Morphological variation in proximal femur anatomy and its implication in metaphyseal fit femur prosthesis in total hip arthroplasty: A dry bone study
Received: 18-Jul-2022, Manuscript No. jotsrr-22-69534; Editor assigned: 20-Jul-2022, Pre QC No. jotsrr-22-69534(PQ); Accepted Date: Jul 28, 2022 ; Reviewed: 25-Jul-2022 QC No. jotsrr-22-69534(Q); Revised: 27-Jul-2022, Manuscript No. jotsrr-22-69534(R); Published: 02-Aug-2022, DOI: 10.37532/1897-2276.2022.17 (7).73
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Total hip replacement is the most common procedure done by orthopedic surgeons which restores the hip joint function. The most commonly used cementless femoral stems in primary hip arthroplasty are metaphyseal fit stems (CORAIL). We found that in certain patients the metaphyseal stem tips comes in contact with the medial cortex and valgus orientation. In this context, there might be variation in metaphyseal fit in type 2 stems, which might lead to stress shielding and thigh pain. So, we decided to do a simple measurement in dry bones and to look for this variation in the proximal femur anatomy which will help to predict preoperatively the implications of metaphyseal fit stems.
Methodology
This is a dry bone study done in the department of orthopedics, MGMCRI. In 65 femurs following measurements were done directly and digitally in PACS after obtaining a templating radiograph.
The proximal femur mediolateral shaft diameter was measured at the lower border of the lesser trochanter. Medial cortex to greater trochanter -Distance between lines drawn along the lateral most border of the greater trochanter to a vertical line drawn along the medial cortex of the femur. Lateral cortex to greater trochanter- Distance between a lines drawn along the lateral most border of greater to a vertical line drawn along the lateral cortex of the femur. The total length of the femur using the infant meter. The statistical analysis was done.
Result
Among the 65 femurs, the distance between the tips of the stem to the innermost aspect of the medial cortex was less than 50% of the canal diameter in 24 femurs; among them the distance was closest almost touching the medial cortex in nine femurs. In these femurs, the distance between the lateral cortex line to an outermost aspect of the greater trochanter was high which was significant (p value=0.045). Three of them were Dorr type I femur and six were Dorr type II.
Conclusion
Our study demonstrates a simple radiological preoperative measurement which will help in choosing an alternative to the metaphyseal fitting stems (CORAIL) in certain population with this varied anatomy. This varied anatomy we describe as proximal femur metaphyseal valgus.
Keywords
femur fractures, arthroplasty, hip replacement
Introduction
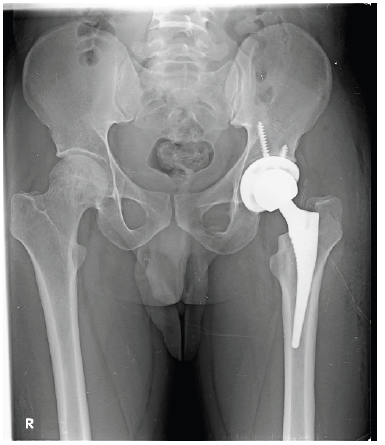
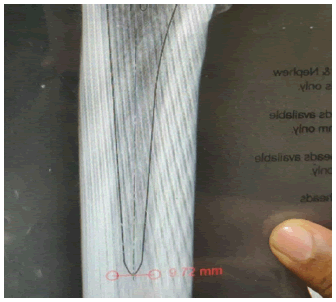
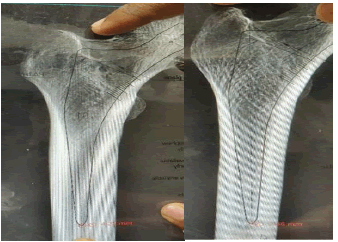
Total hip arthroplasty is one of the most successful procedures which give a reliable outcome at the end stage disease of hip [1]. The long term survival of the prosthesis depends on proper alignment of the femoral stem and acetabular cup. It has been described and reported that varus stem alignment is associated with instability due to the poor seating of the femoral component [2, 3]. It is recommended to ensure neutral stem position to get proper fit [4]. In this context we came across in certain patients there was valgus orientation of the stem, and the stem tip meets medial endosteal cortex of the femur (Fig 1).
There were no studies regarding this alignment, but it has been reported that if the proximal metaphyseal fit to be proper in both 6 mediolateral and anteroposterior planes the stem should be in neutral position and if the stem tip meets the endosteal cortex there might be thigh pain [5]. The type 2 stem is a double wedge tapered stem, in both anteroposterior and mediolateral plane. It was designed to fix via contacting the mediolateral metaphyseal cortex and anteroposterior metaphyseal cortex [6]. So, understanding the morphology in these types of femurs with valgus orientation of metaphysis and its implication on type 2 metaphyseal fit (CORAIL collarless) stems may aid the surgeons to choose an alternative stem to achieve neutral femoral component alignment. We hypothesised that proximal femur morphological variation affects the metaphyseal fit in CORAIL collarless stems in total hip arthroplasty. The objective of this study was to identify the proximal femur anatomical variation in dry bones and their radiographs using measurements with help of acetate templates.
Method
This dry bone study was approved by Institutional review board and was conducted in Department of Orthopaedics, Mahatma Gandhi Medical College and Research Institute. 70 dry femurs both left and right were obtained from our anatomy lab. Five femurs which had evidence of previous injury or deformed were excluded and the remaining 65 femurs was used, and the measurements were done. The bones were serially labelled. The direct measurement was done in the lab using infantometer, vernier calliper and metal scale. The femurs were kept in a flat board in anatomical position and following x measurements were obtained.
1. The length of the femur was obtained by using infantometer.
2. The shaft diameter was measured at the lower border of lesser trochanter using vernier calliper.
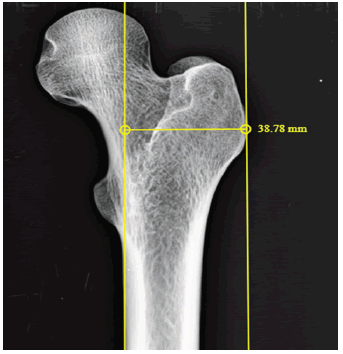
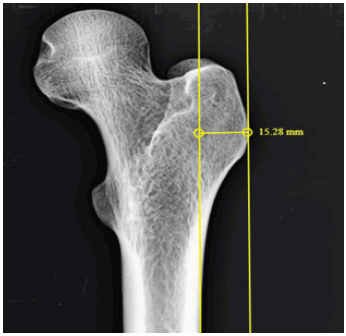
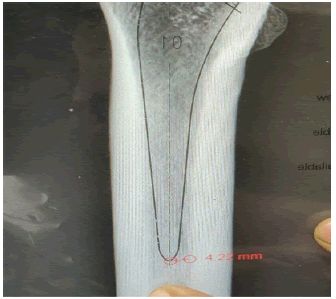
3. Lateral cortex to greater trochanter- Distance between a lines drawn along the lateral most border of greater trochanter to a vertical line drawn along the lateral cortex of the femur. The femurs were kept in anatomical position with a 30 mm spherical ball aside and a digital radiograph was obtained. The CMC templating hybrid technique as described by Krishnamoorthy et al was used to template the femurs using acetate template (Smith & Nephew) for CORAIL collarless stem [7]. The following measurements were done in PACS (Fig 2-7).
1. The shaft diameter was measured at the lower border of lesser trochanter
2. Medial cortex to greater trochanter (MC-GT) -Distance between a lines drawn along the lateral most border of greater trochanter to a vertical line drawn along the medial cortex of the femur.
3. Lateral cortex to greater trochanter (LC-GT) - Distance between a lines drawn along the lateral most border of greater to a vertical line drawn along the lateral cortex of the femur .
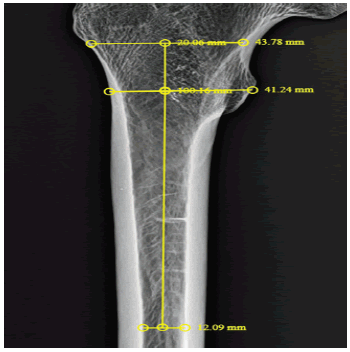
4. The canal flare index was measured, the ratio between the isthmus and the endosteal diameter 2cm above the lesser trochanter. [8].
5. The endosteal canal diameter at the distal tip of the prosthesis.
6. The stem tip to medial endosteal cortex- the distance between the stem tips to the medial endosteal cortex was measured.
The femurs were classified as per Dorr. The Type A indicates thick cortices both in AP and lateral radiographs (Champagne flute), type B indicates thinning of posterior cortices in lateral radiograph and the type C indicates thinning of cortices in both views (Stovepipe) [8].
The canal flare Index was calculated, this was the ratio between the intercortical width of the femur two cm above the lesser trochanter and at the canal isthmus [9]. Two independent observers trained in arthroplasty did the measurements.
Statistical Analysis
Data is analyzed using statistical software R version 4.2.1. and Microsoft Excel. Categorical variables are represented by frequency and %. Continuous variables given in Mean ± SD / Median (IQR) form. Normality of variable is checked by Shapiro Wilk test. Spearman’s rank correlation test is used to check the correlation of different variables with Stem tip- Medial Canal. Logistic regression is used to check the relation of different variables with Fit. P-value less than or equal to 0.05 indicates statistical significance.
Results
Among the 65 femurs, the mean and standard deviation of femur length, shaft diameter outer diameter, MC-GT distance, LC-GT distance, canal diameter, the stem tip medial canal distance and CFI are shown in (Table 1) (Fig 8).
Table.1 Summary of variables.
| Variables | Mean ± SD | Median (IQR) |
|---|---|---|
| Femur Length | 42.56 ± 2.77 | 41.8 (40.5, 44.5) |
| Shaft Diameter (Below LT) | 28.99 ± 2.08 | 28.73 (27.6, 30.44) |
| Medial cortex to greater trochanter (MC-GT) | 37.95 ± 3.38 | 37.41 (35.20, 40) |
| Lateral cortex to greater trochanter (LC-GT) | 11.59 ± 2.89 | 11.46 (9.85, 13.63) |
| Canal Diameter | 10.72 ± 2.63 | 10.4 (9.43, 11.84) |
| Stem tip- Medial Canal | 4.89 ± 1.78 | 4.73 (3.74,5.81) |
| CFI (Canal flare index) | 4.15 ± 0.98 | 4.12 (3.62, 4.59) |
The Pearson correlation of the stem tip- to medial endosteal canal with other variables like femur length, shaft diameter and MC-GT was not significant but there were negative 11 correlations with stem tip - medial canal distance with that of LC-GT. The stem tip- medial canal distance showed positive and statistically significant correlation p < 0.04 (Table.2)
Table 2. Pearson correlation of different variables with stem tip-medial canal
| Stem tip- Medial Canal | ||
|---|---|---|
| Femur Length | Pearson Correlation | 0.0845 |
| p-value | 0.5 | |
| N | 65 | |
| Shaft Diameter(Below LT) | Pearson Correlation | 0.2109 |
| p-value | 0.09 | |
| N | 65 | |
| Medial cortex to greater trochanter(MC-GT) | Pearson Correlation | 0.07 |
| p-value | 0.56 | |
| N | 65 | |
| Lateral cortex to greater trochanter (LC-GT) | Pearson Correlation | -0.0131 |
| p-value | 0.918 | |
| N | 65 | |
| Canal Diameter | Pearson Correlation | 0.322 |
| p-value | 0.05* | |
| N | 65 | |
| Canal flare index (CFI) | Pearson Correlation | 0.3486 |
| p-value | 0.004* | |
| N | 65 |
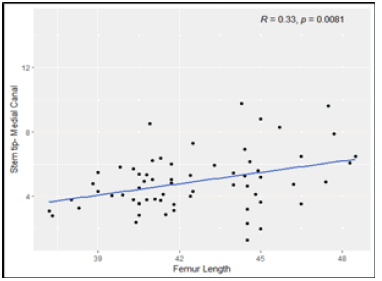
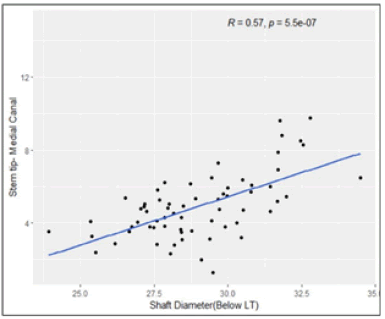
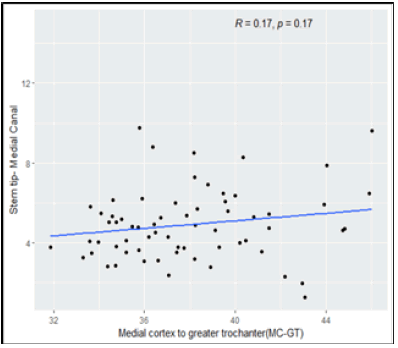
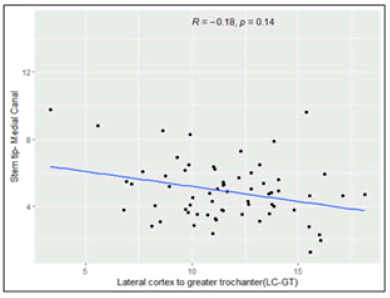
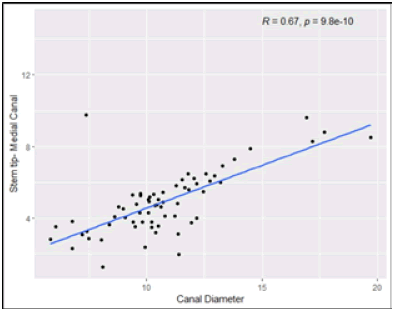
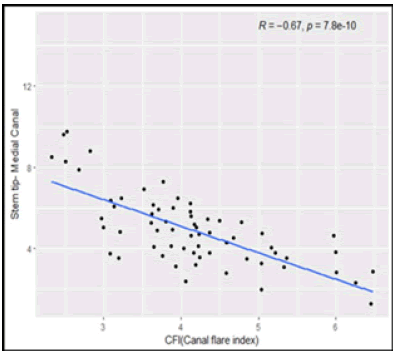
The Spearman’s rank correlation test, we observed that, Femur Length have low positive correlation with Stem tip- Medial Canal Figure 9 to 14. Shaft Diameter (Below LT) and Canal Diameter have moderate positive correlation with Stem tip- Medial Canal. CFI (Canal Flare Index) has moderate negative correlation with Stem tip- Medial Canal. Medial cortex to greater trochanter (MC-GT) and Lateral cortex to greater trochanter (LC-GT) are not significantly correlated with Stem tip- Medial Canal (Table 3).
Table 3. Spearman’s rank correlation of different variables with Stem tip- Medial Canal
| Variables | Correlation Coefficient | p-value |
|---|---|---|
| Femur Length | 0.3256 | 0.0081Sp* |
| Shaft Diameter (Below LT) | 0.5748 | < 0.001Sp* |
| Medial cortex to greater trochanter (MC-GT) | 0.1708 | 0.1719Sp |
| Lateral cortex to greater trochanter (LC-GT) | -0.1841 | 0.1421Sp |
| Canal Diameter | 0.6707 | < 0.001Sp* |
| CFI (Canal flare index) | -0.6736 | < 0.001Sp* |
| Abbreviation: Sp –Spearman’s rank correlation test, * indicates statistical significance. | ||
The other univariate analysis with each variable was weak and not significant. The distance between the tips of the stem to the innermost aspect of the medial cortex was less than 50% of the canal diameter in 24 femurs; among them the distance was closest almost touching the medial cortex in nine femurs. From logistic regression, it was observed that, there was significant effect of Shaft (Below LT), Medial cortex to greater trochanter (MC-GT) with fit. There was no significant effect of Femur Length, Lateral cortex to x Greater Trochanter (LC-GT), Canal Diameter and CFI (Canal Flare Index) with fit. With unit increase in shaft diameter, the odds of having good fit increases by 1.54 (Table 4).
Table 4. Result of logistic regression for fit.
| Odds Ratio (95% CI) | p-value | |
|---|---|---|
| Femur Length | 1.02 (0.98, 1.06) | 0.4115 |
| Shaft Diameter (Below LT) | 1.54 (1.08, 2.18) | 0.0191* |
| Medial cortex to greater trochanter (MC-GT) | 0.72 (0.56, 0.94) | 0.0175* |
| Lateral cortex to greater trochanter (LC-GT) | 0.98 (0.94, 1.04) | 0.5544 |
| Canal Diameter | 0.99 (0.94, 1.05) | 0.7771 |
| Ratio (ML-LT) | 1.5*10-7 (3.5*10-13, 0.07) | 0.0213* |
| CFI (Canal flare index) | 0.96 (0.84, 1.1) | 0.5767 |
| Abbreviation: * indicates statistical significance. | ||
The individual variables relationship with stem tip medialisation. The valgus orientation and stem tip medialisation were present in three Dorr types a femurs and six were Dorr type B
Discussion
The results of our study show that the morphological variation, that is the metaphyseal valgus and stem fit were correlated with femoral stem valgus. This is the first study describing the valgus orientation of the proximal femur. When the distance between the MC-GT increases with increase in canal diameter the stem orientation will be in center and will have good fit. As the canal flare index ratio increases there was stem tip medialization and this is more common in younger and middle-aged patients. In the study done by David S Casper et al they divided the CFI again into Medial Flare Index (MFI) and Lateral Flare Index (LFI) [10]. They showed the MFI changed with age in female and the LFI were high in younger age group compared with elderly. This is comparable to our results, but we don’t know the age of the dry bones. When the MC-GT distance increased in Dorr type A and B femurs there is a high chance for valgus orientation of the stem and medialization of stem tip. This type of valgus orientation of proximal femur is seen after valgus osteotomy of proximal femur and in certain dysplastic hips [11]. If there is increase in canal diameter with the increase in MC-GT distance there will be good fit of prosthesis and this is seen in Dorr type C femur. When the femur prosthesis is undersized there is chance for loss of osteointegration and early osteolysis and if it is oversized, there is high chance for periprosthetic fractures particularly in type 2 metaphyseal fit stems. The broaching technique might change the orientation of the stem but it mostly ends in a diaphyseal fit stem than a metaphyseal fit stem and excessive bone is also removed. Precise placement of the femoral prosthesis is important to get good functional outcome and longterm term survival of component. There are limitations in our study, first we studied the x ray images of dry bone rather the real patients with the aim to find out the morphological variation in real bone, as its dry bone the morphology could have altered, we don’t know the age and gender of the bone, we did our measurements using radiographs, computed tomography could have given more appropriate measurements and the sample size was small. There could have been variations in manual templating.
Conclusion
Our study demonstrates a simple radiological preoperative measurement which will help in choosing an alternative to the CORAIL collarless stems in certain population with this varied anatomy. If the canal flare index ratio increased and the distance between the line along the medial cortex of femur and the outermost aspect of greater trochanter increased with decrease in canal diameter in Dorr type A and B femurs it’s better to choose an alternative to CORAIL collarless stems. This varied anatomy we describe as proximal femur metaphyseal valgus. Future biomechanical and finite element analysis after implantation of prosthesis in these types of femurs will support and validate our results.
References
- McLaughlin JR, Lee KR. Total hip arthroplasty with an uncemented femoral component. Excellent results at ten-year follow-up. J Bone Joint Surg Br. 1997 Nov;79(6):900-7.[CrossRef][Google Scholar]
- Wang H, Gu J, Liu X et al. Variation in greater trochanteric lateroversion: a risk factor for femoral stem varus in total hip arthroplasty. HIP International. 2020 Jan 1;30(1):33–9. [CrossRef][Google Scholar]
- de Beer J, McKenzie S, Hubmann M, et al. Influence of cementless femoral stems inserted in varus on functional outcome in primary total hip arthroplasty. Can J Surg. 2006 Dec;49(6):407–11. [CrossRef][Google Scholar]
- Min BW, Song KS, Bae KC, et al. The Effect of Stem Alignment on Results of Total Hip Arthroplasty with a Cementless Tapered-Wedge Femoral Component. The Journal of Arthroplasty. 2008 Apr 1;23(3):418-23. [CrossRef][Google Scholar]
- Campbell A, Rorabeck C, Bourne R, et al. Thigh pain after cementless hip arthroplasty. Annoyance or ill omen. The Journal of Bone and Joint Surgery British volume. 1992 Jan;74-B(1):63-6. [CrossRef][Google Scholar]
- Khanuja HS, Vakil JJ, Goddard MS, et al. Cementless femoral fixation in total hip arthroplasty. J Bone Joint Surg Am. 2011 Mar 2;93(5):500-9. [CrossRef][Google Scholar]
- Krishnamoorthy VP, Perumal R, Daniel AJ, et al. Accuracy of templating the acetabular cup size in Total Hip Replacement using conventional acetate templates on digital radiographs. J Clin Orthop Trauma. 2015 Dec;6(4):215-9. [CrossRef][Google Scholar]
- Noble PC, Alexander JW, Lindahl LJ, et al. The anatomic basis of femoral component design. Clin Orthop Relat Res. 1988 Oct;(235):148-65[CrossRef][Google Scholar].
- Casper DS, Kim GK, Parvizi J, et al. Morphology of the proximal femur differs widely with age and sex: relevance to design and selection of femoral prostheses. J Orthop Res. 2012 Jul;30(7):1162-6. [CrossRef][Google Scholar]
- Clohisy JC, Nunley RM, Carlisle JC, et al. Incidence and Characteristics of Femoral Deformities in the Dysplastic Hip. Clin Orthop Relat Res. 2009 Jan;467(1):128-34. [CrossRef][Google Scholar]
- Kienapfel H, Sprey C, Wilke A, et al. Implant fixation by bone ingrowth. J Arthroplasty. 1999 Apr;14(3):355-68. [CrossRef][Google Scholar]




 Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.
Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.