Bone LB. Instructional course lecture: fractures of the ankle and the distal part of the tibia. J Bone Joint Surg Am 1996;78:1772-83. [Google Scholar][CrossRef]
- Jones CB, Slabaugh PB. Prospective randomized evaluation of medial malleolar fixation for ankle fractures: single versus double screw fixation. Orthop Trans 1997;98; 21:1194. [Google Scholar]
- Michelson J. Fractures about the ankle. J Bone Joint Surg Am 1995;77:142-52. [Google Scholar]
[CrossRef]
- Ronald M. Dumigan, MD, Dwight G. et al. Analysis of Fixation Methods for Vertical Shear Fractures of the Medial Malleolus. J Orthop Trauma 2006;20:687-91[Google Scholar]
[CrossRef]
- Meagan M. Jennings, DPM, et al.Fixation of the Medial Malleolar Fracture: A Simplified Technique. The Journal of Foot & Ankle Surgery 2008;47(4):368-71. [Google Scholar]
- Kennedy JG, Johnson SM, Collins AL, et al. An evaluation of the Weber classification of ankle fractures. Injury. 1998 Oct 1;29(8):577-80[Google Scholar]
[CrossRef]
- Ayyoub A. Mohammed et al. A comparative study in fixation methods of medial malleolus fractures between tension bands wiring and screw fixation. SpringerPlus (2016)[Google Scholar]
- Sang-Hanko M, Young-JunPark D. Comparison between screw fixation and tension-band wiring for medial malleolus fractures. Korean Soc Foot Surg. 2002;6(1):41-44. [Google Scholar]
[CrossRef]
- Nurul Alam, Parviz S, et al. Comparative study of malleolar fractures by tension-band and malleolar screw. BOS J. 2007;12(1):13-19. [Google Scholar]
[CrossRef]
- Kim SK, et al. One or two lag screws for fixation of Danisâ??Weber type B fractures of the ankle. J Trauma. 2005;46(6):1039-1044.[Google Scholar]
- Mack D, Szabo RM. Complications of tension-band wiring. J Bone Joint Surg. 2005;67:1936-1941. [Google Scholar]
[CrossRef]
- Kinik H, Mergen E. Self-locking tension-band technique. Arch Orthop Trauma Surg. 1999;119:432-434. [Google Scholar]
- Muller ME, Allgower M, Schneider R, et al. Manual of internal fixation. New York: Springer; 2000. pp. 42-48. [Google Scholar]
[CrossRef]
- Ostrum RF, Listsky AS. Tension-band fixation of medial malleolar fracture. J Orthop Trauma. 2008;6:464.. [Google Scholar]



 Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.
Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.