Open supra-intercondylar fracture of the humerus in the elderly: Clinical case
Received: 09-Sep-2020 Accepted Date: Oct 23, 2020 ; Published: 06-Nov-2020
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Distal humerus fractures are more frequent in young men and elderly women, with known negative consequences, especially in the latter group, where multiple factors advocate poor results. Open reduction and internal fixation are considered the method of choice when eligible. We present a case of success with an aggressive approach to a difficult fracture.
Keywords
Distal humerus fractures, supra-intercondylar fracture, internal fixation, low-energy trauma
Introduction
Fractures of the distal humerus are relatively rare injuries (approximately 2% of all fractures) and have a bimodal distribution, with a predilection for young men involved in high-energy accidents and women over 60 with low-energy trauma [1,2].
In the geriatric population, in particular, this type of injury increases its, already high, degree of treatment difficulty, taking into account poor bone quality, low physiological reserve, poor soft tissue conditions, frequent complex involvement of the joint surface and less than ideal rehabilitation conditions [1-3]. Thus, fractures of the distal humerus in this group are associated with high rates of complications and poor functional results [3].
The main objective of treatment in these patients is to obtain a stable, painless and functional elbow, with an objective range of motion between 30º and 130º. In patients with conditions, osteosynthesis is the most used treatment, being, however, technically demanding and associated with risks and complications such as decreased mobility arch, cubital nerve damage, heterotopic ossification and pseudoarthrosis [4]. Open fractures are associated with a worse prognosis, requiring an early approach in the operating room [5].
In this clinical case, we evaluated the results of surgical treatment of an open fracture of the distal humerus in an elderly person with open reduction and internal fixation.
Clinical Case
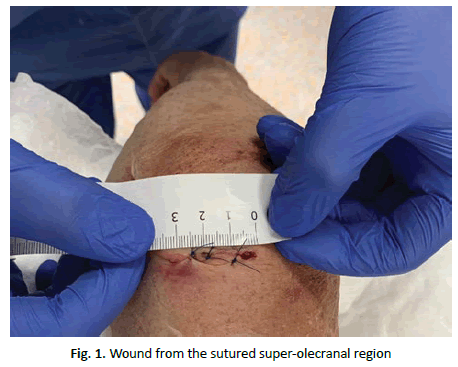
A 77-year-old woman went to the emergency department after falling from her own height with direct trauma to her left elbow. She had an evident local deformity, a deep wound in the supra-olecranal region (Fig. 1) and no apparent neurovascular deficits. The patient had a history of high blood pressure, dyslipidemia and Parkinson’s disease.
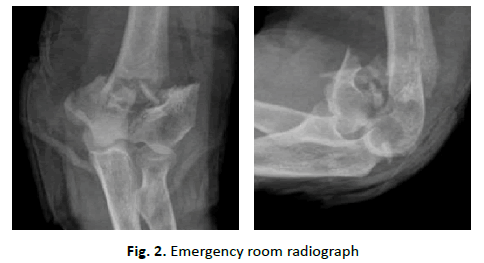
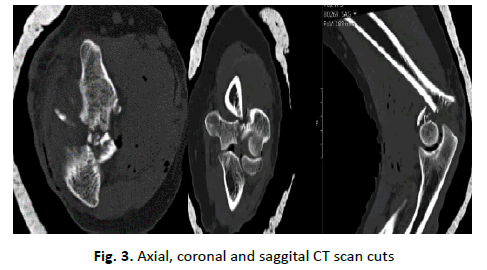
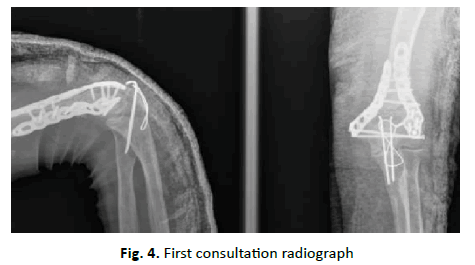
We performed a radiological study (Fig. 2), abundant washing, disinfection and wound closure, as well as immobilization with a cast splint. After observing the radiograph, which showed a supraintracondylar fracture of the distal humerus, CT of the elbow (Fig. 3) was performed to better characterize the injury and operative planning: Gustillo Anderson type II open fracture of the distal humerus, with a comminuted intra-articular component. The patient underwent surgical intervention, and an open reduction was performed using a posterior approach with olecranon osteotomy and internal fixation with posteromedial and lateral plates (Fig. 4).
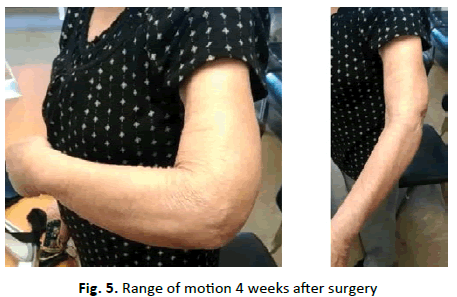
In the postoperative period, she used a plaster cast splint for 2 weeks, followed by progressive onset of passive elbow mobility, having started physical therapy at 3 weeks. She was observed in consultation with a radiograph 30 days after surgery, presenting no pain complaints, range of motion: Extension 15º-20º; 100º flexion (Fig. 5); Pronosupination with limitation of extreme pronation angles.
The patient agreed and collaborated with the elaboration of this article, having signed the informed consent form.
Discussion
The AO/OTA classification is used globally to define lesions of the distal humerus, characterizing the pattern, location and degree of joint involvement [6]. Type A corresponds to extra-articular injuries, type B to partially articular injuries and type C to completely articular injuries without continuity with the shaft. Type C3 lesions are comminuted, deviated and more often accompanied by severe soft tissue injury or exposure [3,7]. The population most affected by these injuries are independent and active post-menopausal female patients. Charissoux et al. [8] evaluated 410 patients over 65 years of age and found a correlation between age and more complex fracture patterns, namely, 67% incidence of type C fractures and 16% of open fractures.
The treatment of intra-articular fractures of the distal humerus is challenging and laborious, especially when aggravated by high comminution, multiple intra-articular fragments and poor bone quality [2]. There are multiple reports in literature about the good results of osteosynthesis of these lesions [2], however, many of these testimonies emphasize complication rates up to 25-30%, especially in elderly patients [1,2,4,5]. Comorbidities such as osteoporosis, diabetes mellitus and lesions of the surrounding soft tissues worsen the prognosis and hinder further rehabilitation [7].
Regarding the aggravating exposure of the lesion, it is described that open fractures are associated with worse functional scores, lower range of mobility, higher complication rates, more time until consolidation and greater need for reintervention.
In the face of complex lesions, such as that of the clinical case described, the therapeutic decision is not simple, namely the choice between early definitive treatment and temporary osteotaxy. Kosters et al. correlated the use of temporary external fixator with worse postoperative results, when compared with the definitive ad initium fixation [7]. Radoicic et al. evaluated the surgical timing, finding no significant differences in complications and outcomes in the operated group in less than 6 hours and the operated group on average 4,6 days later [9].
Although osteosynthesis is the default treatment for these injuries, there are reports of its inapplicability in about 25% of elderly patients [1,10]. In these cases, elbow arthroplasty is a hypothesis with proven results, particularly in women with comorbidities such as rheumatoid arthritis, osteoporosis or under systemic corticosteroids [10].
There are few studies evaluating the functional results after osteosynthesis of these injuries in elderly patients [3], and Korner et al. [3] states that immobilization for more than 15 days results in greater limitations of the range of motion and that early physical therapy acts as a positive factor in functional results. In this analysis, the mean range of mobility was 100º (55º-135º arc) for extension/flexion and 110º for pronation supination (60°-180° arc), values that were surpassed in the case reported here.
Conclusion
Intra-articular fractures of the distal humerus are feared in traumatology by several factors, not only for its intra-operatory technical difficulty but also by the subsequent functional results, especially in older patients. The authors seek to reinforce the possible good results with open reduction and early internal fixation, even when everything seems to predict the worst.
REFERENCES
- Varecka T.F., Myeroff C.: Distal humerus fractures in the elderly population. J Am Acad Orthop Surg. 2017;25:673-683.
- Virani S.R., Sonone S., Dahapute A.A., et al.: Functional results of communited intra-articular distal humerus fractures treated with bicolumnar plating. J Clin Diagn Res. 2017;11:RC01-RC03.
- Korner J., Lill H., Müller L.P., et al.: Distal humerus fractures in elderly patients: results after open reduction and internal fixation. Osteoporos Int. 2005;2:S73-S79.
- Greiner S., Haas N.P., Bail H.J.: Outcome after open reduction and angular stable internal fixation for supra-intercondylar fractures of the distal humerus: preliminary results with the LCP distal humerus system. Arch Orthop Trauma Surg. 2008;128:723-729.
- Min W., Ding B.C., Tejwani N.C.: Comparative functional outcome of AO/OTA type C distal humerus fractures: Open injuries do worse than closed fractures. J Trauma Acute Care Surg. 2012;72:E27-E32.
- Marsh J.L., Slongo T.F., Agel J., et al.: Fracture and dislocation classification compendium-2007: Orthopaedic Trauma Association classification, database and outcomes committee. J Orthop Trauma. 2007;21:S1-S133.
- Kösters C., Lenschow S., Schulte-Zurhausen E., et al.: Management of comminuted fractures of the distal humerus: clinical outcome after primary external fixation versus immediate fixation with locking plates. Arch Orthop Trauma Surg. 2017;137:1693-1698.
- Charissoux J.L., Vergnenegre G., Pelissier M., et al.: SOFCOT: Epidemiology of distal humerus fractures in the elderly. Orthop Traumatol Surg Res. 2013;99:765-769.
- Radoicic D., Micic I., Dasic Z., et al.: Does timing of surgery affect the outcome of open articular distal humerus fractures. Eur J Orthop Surg Traumatol. 2014;24:777-782.
- Frankle M.A., Herscovici D., DiPasquale T.G., et al.: A comparison of open reduction and internal fixation and primary total elbow arthroplasty in the treatment of intraarticular distal humerus fractures in women older than age 65. J Orthop Trauma. 2003;17:473-480.



 Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.
Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.