Replacing the entire femur for the cancer treatment of the lower femur: reporting one clinical case
2 K Central Hospital, Vietnam
3 Saint Paul Hospital, Vietnam
Received: 07-May-2020 Accepted Date: Jun 19, 2020 ; Published: 28-Jun-2020
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: Replacing the entire femur is the replacement of the entire femur of the patient with the artificial femur, and replacement of hip and knee joint. This is a rare, complicated surgery that is often indicated in bone cancer to preserve the lower limbs of the patient.
Case Report: A 24-year-old female patient. Diagnosis: Right femur osteosarcoma. The patient was treated with the preoperative chemicals according to the EOI regimen. The patient had surgery to remove the entire femur and replace it with an artificial femur. After 3 months, the patient could walk on their own with the crutches, no pain, the incision was good. The knee joint ROM is 0°-10°-90°. MSTS score reached 25/30 points. There were no signs of tumor recurrence, infection, dislocation.
Conclusion: This is the first clinical case to be realized in Vietnam. The replacement of the entire femur is a major surgery, requiring a careful evaluation of the injury and an elaborate treatment planning. This is our experience in diagnosing and treating bone cancer.
Keywords
Osteosarcoma, total femur replacement, endoprosthetic reconstruction
Introduction
Bone cancer is a malignant tumor originating from the bone-forming cells. Osteosarcoma is the most common primary tumor in malignant diseases of the musculoskeletal system, often appearing in young patients, mainly at the age of 10-14 [1]. The current treatment regimen combines chemicals and surgery. Pre-surgical chemicals kill micro metastatic malignant cells. After being treated with chemical, the tumor will be shrunk, the tumor surface had necrosis and calcinosis, facilitating the surgery, avoiding the spread of malignant cells around. Simultaneously, after being treated with chemical, the shrunk tumor surface will accurately evaluate the tumor size to be removed, minimizing the limb section [2]. The radical ablation is performed after using pre-surgery chemicals, including surgery to remove the tumor and disengage the joint. Postoperative chemicals help avoid the local recurrence and prevent micro metastases. Pure chemical treatment that has a survival rate of more than 5 years is less than 20%. With the pure surgery, the survival rate of more than 5 years is less than 15%. The combination of chemicals and surgery helps the patient survival rate of over 5 years at about 65% [3].
Osteosarcoma is metastasized by blood. Patients often die from distant metastases in the lungs, local metastases following the marrow canal on the same bone. The ablation of the entire femur and replacing it with a metal femur are considered a surgery that kills the metastasis in cancer [4]. This surgery was first performed by the surgeon named Buchman in 1965 and it is considered the world’s first total femoral replacement surgery. Its biggest advantage is to remove the patient’s diseased femur while preserving his limb and early rehabilitation mobilization. However, over 50 years of development, patients who were assigned to this surgery were very limited (mainly patients with bone cancer and also responded to chemicals and radiation), the design of artificial femur instruments corresponding to the patient’s size is not many, the difficulty in resuscitation anesthesia and postoperative rehabilitation training after the surgery makes this surgery not be applied in many places, and there is very few research works on the treatment results of this method, mostly for the past 15 years, and the published research results have not been really consistent. Common complications of the coxa replacement surgery are blood loss, loose joints from soft parts, joint or soft parts infection, limb length deviation, broken joints, coxa and knee joint dislocation, etc.
Case Report
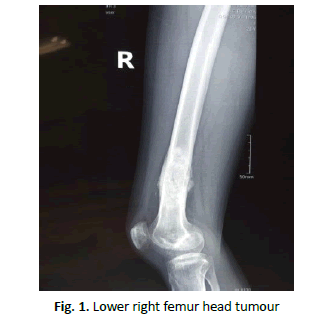
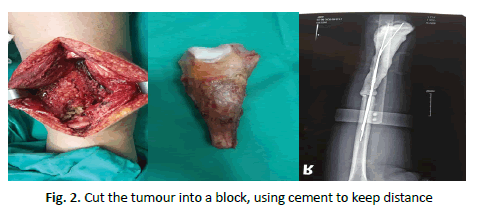
A 24-year-old female patient. Diagnosis: Osteosarcoma of the right lower femur (Fig. 1). She was treated with the preoperative chemicals with 3 phases, EOI regimen. The patient underwent surgery to cut broadly the first segment of the right lower femur, placing cement to maintain distance. Ensuring the safety of oncology and surgery according to the principle: The tumor was cut broadly into cubes; the removal area was larger than 3 cm from the tumor edge. The removal area was re-examined by an immediate biopsy and the bone marrow hadn’t malignant cells [5] (Fig. 2).
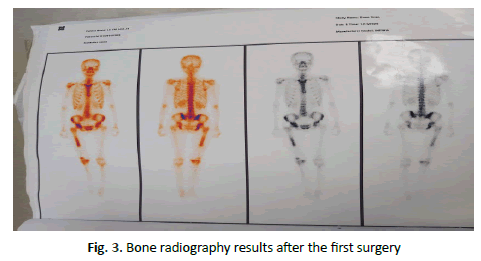
The anatomical results confirmed osteosarcoma, the tumor necrosis rate reached 20%. The patient changed the chemotherapy regimen after the IE5 surgery. After 6 phases of chemotherapy, the patient was fully evaluated before knee joint plastic surgery. Chest CT scanner did not show metastatic injury. Local CT and MRI did not show tumor recurrence signs. However, bone radiography showed an increase in radiation concentration in both the femoral section and the right femoral head region (Fig. 3). Further examination with coxa MRI showed no abnormalities, we decided to remove the entire femur and replace the artificial femur to ensure thorough oncology due to the injury suspicion to the coxa, simultaneously, the bone necrosis after pre-surgical chemotherapy had not met the requirements.
However, this patient’s limbs were immobilized due to the tumor ablation and cement replacing to maintain distance. The muscle and tendon system of the right leg after 3 months shrunk to 2 cm, shorter than the left leg. The knee joint folded 30 degrees. Therefore, to accommodate the patient’s condition, we designed the femur that was 2 cm shorter than the left leg.
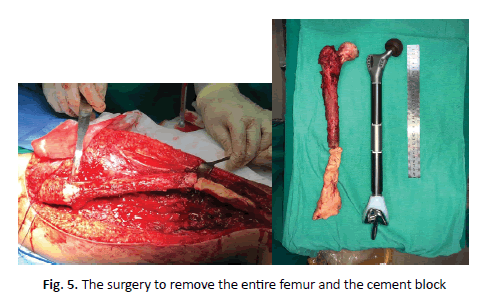
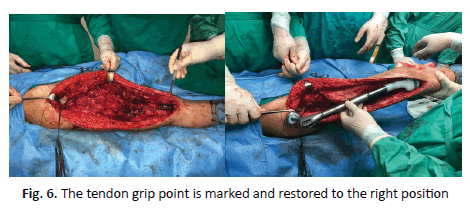
The 70 cm incision (Fig. 4) was selected along the outer surface of the thigh and continued to the old incision. Due to the tendon contraction and the incision outside, the surgery revealed the limited tibial plateau, the difficulty in forming the tibial plateau. During the surgery, all tendon grip points to the femur head are marked (Fig. 5 and 6). The entire femur was replaced in the correct anatomical position. The tendon grip points were restored. The whole operation took about 2:30 minutes.
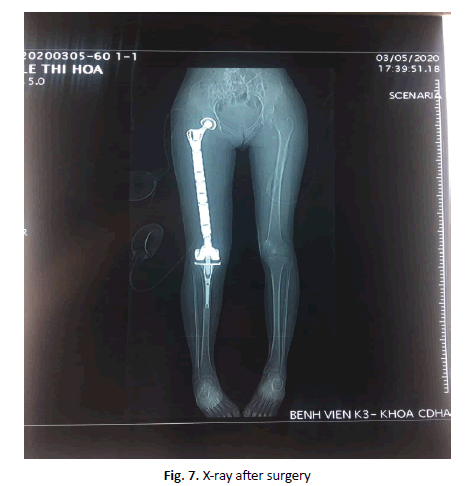
After the surgery, the patient had passive exercises on folding knees, groin movement, muscle contraction in bed, after 1 week of standing exercises. After 10 days, she could go with 2 crutches without pressure on the right leg. 1 month after the surgery, the results of the coxa and knee joint movement were good (Fig. 7). The patient was able to walk on crutches on his own, without pain (Fig. 8). The knee could fold 90 degrees. MSTS score reached 25/30 points. There were no signs of the tumor recurrence, no early complications such as infection, joints dislocation. After the surgery, the patient continued to receive chemotherapy according to IE5 regimen to complete the chemical process.
Discussion
The entire femur replacement surgery performed in 1952 by Buchman, reporting good results after 6 months [6]. However, since then, this is still a less common and complicated surgery, few medical centers in the world can perform it so there are not many reports. Most reports are in the clinical cases form, or in small numbers for many years [7]. The entire femur replacement surgery is indicated for patients with malignant bone tumors or replacement surgery for 2 of the patients who had other non-malignant disease. Toepfer compared the results of the entire femur replacement surgery replacement of 22 patients divided into 2 groups: cancer patients and non-cancer patients. The results were quite interesting when the average functional score of the cancer patients’ group was significantly higher with 19/30 points compared with 9/30 points for non-cancer patients. Some complications were soft parts complications (stiffness, dislocated joints), accounting for 59%, infections 22%, and joint instruments fracture 9% [8].
According to the original plan, our patients would be reshaped the knee joint with the hinge knee joint with metal module of the lower femur head form. However, during the pre-surgery re-evaluation, a new lesion was suspected in the femoral head, so we changed to replace the entire femur. Although the anatomical result of the femoral head injury after the surgery was an inflammatory lesion, not a cancer lesion, it was also a very important experience to help evaluate future cases. No standard incisions were recommended for the entire femur replacement surgery. Our chosen incision was Watson John’s incision, following the 70 cm patient’s old scar, through many blood vessels, large muscle tendons. This incision was favorable for the surgery of 1/3 on the femur. However, it was difficult to have surgery to release knee joints and tibial plateau. The patella did not turn over and had to be lifted, the patella tendon tension would limit the operation and, could damage the patella tendon.
The MSTS joint function score of the patients who were replaced with the entire femur in the previous studies reached from 65.5% to 80% [7,9,10]. The MSTS score in this study is 25/30 points (83%). One of the reasons we achieved such a functional score is that due to the primary cancer injury in the bone, the soft part is not invaded so the tendon and muscle system is intactly preserved, young patient, good preparation and psychological counseling process, close guidance for rehabilitation. Toepfer author [10] also said that the average function score of the cancer patients’ group was significantly higher with 19/30 points than the non-cancer patients’ group with 9/30 points [8]. Kakimoto author also suggested that the priority should be given to the entire femur replacement in the patients with primary cancer at the femur than in the patients group with soft part cancer that invaded the bone or metastases from other organs to the bone due to the overall survival prognosis and limbs function of the primary cancer group were better [10]. Moreover, Sewell suggested that when the second surgery is required, the MSTS score will be significantly reduced in comparison with the beginning [10,11].
The complications rate after the entire femur replacement surgery is still high. Andreas and his colleagues reported their experience of replacing the entire femur in 22 patients, 5 cases had deep infections requiring the re-surgical intervention (1 case due to the cancer, 4 infections cases due to femoral replacement surgery with other reasons) [8]. Kakimoto had one in nine patients with deep infections to be intervened again to avoid having to remove the coxa. The infection rate in previous studies ranged from 3 to 22% [7,12,13]. This was the first femur replacement surgery in Vietnam, we did not have much experience in this surgery. So, we divided the surgery into 2 periods. During the first period, we cut the lower segment of the femur and placed the cement to maintain distance. During the second period, we cut the upper segment of the femur and replaced the artificial femur. We think that the surgery time is shorter so the blood loss is low, not compensated, and concurrently the infection complication after the surgery reduces. Some other complications noted by the authors were soft part complications (stiffness, joint dislocation) in the study of 22 Toepfer patients accounting for 59%, joint instruments fracture 9% [8]. Ahmed noted that 1 case had loose tibial plateau hilt [7], and Kakimoto with 9 patients reported no loose joints case.
About the artificial femur, we used hinged knee joint system, at the coxa we restored tendon grip points at good positions. The tendon grip points were sewn and marked during the surgery, avoiding missed or dropped tendons. We fixedly sewed with super durable thread. However, joint grip points interconnected with artificial materials needed a long time. In the first 2 months, the patient walked with splint support, straight leg, practiced folding passive knee in the bed to avoid the early muscle contraction. After 2 months, she practiced active muscle contraction. Especially this patient immobilized for a long time, about 3 months, so the muscle and tendon system was shrunk, when she recuperated her health, grip points would be stretched. Early muscle contraction can cause pain or damage muscle and tendon, leading to loosen joints when moving later. Adel Refaat Ahmed replaced the entire femur for 9 patients from 1993-2007, resulting in 1 patient with loose knee joint [7]. In the report of Toepfer and his colleagues, there were 5 cases of loose coxa, 1 case of loose knee to have to be operated again with 22 cases of entire femur replacement [8]. However, for our patients whose upper femur head lesions did not invaded surrounding soft part, all muscle and tendon grip points were maximally preserved in length without defect and young patients. We anticipated that the rehabilitation might be better later. From the results of previous studies and this case, it can be drawn a conclusion that, when we want a maximum limbs rehabilitation, it is necessary to carefully evaluate the soft part damage before surgery and make appropriate surgery plan and rehabilitation method. Especially for cancer patients, it is necessary to evaluate invasive injury degree. When the injury spread, we have to remove a large soft part, it will cause functional deficiencies and severely affect the limbs mobility. Surgeons should always consider carefully between conservation and amputation design. Even with a full preoperative evaluation, the failure risk with this surgery is still very high.
Conclusion
The entire femur replacement surgery for bone cancer treatment is a major, rare and high complication surgery. To avoid the failure, it is necessary to carefully evaluate the soft part injury before surgery and have surgical, postoperative care and rehabilitation plan. The initial success of this surgery reflects the advances in science and technology of Vietnamese Medicine. However, whole treatment process is long, many happenings are complicated and there still are serious impacts on the patient life quality. Therefore, it is still necessary to continue researching and developing more effective and safer bone cancer treatment procedures in the future.
Compliance with Ethical Standards
Funding: this study does not receive funding from any organization.
Conflict of Interest
Authors have no conflict.
Ethical Approval
Ethical approval has been granted in this study.
Informed Consent
The consent and commitment were signed by the patient.
REFERENCES
- Fletcher C.D.M, Bridge J.A., Hogendoorn P.C.W., et al.: WHO classification of tumors of soft tissue and bone. Fourth Edition. WHO. 2020;5.
- Anderson M.E.: Update on survival in osteosarcoma. Orthop Clin North Am. 2016;47:283-292.
- Biermann J.S., Chow W., Adkins D.R., et al.: nccn guidelines index table of contents discussion. Bone Cancer. 2019;96.
- Malawer M.M., Wittig J.C., Bickels J., et al.: Operative techniques in orthopaedic surgical oncology. Lippincott Williams and Wilkins. 2015.
- Ernest U. Conrad.: Orthopeadic Oncology. 2010:117.
- Buchman J.: Total femur and knee joint replacement with a vitallium endoprosthesis. Bull Hosp Joint Dis. 1965;26:21-34.
- Ahmed A.R.: Total femur replacement. Arch Orthop Trauma Surg. 2010;130:171-176.
- Toepfer A., Harrasser N., Petzschner I., et al.: Is total femoral replacement for non-oncologic and oncologic indications a safe procedure in limb preservation surgery? A single center experience of 22 cases. Eur J Med Res. 2018;23:5.
- Reddy K.B.: Total femoral prosthesis in malignant bone tumours: a case series. CTOIJ. 2017;3:1-4.
- Kakimoto T., Matsumine A., Asanuma K. va cong su.: The clinical outcomes of total femur prosthesis in patients with musculoskeletal tumors. SICOT J. 5.
- Sewell M.D., Spiegelberg B.G.I., Hanna S.A., et al.: Total femoral endoprosthetic replacement following excision of bone tumours. J Bone Joint Surg Br. 2009;91:1513-1520.
- Kalra S., Abudu A., Murata H., et al.: Total femur replacement: primary procedure for treatment of malignant tumours of the femur. Eur J Surg Oncol. 2010;36:378-383.
- Puri A., Gulia A., va Chan W.H.: Functional and oncologic outcomes after excision of the total femur in primary bone tumors: Results with a low cost total femur prosthesis. Indian J Orthop. 2012;46;470-474.




 Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.
Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.