Percutaneous crossing screws, a novel technique for transverse patella fractures
2 Department of Orthopedic and Trauma Surgery, Al-Baha University, KSA, Email: abdulwahab@bu.edu.sa
Received: 03-Dec-2017 Accepted Date: Dec 18, 2017 ; Published: 21-Dec-2017
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: For the common transverse patella fractures, many stabilization techniques have been applied. The high frequency of complications underlines a problem that declares the need for a better fixation technique. This study describes a new technique using a percutaneous, or mini-invasive, cannulated crossing screws to solve this problem.
Material and Methods: Thirty-six patients with displaced transverse patellar fractures were managed with this technique. Their outcomes were evaluated clinically, radiologically, and functionally.
Results: The mean follow-up period was 22 ± 4.31 months. All the fracture united in a mean time of 7.6 ± 1.28 weeks. The average knee flexion was 134.10 ± 7.61 and 0.5° for extension. The mean Lysholm knee score was 94.5 ± 5.7. No major complications, cosmetic, or hardware problem.
Conclusions: The use of crossing screws simplifies fracture fixation, is mini-invasive, and provides stability enough to allow early range of motion exercises, with less injury to the extensor mechanism and better cosmetic scar.
Keywords
Patella fractures, Percutaneous, Crossing cannulated screws
Introduction
A high percentage of patella fractures have a transverse fracture pattern [1,2]. Although several stabilization techniques have been applied, the modified tension band wiring (MTBW) is vying for the lead. [1,3-8]. Despite several technical modifications of tension wiring, early fracture displacement was reported in 22% to 30% of cases [9]. The adverse effects such as the need for a long skin incision with extensive soft tissue dissection [4,6], increased surgical time and blood loss [7,10,11], the potential for blood supply damage [7,8,10], the need for subsequent prolonged rehabilitation [10-13], and hardware related complications with subsequent frequent need for implant removal (up to 65% of cases) resulted in amendable long-term results [8,12]. Such outcomes potentiate the continuous search for a better fixation techniques and invited introduction of several alternatives. Of those, inter-fragmentary parallel cannulated screws with or without tension wiring promised greater stability and a minimally invasive approach [10-14]. But, application of the screws in the same line of pull of the tension forces, especially with the need for early mobilization, puts a great demand over the screws and the wires or may lead to gradual loss of reduction and/or fixation (5). This study aimed to determine whether fixing the screws in a crossing manner could offer fracture compression with a stable fixation construct enough to withstand tension forces, maintain the initially obtained fracture reduction and compression, and improve the clinical, radiographic, and functional outcomes.
Materials and Methods
Between January 2011 and January 2014, 36 patients, 22 males and 14 females, incorporated in this interventional case-series prospective study. The inclusion criteria were: (1) AO/OTA34-C1 fractures (fractures with a primarily transverse fracture line); and (2) AO/OTA 34-C2 fractures (transverse fractures with a single additional longitudinal fracture line). The exclusion criteria included: (1) AO/OTA 34-C3 fractures (comminuted fractures); (2) open fractures; (3) previous knee injuries with stiffness; and (4) old fractures. Their mean age was 39 ± 11.45 years (range, 20 to 71 years). The mechanisms of injury were indirect trauma in 25 patients in slip down and motor vehicle accidents in 11 patients. Twenty-one patients had middle third fractures, 8 patients had their fracture in the distal third, and 7 in the proximal third. Twenty-six patients had AO/OTA34-C1 fractures, and 10 had AO/OTA34-C2 fractures. The outcomes of these patients were evaluated with simple radiographs, ROM measurements, and Lyshom score. Postoperative displacement was defined as a fracture site displacement of greater than 2 mm as compared to the position on the immediate postoperative imaging tests.
Ethics approval and consent
This study was performed in compliance with the Helsinki Declaration and has been granted approval from the Ethics Committee of our hospital. Written informed consent was obtained from all patients enrolled in this study.
Surgical technique
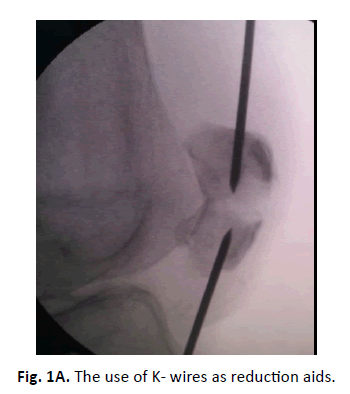
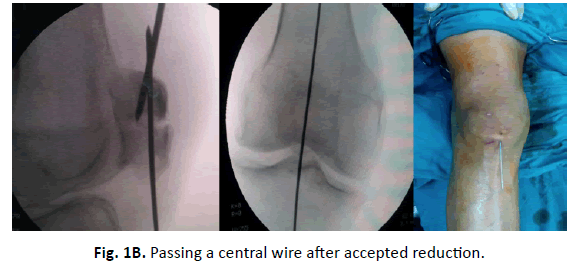
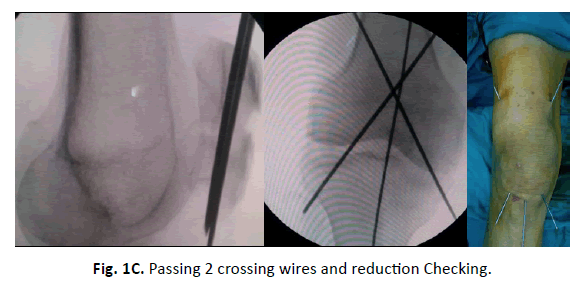
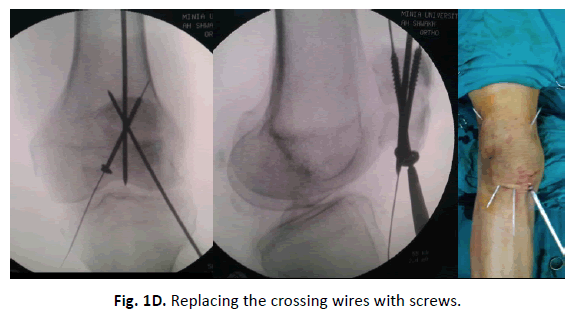
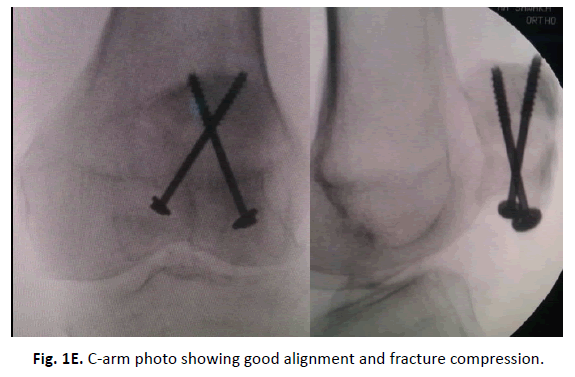
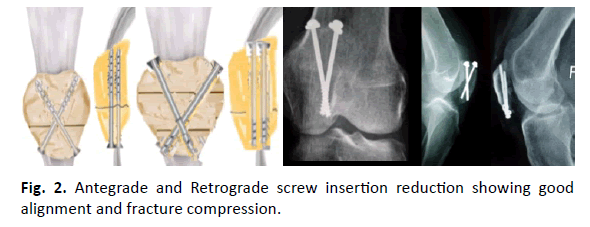
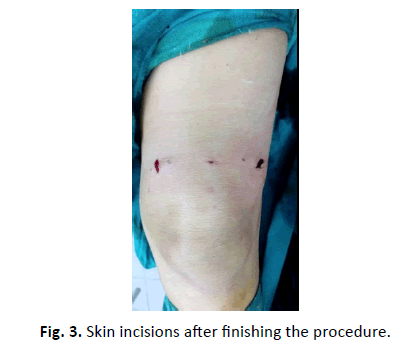
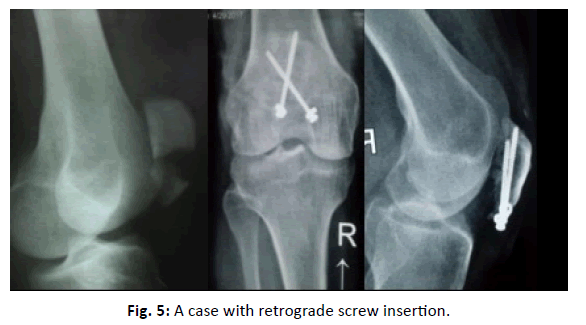
Under spinal anaesthesia, the patients were placed in supine position on a standard radiolucent operating table with the knee in full extension. One gram first generation cephalosporin was given, and no tourniquet was applied. Provisional alignment of the fractured patella was done by manipulation and evaluated by C-arm image intensifier to determine the two points suitable for screws insertion. At these points, 2 skin incisions, 5 mm each, at both sides of the patellar tendon were made. Through these skin incisions, hematoma was evacuated. Under C-arm image in-tensifier control, the fracture was anatomically reduced by manipulation only or with the help of reduction aids (Fig. 1A). If closed reduction failed a mini-incision (1-2 cm) can be made over the fracture site to help in anatomical reduction. If accepted, the reduction is maintained by a reduction clamp and augmented by passing a k-wire from inferior upward centered on the middle of the patella in AP and lateral C-arm views (Fig. 1B). Thereafter, two K-wires were drilled. In the AP view, these wires are crossing, nearly perpendicular to each other, and at about 45 degree to the fracture line. In the lateral view, the wires are nearly parallel, or crossing, and nearly perpendicular to the fracture line (Fig. 1-C). For easy and fast insertion, it is better to keep one of these wires anterior to the central wire and the other posterior to it. After satisfaction with fracture reduction and position of the K-wires, drilling was done along the guide wires with a cannulated drill bit, and two partially threaded 4.0 mm cannulated compression screws (Synthes Inc., West Chester, PA, USA) were inserted (Fig.1D). Every screw was advanced till its head be within 5 mm from the cortex, then both screws were tightened simultaneously (Fig.1E). The technique may be modified by adding additional screws in type AO/OTA 34-C2 fractures. The direction of the screws could be changed from antegrade to retrograde in high proximal or low distal fractures (Fig. 2). Stability of reduction and fixation was checked by image intensifier while flexing and extending the knee. The skin incisions after finishing the procedure revealed how much this approach is mini-invasive (Fig. 3). No suction drain was used, and after routine suturing of the skin, a cylinder splint was applied with 15-degree flexed knee position.
Post-operative management
All the patients were discharged home in the next day with an adjustable angle hinged knee brace allowing initial range of motion (ROM) of 0° to 45°. Then, the flexion angle was increased by about 15° to 20° weekly with the objective of reaching full flexion in 4 weeks. Immediately postoperatively, the patients were encouraged to start quadriceps setting exercises, active knee extension, with sequential increase. Quadriceps exercises against resistance were delayed for 6 weeks. Also, the patients were encouraged for nonweight bearing ambulation with crutches, partial weight bearing 3 weeks postoperatively, and full weight bearing after a radiographic evidence for fracture healing.
Statistical methods
SPSS 18 statistical software for Windows was used for all analyses. For comparison of the normally distributed variables, a two-tailed Student’s t-test was used; for non-normal distributions, the Mann– Whitney U test was used. Differences in proportions for categorical variables were assessed with the use of chi-squared tests. The p-value was set at a significance level of 0.05.
Results
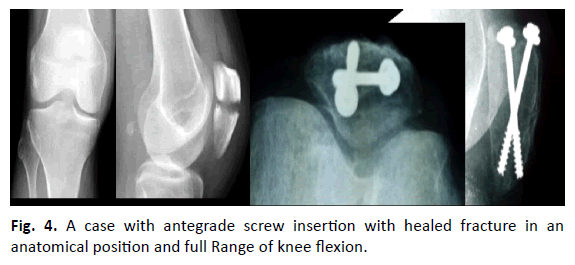
The mean follow-up period was 22 ± 4.31 months (range, 12 to 36 months). Closed reduction could be achieved in 30 patients, while mini-open incision was required in the other 6 patients. The mean operation time was 37.6 ± 6.54 min (range 25-60 min). All the fractures united. The mean radiographic union period was 9.6 ± 1.28 weeks (range, 6 to 12 weeks). In relation to the knee ROM, the average flexion was 134.10 ± 7.61 (range, 125° to 140°), and 0.5° for extension (range, -1° to 2°). No significant ROM differences were noted in comparison to the uninjured contralateral knee. The average Lysholm knee score was 94.5 ± 5.7 (range, 85 to 100). No major complications as significant limitation of the knee ROM, loss of reduction, failure or migration of hardware or deep infection were encountered. No cosmetic problem with surgical scars. One patient got superficial infection that did not involve the bone, joint, or implant, and was successfully treated on an outpatient basis with the use of antibiotics. Another two patients experienced skin irritation at the screw heads. They were reassured, and no one underwent hardware removal. Demographics were presented in Table 1, the results in Table 2, and the master sheet for all the cases in Table 3. Some cases were presented Fig. 4 and 5.
| S. No. | Sex | Age/Yr | Fracture level/third | Crossing screw direction | Fracture type as per AO/OTA | Operative Time / Min | Type of reduction | Time to union /Wk | follow up period/ Month | Lysholm knee score | Compli-cations |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | F | 47 | Mid | R | C1 | 30 | C | 10 | 15 | 90 | - |
| 2 | F | 30 | Mid | R | C1 | 45 | C | 12 | 28 | 100 | - |
| 3 | M | 36 | Mid | R | C1 | 40 | C | 10 | 16 | 95 | - |
| 4 | F | 22 | D | A | C2 | 60 | MO | 8 | 29 | 95 | - |
| 5 | M | 26 | Mid | R | C1 | 55 | C | 10 | 22 | 100 | - |
| 6 | M | 20 | Mid | R | C2 | 30 | C | 12 | 17 | 100 | - |
| 7 | F | 32 | P | A | C1 | 60 | C | 8 | 15 | 95 | - |
| 8 | M | 43 | Mid | R | C1 | 50 | C | 8 | 30 | 95 | - |
| 9 | M | 54 | Mid | R | C1 | 25 | C | 10 | 21 | 85 | - |
| 10 | M | 28 | D | A | C1 | 40 | C | 6 | 31 | 100 | - |
| 11 | F | 26 | Mid | R | C2 | 30 | MO | 12 | 16 | 95 | - |
| 12 | M | 37 | D | A | C2 | 45 | C | 8 | 29 | 95 | - |
| 13 | M | 26 | Mid | R | C1 | 50 | C | 8 | 30 | 100 | - |
| 14 | F | 42 | P | A | C1 | 35 | C | 12 | 30 | 90 | - |
| 15 | M | 29 | Mid | R | C1 | 45 | C | 10 | 16 | 100 | - |
| 16 | M | 43 | D | A | C1 | 40 | C | 12 | 24 | 90 | - |
| 17 | M | 71 | Mid | R | C1 | 50 | MO | 8 | 22 | 85 | SK I |
| 18 | M | 35 | D | A | C2 | 50 | C | 10 | 22 | 100 | - |
| 19 | F | 56 | P | A | C1 | 45 | C | 8 | 23 | 85 | - |
| 20 | M | 45 | Mid | R | C1 | 35 | C | 8 | 29 | 95 | - |
| 21 | M | 22 | Mid | R | C1 | 40 | MO | 10 | 21 | 100 | - |
| 22 | F | 32 | P | A | C1 | 40 | C | 12 | 28 | 95 | - |
| 23 | F | 20 | D | A | C2 | 35 | C | 10 | 16 | 100 | - |
| 24 | M | 27 | Mid | R | C1 | 40 | C | 10 | 22 | 100 | - |
| 25 | F | 34 | Mid | R | C1 | 30 | C | 10 | 15 | 95 | - |
| 26 | M | 41 | Mid | R | C1 | 25 | C | 12 | 16 | 90 | - |
| 27 | M | 20 | Mid | R | C2 | 50 | MO | 8 | 23 | 100 | - |
| 28 | M | 65 | P | A | C1 | 40 | C | 8 | 17 | 85 | Sk I |
| 29 | F | 33 | D | A | C1 | 30 | C | 8 | 30 | 95 | - |
| 30 | M | 22 | Mid | R | C2 | 35 | C | 12 | 16 | 100 | - |
| 31 | F | 36 | D | A | C1 | 40 | C | 12 | 22 | 90 | - |
| 32 | M | 23 | Mid | R | C2 | 40 | C | 8 | 23 | 100 | - |
| 33 | M | 44 | P | A | C1 | 50 | MO | 10 | 15 | 90 | Sk I |
| 34 | F | 58 | P | A | C1 | 55 | C | 10 | 32 | 85 | - |
| 35 | M | 26 | Mid | R | C2 | 40 | C | 12 | 16 | 100 | - |
| 36 | F | 24 | Mid | R | C1 | 50 | C | 8 | 23 | 100 | - |
M: Male, F: Female, Yr: Year, Wk: Week, Min: Minute, D: Distal, Mid: Middle, P: Proximal, A: Antegrade, R: Retrograde, MO: Mini-Open, C: Closed, SI: Superficial Infection, Sk: Skin Irritation.
Table 1:Patient baseline characteristics and outcome measures.
| Variables | Average | Range | |
|---|---|---|---|
| Age (years) | 39 ± 11.45 | 20-71 | |
| Mechanism of injury | |||
| Slip down | 25 | ||
| Motor vehicle accidents in | 11 | ||
| Side | |||
| Left | 20 | ||
| Right | 16 | ||
| Gender | |||
| Male | 19 | ||
| Female | 17 | ||
| AO classification | |||
| 34-C1 | 20 | ||
| 34-C2 | 16 | ||
Table 2: Basic characteristics of the patients.
| Variables | Average | Range |
|---|---|---|
| Follow up period (months) | 22±4.31 | 12-36 |
| Operation time (minutes) | 37.6±6.54 | 25-60 |
| Time to bone union (months) | 7.6±1.28 | 6-10 |
| Knee flexion | 134.10±7.61 | 125°-140° |
| Knee extension | 0.5° | 0°-3° |
| Lysholm knee score Hardware Removal |
94.5 ± 5.70 | 85-100 |
Table 3: Results.
Discussion
This study had many limitations. First, our technique was indicated for displaced transverse patellar fractures but is not recommended for other types of fractures as comminuted fractures. Second, this was an open-label trial, and the sample size was relatively small. Thus, this study design might be a cause of bias. Despite these limitations, we could get important findings. These included that percutaneous (PC) crossing screws technique allows the transfer of the tension force directly on to bone, and protects the tendon. Also, the study revealed positive clinical outcomes with primary union of all fractures, low implant-related complications, no fixation failure, or implant removal.
Most transverse patellar fractures result from excessive tensile force across the extensor mechanism and restoration of its competence is crucial to ensure an optimal outcome and patient satisfaction. Displaced fractures more than 8 mm are likely to be accompanied by disruption of the extensor mechanism [2,7]. So, closed reduction by indirect means may not be difficult, especially with less than 8 mm displacement [15].
Surgery is indicated if there is damage to the extensor mechanism or in fractures associated with more than 3-5 mm displacement or 2 mm articular surface step-off incongruity [16]. The main goal of the treatment of patella fractures is to provide a regular articular surface, to maintain a stable fixation that allow early knee ROM to preserve joint function [16].
Of the plethora of methods applied for treating transverse patellar fractures, MTBW through open surgical techniques was vying for the lead, but with many reported complications [12,16]. Because the patella is a subcutaneous bone, fixation devices (wires and wire knots) are frequently irritating to the soft tissues of the anterior knee area. So, PC applied screws may be less irritating. Also, stainless steel wire is a difficult material to manipulate through tissues and may result in soft tissue damage, blood supply jeopardize, and poor fracture fixation with a high rates of implant-related complications (up to 60%) [3], and necessitating implant removal up to 52% [17]. Most of these complications could be avoided with our technique and we agree with other authors [7,11] in that soft tissue irritation and elective implant removal could be reduced with the use of cannulated screws instead of K-wires. Others reported better clinical outcomes for cannulated screws when compared to the standard technique [15]. This may be attributed to the advantages of the percutaneous approach over the open technique as avoidance of extended incisions with less destruction of the soft tissues, preservation of the blood supply to the patella, less implant irritation to the soft tissues, reducing the risk of wound complications, and the possibility of a simpler hardware removal, if required. [4,6,7,15].
In relation to fixation stability, biomechanical investigations have revealed that the cancellous screws alone or in combination with tension band could provide a stable fixation [16,18]. Biomechanical comparison for fixation stability between screws and MTBW, suggested that parallel cannulated screws can provide a direct interfragmentary compression force, while the tension band wiring technique cannot achieve direct fracture site compression and can only transform distraction forces into compression forces, and may even lead to further fracture displacement [4]. The flexibility of K-wires can counteract a part of the force that should act on the fractured bone [4]. Especially under full knee extension, the K-wires in a tension wire system, may counteract a part of the force that should act on the fractured bone [4]. This counteraction may be aggravated by the concomitant presence of soft tissue atrophy and loss of muscle tone. Despite biomechanical superiority, Lin et al. [15] reported a postoperative interfragmentary gap in 6 of 26 patients received parallel cannulated screws and one with displacement. They did not attribute this to fixation failure secondary to an inadequate screw or in-appropriate placement. But, they suspected that the extremely poor bone quality and unlimited and aggressive early active mobilization contributed to that resultant failure. In our opinion, the repeated tension force may lead to gradual loss of the initial compression, gap, loss of reduction and displacement, as its line of pull is parallel to the screws. If the screws were applied in a crossing manner, the tension force when applied to the partially threaded screws will lead to pull in opposite directions. This, theoretically, may lead to dynamic fracture compression instead of gapping. In our study, no patient got gapping of displacement of the fractures.
In order to function properly, the patella must be able to withstand significant axial and distraction forces. Many studies reported that cannulated screws are more durable against distraction forces than the MTBW [19]. Moreover, the fractures stabilized with a MTBW may displace significantly more than those fixed with screws alone or screws plus a tension band in simulated knee extensions (p<0.05) [2,7,11,20]. The advantages of the partially-threaded screws could be more improved by the crossing mode of screw application. It could offer direct fracture compression in 2 planes with improvement of screw engagement that will be not only, able to withstand the axial and distraction forces, but also, allows for dynamic compression during knee ROM. The initial compression obtained in our cases, was not decreased or lost.
We agree with Luna-Pizarro et al [12] in that technical difficulty may represent a disadvantage of the PC fixation methods, and it may have a substantial learning curve. But, this difficulty may be less with screws alone if compared to PC tension band wiring [1,12]. Finally, technical errors in wire placement or wire twists have been identified as the cause of fixation failure with the use of PC techniques [9,11], which is suspected to be less with screws.
Lin, et al. [15] reported 11.5% complication rate with screws when compared to 53.4% for MTBW. The most common complications were painful hardware, tension band loosening, and K-wire migration, and elective hardware removal. They reported a reoperation rate of 11.5% in the screws group versus 42.3% in the MTBW group. In our study, no significant complications or reoperations were encountered.
Conclusion
Surgical treatment of transverse patella fractures with PC crossing cannulated screws combined the advantages of rigid internal fixation and minimally invasive surgery, and has shown to provide satisfactory clinical results and excellent knee functions, with less pain and low incidence of complications. It may be considered as an adequate alternative and a new option in the treatment of transverse patella fractures.
REFERENCES
- Hughes S.C., Stott P.M., Hearnden A.J., et al.: A new and effective tension-band braided polyester suture technique for transverse patellar fracture fixation. Injury. 2007;38:212-222.
- Chiang C.C., Chen W.M., Jeff Lin C.F., et al.: Comparison of a minimally invasive technique with open tension band wiring for displaced transverse patellar fractures. J Chin Med Assoc. 2011;74:316-321.
- Melvin J.S., Mehta S. et al.: Patellar fractures in adults. J Am Acad Orthop Surg. 2011;19:198-207.
- Tian Y., Zhou F., Ji H., et al.: Cannulated screw and cable are superior to modified tension band in the treatment of transverse patella fractures. Clin Orthop Relat Res. 2011;469:3429-3435.
- Baran O., Manisali M., Cecen B.: Anatomical and biomechanical evaluation of the tension band technique in patellar fractures. Int Orthop. 2009;33:1113-1117.
- Qi L., Chang C., Xin T., et al. Double fixation of displaced patella fractures using bioabsorbable cannulated lag screws and braided polyester suture tension bands. Injury. 2011;42:1116-1120.
- Tandogan R.N., Demirors H., Tuncay C.I., et al. Arthroscopic-assisted percutaneous screw fixation of select patellar fractures. Arthroscopy. 2002;18:156-62.
- Schuett D.J., Hake M.E., Mauffrey C., et al.: Current treatment strategies for patella fractures. Orthopedics. 2015;38: 377-384.
- Smith S.T., Cramer K.E., Karges D.E., et al.: Early complications in the operative treatment of patella fractures. J Orthop Trauma. 1997;11:183-187.
- Hoshino C.M., Tran W., Tiberi J.V., et al.: Complications following tension-band fixation of patellar fractures with cannulated screws compared with Kirschner wires. J Bone Joint Surg Am. 2013;95:653-659.
- Mao N., Liu D., Ni H., et al.: Comparison of the cable pin system with conventional open surgery for transverse patella fractures. Clin Orthop Relat Res. 2013;471:2361-2366.
- Luna-Pizarro D., Amato D., Arellano F., et al.: Comparison of a technique using a new percutaneous osteosynthesis device with conventional open surgery for displaced patella fractures in a randomized controlled trial. J Orthop Trauma. 2006;20:529-535.
- Lazaro L.E., Wellman D.S., Sauro G., et al.: Outcomes after operative fixation of complete articular patellar fractures: assessment of functional impairment. J Bone Joint Surg Am. 2013;95:e96.
- Berg E.E.: Open reduction internal fixation of displaced transverse patella fractures with figure-eight wiring through parallel cannulated compression screws. J Orthop Trauma. 1997;11:573-576.
- Tao Lin., Junbin Liu., Baojun Xiao., et al.: Comparison of the outcomes of cannulated screws vs. modified tension band wiring fixation techniques in the management of mildly displaced patellar fractures. BMC Musculoskelet Disord. 2015;16:282.
- Carpenter J.E., Kasman R.A., Patel N., et al: Biomechanical evaluation of current patella fracture fixation techniques. J Orthop Trauma. 1997;11:351-356.
- LeBrun C.T., Langford J.R., Sagi H.C.: Functional outcomes after operatively treated patella fractures. J Orthop Trauma. 2012;26:422-426.
- Dargel J., Gick S., Mader K., et al.: Biomechanical comparison of tension band-and inter-fragmentary screw fixation with a new implant in transverse patella fractures. Injury. 2010;41:156-160.
- Baydar M.L., Atay T., Gurbuz O.: Compressive screwing of transverse patella fractures provides better resistance to traction than tension band. Eur J Orthop Surg Traumato. 2011;21:105-110.
- Domby B., Henderson E., Nayak A., et al.: Comparison of cannulated screw with tension band wiring versus compressive cannulated locking bolt and nut device (Compressure) in patella fractures-a cadaveric biomechanical study. J Orthop Trauma. 2012;26:678-683.



 Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.
Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.