Prospective study to compare and correlate the clinical, MRI, and arthroscopic finding in patients with knee injuries
2 Amandeep Hospital, Amritsar, Punjab, India, Email: dharmesh_19872003@yahoo.co.in
Received: 20-Mar-2021 Accepted Date: Apr 14, 2021 ; Published: 27-Apr-2021, DOI: 10.37532/1897-2276.2021.16(1).15
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Aim and Objective: To compare and correlate the clinical, MRI, and arthroscopic findings in patients with knee injuries. Introduction: Internal derangement of the knee (traumatic or degenerative) are a very common entity. Diagnostic modalities used most commonly to assess and evaluate joint injuries are arthroscopy and MRI. Arthroscopy, though invasive and can cause complications, is considered a gold standard. MRI has now been accepted as the best imaging modality for the non-invasive evaluation of knee injuries. Arthroscopy is the gold standard. Material and Methods: 48 patients (50 knees) with a history of knee injuries taken, detailed history, and relevant clinical examination of all the subjects were recorded. All patients underwent MR Imaging and arthroscopy and considering arthroscopy as the gold standard, Clinical findings were compared with MRI and arthroscopic findings. Results: The accuracy of MRI Knee for ACL, PCL, Medial meniscus, and Lateral meniscus injuries when compared with arthroscopy was 90.0%, 94.0%, 78.0%, and 90.0%. The accuracy of clinical examination for ACL, PCL, Medial meniscus, and Lateral meniscus injuries, when compared with arthroscopy, was 92.0%, 100.0%, 74.0%, and 90.0%. The accuracy of clinical examination for ACL, PCL, Medial meniscus, and Lateral meniscus injuries, when compared with MRI findings, was 92.0%, 100.0%, 96.0%, and 92.0%. 48 cases (50 knees) with a mean age of 31.90 years (18-55 yr). All the subjects of our study were of active age group with a peak incidence of 29.2% occurring in the age group 21- 30 years. Right knee (60%) involved more than left with male (70%) predominance females (30%), male to female ratio of 2.3:1. The present study showed that sports injuries accounted for the highest number of patients (58%) followed by slipping injuries and roadside accidents (36%). Conclusion: In conclusion, the present study supports that the clinical examination if done properly has almost the same value as MRI (which is a useful non-invasive modality having high diagnostic accuracy, sensitivity, and negative predictive value, making it a very reliable screening test for diagnosing ligamentous and meniscus injuries). MRI is unique in its ability to evaluate the structures not accessible on arthroscopy like evaluation of bone contusions and collateral ligaments.
Keywords
arthroscopy, knee injury, ACL (Anterior Cruciate Ligament), PCL (Posterior Cruciate Ligament), MRI (Magnetic Resonance Imaging), medial meniscus, lateral meniscus, MCL (Medial Collateral Ligament), LCL (Lateral Collateral Ligament)
Introduction
Internal derangement of the knee (traumatic or degenerative) is a very common entity and may require certain studies for the establishment of diagnosis, in addition to clinical history and a thorough physical examination. Clinical examination, performed by an experienced examiner, can have equal or even more diagnostic accuracy compared to MRI to evaluate meniscal lesions [1]. The use of arthroscopy improves the accuracy of the diagnosis but is invasive and can cause complications [2]. Diagnostic arthroscopy is an important advance, improving diagnostic accuracy from 64% to 94%. However, it is an invasive procedure, with the possible complications of infection, hemarthrosis, adhesions, and reflex sympathetic dystrophy [3].
MRI examination is now routinely used to assess a wide spectrum of internal knee derangements and articular disorders and has virtually replaced conventional arthroscopy in the evaluation of the menisci and the cruciate ligaments, decreasing both morbidity and costs associated with negative arthroscopic examinations. MRI provides information that can be used to grade pathology, guide therapy, prognosticate conditions, and evaluate treatment for a wide variety of orthopedic conditions in the knee. Thus, MRI is a very useful-invasive diagnostic modality having highs sensitivity, specificity, and accuracy in the identification of meniscal and cruciate ligament injuries [4].
The comparison of MRI diagnosis and surgical/clinical findings has always been a challenge for the health professions. A review of the available literature suggests that several studies are looking at two out of the three diagnostic tools (clinical examination, MRI scan, and arthroscopy) and only limited studies are available taking all of them together [5]. MRI is an accurate and cost-effective means of evaluating a wide spectrum of knee injuries, ranging from cruciate-collateral ligament injuries to cartilage deficiencies [6].
The present study is designed to compare and correlate these three methods in the diagnosis of ligamentous knee injuries.
Materials and Methods
The study was conducted in the Department of Orthopedics, Amandeep Hospital, Amritsar, Punjab from Dec 2015 to Nov 2016 (1 year) on patients coming to orthopedics OPD after obtaining the ethical clearance from the institutional ethical committee and after taking informed consent from the patients.
The hypothesis taken was that when the clinical examination was done by an experienced surgeon then MRI could be optional for low socioeconomic patients. Previously researchers have performed studies on the clinical, MRI & arthroscopic findings in knee injuries. Therefore, assuming p=85% as the sensitivity of Clinical and MRI findings correlating with Arthroscopic findings with a 10% margin of error, the minimum required sample size at 5% level of significance is 48 patients [7, 8].
Data between the groups were compared using the Chi-squared test or Fisher’s exact test appropriately. The sensitivity, specificity, PPV, and NPV were calculated to analyze the diagnostic value of Clinical, MRI findings correlating with Arthroscopy findings. For all statistical tests, a p-value less than 0.05 was taken to indicate a significant difference.
Inclusion Criteria
Patients (18-60 years) general patient and sportsperson coming to orthopedics OPD of Amandeep Hospital, Amritsar with history of trauma to knee undergoing cruciate ligamentous and meniscal knee injury and having MRI and underwent arthroscopy within 5 days of MRI. Clinical examination was done at the time of presentation of the patient to the orthopedics OPD by the clinical examinee.
Exclusion Criteria
Patient with recurrent arthroscopic surgery, major knee trauma (fracture around the knee) other than internal derangement of the knee, nontraumatic pathologies in the knee. Patients with the implant in situ at distal femur, patella and proximal tibia.
Methodology
Total 48 patients (50 knees) had undergone a primary thorough clinical examination after taking history. Case Reporting Form was developed and used to generate data. All patients with a history of trauma and clinical suspicion of ligamentous injuries are subjected to MRI from a dedicated Imaging Centre followed by arthroscopy within 5 days by the single arthroscopic surgeon (not by clinical examinee) so that result remains biased at Amandeep Hospital Amritsar.
Clinical criteria used were history, tender joint line, and positive McMurray’s test for meniscal injury. Anterior drawer test, Lachman test, pivot shift, and posterior drawer test was considered essential for clinical diagnosis of anterior cruciate ligament injury and posterior cruciate ligament injury respectively. Valgus stress test and Varus stress test were done for clinical diagnosis of medial collateral ligament and lateral collateral ligament respectively. Rotational instability tests were not included. After excluding any contraindication to MR imaging, MRI has done at:
• 1.5 Tesla Scanner at the dedicated imaging center
• GRE T2 W sequence in the coronal plane
• Proton density fat-saturated sequence in the sagittal plane
• FS proton density sequence in the axial plane
• Different sequences with a slice thickness of 4 mm-5 mm
The arthroscopic examination was carried out by single Ortho-surgeon through the use of two inferior para-patellar portals under general/or spinal anesthesia. A routine sequence was the evaluation of the patellafemoral joint and examination of the intercondylar notch. Further, the medial and lateral compartments were evaluated for osseous, cruciate, and meniscal abnormalities. Arthroscopic findings were regarded as the gold standard. Record of clinical, MRI, and arthroscopic findings was kept and compared. The statistical analysis was done by using software SPSS version 22.0. Sensitivity, specificity, positive predictive value, and negative predictive value were calculated.
MRI Findings
1. The cruciate ligament was described as either intact, relaxed, partial tear, or complete tear.
Following signs were used to diagnose different types of ACL tears:
• General or focal increased signal intensity
• Absence/non-visualization of ACL
• Alteration of course of ACL
• In acute ACL tears (<8 weeks) because of edema and hemorrhage, increased signal
• intensity on T2W images was seen along with the mass in the expected location of the ACL. Focal or diffuse disruption indicates complete acute ACL tear
• Following signs were used to diagnose chronic ACL tears: Absence of edema/hemorrhage, Variable sized, distal ACL fragment lying along the proximal tibia directed towards the PCL, Indirect signs may also be present and include anterior tibial subluxation, buckling of the PCL, and cruciate ligament cyst
2. Following sign were evaluated for determining the PCL status: Buckled PCL: The PCL was considered to be buckled if any portion of the posterosuperior border was concave. On sagittal T2-weighted images, anteroposterior diameter of 7 mm or more is highly suggestive of a torn PCL. Increased intra substance signal intensity in the PCL on proton-density images with lower signal intensity on T2-weighted images
3. MRI grading of meniscal tears and degenerations: A grading system based on the signal abnormality correlated with histopathological abnormalities has been developed to understand the significance of increased signal intensity patterns in meniscal abnormalities [9, 10]
• Grade I: Non-articular focal or globular intrasubstance increased signal intensity in the non-articular portion of the meniscus
• Grade II: Horizontal linear intrasubstance increased signal intensity usually extends from the capsular periphery but does not involve an articular surface
• Grade III: Region of abnormal signal intensity extends or communicates to at least one of the articular surfaces
• Grade IV: It is sometimes added to indicate a complex tear with multiple components or fragmentation
4. MRI appearance of meniscal tears:
• Horizontal Tears: These are parallel to the tibial plateau and divide the meniscus into upper and lower segments.
• Vertical Tears: They are perpendicular to the tibial plateau
• Root tears: They are full-thickness radial tears at the central tibial attachment sites of the menisci & are called the root ligaments
• Bucket-handle tears: These are displaced longitudinal tears. The displaced fragment often has the appearance of a handle, and the remaining peripheral segment attached to the tibial resembles a bucket-hence the name.
• Complex tears: They either have two or more tear configurations or are not categorized easily into a certain type of tear.
5. MRI grading of Medial Collateral Ligament (MCL) [6]:
• Grade I: Lesions are defined as high signal intensity superficial to the MCL representing edema, with intact MCL fibers.
• Grade II: Lesions in which fluid signal extend partially through the MCL, although some fibers remain intact
• Grade III: Lesions with complete discontinuity of the MCL fibers seen along with surrounding edema, consistent with a complete
6. Lateral Collateral Ligament (LCL): Lateral collateral ligament injuries were classified similarly as medial collateral ligament lesions, using the 3-point grading system as outlined above. rupture.
Results
48 cases (50 knee) with mean age was 31.90 years (18-55 yr). All the subjects of our study were of active age group with peak incidence of 29.2% occurring in age group 21-30 years. Right knee 60% involved more then left with males (70%) predominance females (30%), male to female ratio of 2.3:1.The present study showed that the sports injuries accounted for the highest number of patients (58%) followed by slipping injury and road side accident (36%).
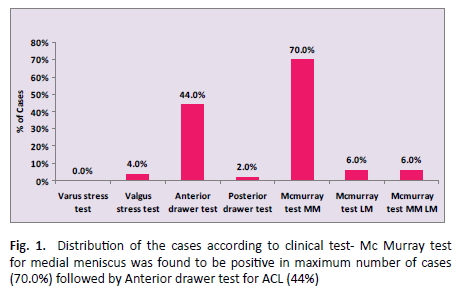
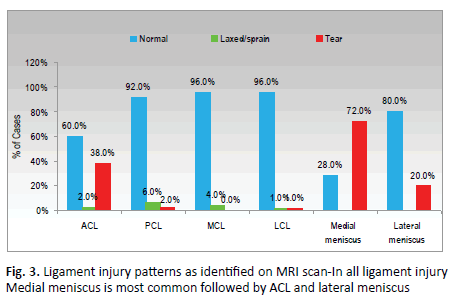
In our study clinically we find medial meniscus tear(70%) LM tear (6%), ACL tear (44%), PCL tear (2%),LCL tear (4%) (Figure 1), on MRI ACL tear was found in 19 patients (38%), Posterior cruciate ligament less common (8%). MCL tears (4%), LCL tear (2%) and all showed partial tear with similar incidence of grade I and grade II signal intensity (50%). Medial meniscal injuries was in 36 cases (72%), Lateral meniscal injury was found in 10 cases (20%). We found 15 cases of combined injuries and the most common combination was found to be ACL- MM injury seen in 40% of the cases followed by ACL-LM and PCL- LM accounting for 13.33% each. On arthroscopy the occurrence of medial meniscal tear was found to be more common (50%) followed by ACL tear (38%) amongst all the cases whereas lateral meniscus tear was seen in 10% of cases (Figure 2). MRI detected 19 cases of ACL injury, arthroscopy confirmed also 19 cases. Sensitivity and specificity of MRI with respect to arthroscopy was 89.5% and 90.3% respectively with diagnostic accuracy of 90%. Diagnostic accuracy of MRI was 78% for medial meniscus and 90% for lateral meniscus (Figure 3). It was observed that the most common combination was ACL-MM injury which was seen in 40% of the cases followed by ACL-LM and PCL-LM accounting for 13.33% each.
The accuracy of MRI Knee for ACL, PCL, Medial meniscus and Lateral meniscus injuries when compared with arthroscopy was 90.0%, 94.0%, 78.0% and 90.0% (Table 1).
MRI |
ARTHROSCOPIC FINDINGS | p value | |||
| Tear | Normal | ||||
| Frequency | % | Frequency | % | ||
| ACL | |||||
| TEAR | 17 | 0.895 | 3 | 0.097 | <0.001 |
| Normal | 2 | 0.105 | 28 | 0.903 | |
| Total | 19 | 1 | 31 | 1 | |
| PCL | |||||
| TEAR | 1 | 1 | 3 | 0.061 | <0.001 |
| Normal | 0 | 0 | 46 | 0.939 | |
| Total | 1 | 1 | 49 | 1 | |
| Medialmeniscus | |||||
| TEAR | 25 | 1 | 11 | 0.44 | <0.001 |
| Normal | 0 | 0 | 14 | 0.56 | |
| Total | 25 | 1 | 25 | 1 | |
| Lateralmeniscus | |||||
| TEAR | 5 | 1 | 5 | 0.111 | <0.001 |
| Normal | 0 | 0 | 40 | 0.889 | |
| Total | 5 | 1 | 45 | 1 | |
| Senstivity | Specificity | PPV | NPV | Accuracy | |
| ACL | 0.895 | 0.903 | 0.85 | 0.933 | 0.9 |
| PCL | 1 | 0.939 | 0.25 | 1 | 0.94 |
| Medial meniscus | 1 | 0.56 | 0.694 | 1 | 0.78 |
| Lateral meniscus | 1 | 0.889 | 0.5 | 1 | 0.9 |
Table 1. Correlation of MRI and arthroscopy findings.
The accuracy of clinical examination for main ligaments ACL, PCL, Medial meniscus and Lateral meniscus injuries when compared with arthroscopy was 92.0%, 100.0%, 74.0% and 90.0%. (Table 2).
Clinical |
ARTHROSCOPIC FINDINGS | p value | |||
|---|---|---|---|---|---|
| Tear | Normal | ||||
| Frequency | % | Frequency | % | ||
| ACL | |||||
| TEAR | 18 | 0.947 | 3 | 0.097 | <0.001 |
| Normal | 1 | 0.053 | 28 | 0.903 | |
| Total | 19 | 1 | 31 | 1 | |
| PCL | |||||
| TEAR | 1 | 1 | 0 | 0 | 0.02 |
| Normal | 0 | 0 | 49 | 1 | |
| Total | 1 | 1 | 49 | 1 | |
| Medial meniscus | |||||
| TEAR | 25 | 1 | 13 | 0.44 | <0.001 |
| Normal | 0 | 0 | 12 | 0.56 | |
| Total | 25 | 1 | 25 | 1 | |
| Lateral meniscus | |||||
| TEAR | 3 | 0.6 | 3 | 0.067 | 0.009 |
| Normal | 2 | 0.4 | 42 | 0.933 | |
| Total | 5 | 1 | 45 | 1 | |
| Senstivity | Specificity | PPV | NPV | Accuracy | |
| ACL | 0.947 | 0.903 | 0.857 | 0.966 | 0.92 |
| PCL | 1 | 1 | 1 | 1 | 1 |
| Medial meniscus | 1 | 0.48 | 0.658 | 1 | 0.74 |
| Lateral meniscus | 0.6 | 0.933 | 0.5 | 0.955 | 0.9 |
Table 2. Correlation of clinical and arthroscopy findings.
The accuracy of clinical examination for ACL, PCL, Medial meniscus and Lateral meniscus injuries when compared with MRI Findings was 92.0%, 100.0%, 96.0% and 92.0%(Table 3).
Clinical |
MRI | p value | |||
|---|---|---|---|---|---|
| Tear | Normal | ||||
| Frequency | % | Frequency | % | ||
| ACL | |||||
| TEAR | 18 | 0.947 | 3 | 0.097 | <0.001 |
| Normal | 1 | 0.053 | 28 | 0.903 | |
| Total | 19 | 1 | 31 | 1 | |
| PCL | |||||
| TEAR | 1 | 1 | 0 | 0 | 0.02 |
| Normal | 0 | 0 | 49 | 1 | |
| Total | 1 | 1 | 49 | 1 | |
| Medial meniscus | |||||
| TEAR | 36 | 1 | 2 | 0.143 | <0.001 |
| Normal | 0 | 0 | 12 | 0.857 | |
| Total | 36 | 1 | 14 | 1 | |
| Lateral meniscus | |||||
| TEAR | 6 | 0.6 | 0 | 0 | <0.001 |
| Normal | 4 | 0.4 | 40 | 1 | |
| Total | 10 | 1 | 45 | 1 | |
| Senstivity | Specificity | PPV | NPV | Accuracy | |
| ACL | 0.947 | 0.903 | 0.857 | 0.966 | 0.92 |
| PCL | 1 | 1 | 1 | 1 | 1 |
| Medial meniscus | 1 | 0.857 | 0.947 | 1 | 0.96 |
| Lateral meniscus | 0.6 | 0.889 | 1 | 0.909 | 0.92 |
Table 3. Correlation of clinical and MRI findings.
Discussion
48 cases (50 knees) with a mean age were 31.90 years (18 years-55 years). All the subjects of our study were of active age group involved in various kinds of day-to-day physical activities making them prone to knee injuries with a peak incidence of 29.2% occurring in the age group 21 years-30 years in our study. This was in concordance with the studies done by [9-11]. This study showed that the right knee 60% involved more than left with males (70%) predominance females (30%), male to female ratio of 2.3:1.
The present study showed that sports injuries accounted for the highest number of patients (58%) followed by slipping injuries and roadside accidents (36%). In other studies done by [12-15] showed that the maximum number of subjects had sports-related knee injury accounting for 45%, 55%, 48% and 50% cases respectively.
In our study on MRI ACL tear was found in 19 patients (38%), Posterior cruciate ligament injuries were found to be relatively less common (8%). In our study, MCL tears (4%) were found to be more common than the LCL tear (2%) and all showed partial tear with a similar incidence of grade I and grade II signal intensity (50%). This was in disconcordance with the study done which showed that on MRI out of 30 cases 11 patients LCL tear and 7 patients had a tear of MCL [16].
In our study, medial meniscal injuries were found in 36 cases (72%). The lateral meniscal injury was found in 10 cases (20%). There is a preponderance of MM tears over LM tears in our study which is well correlated with the study done by [17] in a series of 173 cases of which they found 57 (38.23%) patients showed MM tear and 28 (29.41%) patients showed LM tear.
In our study showed, we found 15 cases of combined injuries, and the most common combination was found to be ACL-MM injury seen in 40% of the cases followed by ACL-LM and PCL-LM accounting for 13.33% each. This was in concordance with the study by [18], which showed 17 cases of concomitant injuries on MRI with the commonest combination of anterior cruciate ligament rupture and medial meniscus tear (38%). On arthroscopy, the occurrence of medial meniscal tear was found to be more common (50%) followed by ACL tear (38%) amongst all the cases whereas lateral meniscus tear was seen in 10% of cases.
In our study, MRI detected 19 cases of ACL injury, arthroscopy confirmed also 19 cases. The sensitivity and specificity of MRI concerning arthroscopy were 89.5% and 90.3% respectively with a diagnostic accuracy of 90%. The accuracy of MRI knee for PCL injuries, when compared with arthroscopy, was 94%. Diagnostic accuracy of MRI was 78% for medial meniscus and 90% for lateral meniscus in our study which corresponds to studies done by [19] 73% for MM and 78.5% for LM, [16] 74% for MM, and 94% for LM, [20] 77% for MM and 91% for LM, [21] 82% for MM and 88% for LM and [22] 86% accuracy rate for menisci.
In our study, the accuracy of clinical findings in ACL injuries and PCL injuries when compared with arthroscopy was 92% and 100% respectively. The accuracy of clinical findings for both medial meniscal injuries and lateral meniscal injuries when compared with arthroscopy was 74% and 90% respectively. This was in concordance with the study done in Kathmandu by [23], which showed that the sensitivity, specificity, diagnostic accuracy of clinical examination were 96.1%, 33.3%, and 73.1% respectively for medial meniscal tear; 38.4%, 96.4%, and 78.1% respectively for lateral meniscal tear. The sensitivity, specificity, diagnostic accuracy of MRI were 100%, 56%, and 78% for medial meniscal tear; 100%, 88.9%, and 90% respectively for lateral meniscal tear.
Conclusion
In conclusion, the clinical examination is an important diagnostic tool, and its sensitivity and specificity for MM, LM, ACL, and PCL are respectively when compared to arthroscopy. Our clinical examination emphasizes that after doing a good clinical examination by expertise the patient may be taken for surgery when they cannot afford MRI.
With a combination of MRI, Clinical examination the treatment plan can be formulated in most of the patient and both diagnostic and arthroscopic treatment can be done at the same sitting.
The present study supports that MRI helps diagnose meniscal and cruciate ligament injuries most important for diagnosing MCL and LCL injuries. Undoubtedly new techniques and more powerful tomograms will improve MRI’s accuracy leading to better diagnostic accuracy in knee injuries. But one cannot be left behind only with techniques; we should not forget the part of a good clinical and history as they are very important.
Although we did not diagnostic arthroscopy after clinical examination and MRI only diagnostic arthroscopy must be done when there is a discrepancy between clinical and MRI finding and patients continue to have their sign symptoms which can alter the treatment plan.
MRI is unique in its ability to evaluate the structures not accessible on arthroscopy like evaluation of bone and collateral ligaments.
Conflict of Interest
No Conflict of Interest
REFERENCES
- Hashemi S.A., Ranjbar M.R., Tahami M., et al.: Comparison of Accuracy in Expert Clinical Examination versus Magnetic Resonance Imaging and Arthroscopic Exam in Diagnosis of Meniscal Tear. Adv Orthop. 2020;2020:1-5.
- Chivers M.D., Howitt S.D.: Anatomy and physical examination of the knee menisci: a narrative review of the orthopaedic literature. J Can Chiropr Assoc. 2009;53:319-333.
- Keith L.M., Dalley A.F.: Lower Limb in: Clinically oriented Anatomy: 5th ed. Lippincott Williams and Wilkins. 2006;555-725
- Freiberger R.H., Killoran P.J., Gonzalo C.: Arthrography of the knee by double contrast method. Am J Roentgenol. 1966;97:736-747.
- Hamish G. and David S.: Precision in the diagnosis of meniscal lesions: a comparison of clinical evaluation, Arthrography and Arthroscopy. J Bone Joint Surg.1979;61:343-346.
- Khan H. A., Ahad H., Sharma P., et al.: Correlation between magnetic resonance imaging and arthroscopic findings in the knee joint. Trauma Month. 2015;20:e18635
- Gupta S., Sharma R., Sachar A., Saini Y., Saini N.: Comparison of clinical examination, mri and arthroscopy in knee injuries. Internet J Ortho Surg. 2012;19:3
- Gupta K., Kulkarni P.N., Ratil N.: Comparison of MRI findings with arthroscopy finding in internal derangement of knee. Int J Rec Trends Sci Tech. 2013;9:159-163
- Clayton R.A., Brown C.M.: The epidemiology of musculoskeletal tendinous and ligamentous injuries. Injury. 2008;39:1338-1344.
- LaPrade R.F., Wentorf F.A., Gundry C., et al.: A prospective MRI study of the incidence of posterolateral and multiple ligament injuries in acute knee injuries presenting with a hemarthrosis. Arthroscopy. 2007; 23:1341-1347.
- Incesu L., Dabak N., Belet U. et al: Comparision of MRI and arthroscopic findings in knee joint pathologies. Turk J Med Res. 1997;15:21-25.
- Kannus P., Jarvinen M.: Incidence of knee injuries and the need for further care: a one year prospective follow up study. J Sports Med Phys Fitness.1989;29:321-25.
- Nielsen A.B., Yde J.: Epidemiology of acute knee injuries: a prospective hospital investigation. J Trauma. 1991;31:1644-1648
- Yawn B.P., Amadio P., Harmsen W.S. et al: Isolated acute knee injuries in the general population. J Trauma. 2000;48:716-723.
- Ansari M.Z., Ahee P., Iqbal M.Y., et al.: Traumatic haemarthrosis of the knee. Eur J Emerg Med. 2004;11:145-147.
- Glashow J.L., Katz R., Schnieder M. et al.: Double-blind assessment of the value of magnetic resonance imaging in the diagnosis of anterior cruciate and meniscal lesions. J Bone Joint Surg Am. 1989; 71: 113-119.
- Singh J.P., Garg L., Shrimali R., et al.: MR Imaging of knee with arthroscopic correlation in twisting injuries. IJRI. 2004;4:33-40.
- EsmailiJah A.A., Sohrab K., Zarei R., et al: Accuracy of MRI in comparison with Clinical and Arthroscopic findings in ligamentous and meniscal injuries of the knee. Acta Orthop Belg. 2005;71:189-196.
- Behairy N.H., Dorgham M.A., Sherif A.K.: Accuracy of routine MRI in meniscal and ligamentous injuries of the knee: comparison with arthroscopy. IntOrthop SICOT. 2009;33:961-967.
- Reppeport E.D., Mehta S., Wieslander S.B. et al.:MR imaging before arthroscopy in knee joint disorders. Acta Radiol. 1996;37: 602-629.
- Kinnunen J., Bondestam S., Kivioja A., et al.: Diagnostic performance of low field MRI in acute knee injuries. Magn Reson Imaging. 1994;12:1155-1160.
- Incesu L., Dabak N., Belet U., et al.: Comparision of MRI and arthroscopic findings in knee joint pathologies. Turk J Med Res. 1997;15:21-25.
- Sharma U.K., Shrestha B.K., Rijal S., et al. Clinical, MRI and arthroscopic correlation in internal derangement of knee.Acta Orthop Belg. 2005;71:189-196




 Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.
Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.