Results of anterior decompression and fusion in thoracic spinal tuberculosis patients presenting with advanced neurological deficit: A prospective mid-term follow-up study
Received: 13-Apr-2022, Manuscript No. JOTSRR-22-60609; Editor assigned: 16-Apr-2022, Pre QC No. JOTSRR-22-60609(PQ); Accepted Date: Apr 28, 2022 ; Reviewed: 18-Apr-2022 QC No. JOTSRR-22-60609(Q); Revised: 22-Apr-2022, Manuscript No. JOTSRR-22-60609(R); Published: 01-May-2022, DOI: DOI. 10.37532/1897- 2276.2022.17(1).72
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Introduction
Spinal tuberculosis is one of the most ancient diseases known to human race which has been reported from Egyptians mummies dating as far back as 3400 BC [1]. Only eight countries account for around two third of global burden of tuberculosis of which India (27%) constitute the maximum prevalence of cases [2]. In spite of initial success following advances in early diagnosis and improved management, tuberculosis continues to be a major health concern worldwide due to emergence of Multidrug Resistant (MDR) strains, resurgence of HIV infection and global migration phenomenon [3]. Around 10% of patients with extra-pulmonary tuberculosis have skeletal affection with spinal involvement seen in 50% of cases followed by the hip and the knee [4].
Neurological complication is the most dreaded consequence of tuberculosis of spine [5]. It is more commonly encountered in thoracic region because of narrow spinal canal diameter and can quickly progress to cause paraparesis or even paraplegia. Although neurological complications are best managed by prevention, surgical intervention is often required in advanced cases or in those who fail to respond to medical therapy [6].
Various surgical techniques have been described in literature to access the pathological lesion at different levels of vertebral column such as anterior approach, posterior approach, global reconstruction by posterior alone approach or combined procedures [7]. The anterior approach is regarded as the gold standard for debridement and decompression of tuberculosis of spine [8]. In thoracic spinal affection this can be achieved by thoracotomy, extrapleural (antero-lateral) approach and posterior transpedicular approach [9]. The aim of the present study was to evaluate the results of transpleural anterior decompression and fusion with or without instrumentation in tuberculous paraplegic patients of thoracic spinal affection.
Method
STUDY DESIGN
Institutional Ethics Committee approval was sought and granted before commencement of the present study. Written informed consent was obtained from all patients before they were enrolled. A prospective trail was performed on all consecutive patients who fulfilled the inclusion criteria and were operated for tuberculous paraplegia following thoracic spinal affection at a tertiary care hospital in the state of Maharashtra, India, between the duration July 2016 and September 2019.
STUDY POPULATION
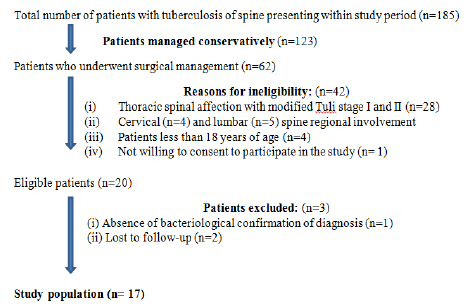
Out of the 187 patients who were admitted with a diagnosis of tuberculosis of spine, 17 patients were found to be eligible and thus included in the present study (Figure 1).
INCLUSION AND EXCLUSION CRITERIA
All patients above 18 years of age with tuberculosis of spine involving the thoracic region and presenting with modified Tuli SM classification system stage III to stage V neurological impairment who underwent surgical intervention by a single senior spine surgeon at a tertiary care referral centre were included in the present study [10]. Conversely, patients managed on medical therapy; operated for stage I and stage II neurological impairment; non availability of bacteriological confirmation of diagnosis; age <18years; unwilling to consent for participation or follow-up less than 6 months were excluded.
SAMPLE SIZE CALCULATION
A pre-hoc analysis was carried out based on a previous study reference using the formula mentioned below. In order to achieve 80% power, 5% level of significance and 9% margin of error, the required sample size was 15. Considering a non-response rate of 10% the final sample size was calculated to be 17.
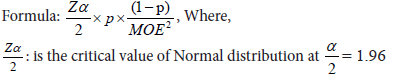
MOE: is the margin of error = 9% p: is the sample proportion = 5%
DATA COLLECTION AND MEASUREMENTS
All the data was electronically collected and stored in Microsoft Excel spreadsheet. Demographic and baseline characteristics such as age, gender, occupation and socio-economic status were recorded for all patients. A detailed history and through clinical examination including neurological assessment was performed. Neurological impairment was staged based on classification system suggested by Tuli SM et al and modified by Jain AK et al. This classification system was preferred as it not only stages all cases of paraplegia but also reflects the severity of cord compression by the addition of sensory and motor deficit scores.
Stage 1, Patient unaware of neural deficit, clinician detects plantar extensor and/or ankle clonus
Stage 2, Patient has spasticity with motor deficit but is a walker. Anticipated motor score in paraparesis is between 80 and 100. Sensory impairment involves the lateral column.
Stage 3, Bedridden spastic patient. Anticipated motor score for paraplegia is 50-80. Sensory impairment is same as in stage II
Stage 4, Bedridden patient with severe sensory loss, and/or pressure sores. Anticipated motor score in paraplegia is 50. Sensory impairment of both lateral and posterior column
Stage 5, Same as stage IV and/or bladder and bowel involvement, and flexor spasm/flaccid tetraplegia/paraplegia
Pre-operative patient preparation included routine laboratory investigations and anaesthetic fitness for all patients. Imaging modalities such as radiographs (antero-posterior and lateral views) and MRI scan were obtained to assess location and extension of tuberculosis lesion. Final diagnosis was confirmed based on histopathological and/or microbiological examination of biopsy samples obtained intra-operatively.
ANTI-TUBERCULAR CHEMOTHERAPY PROTOCOL
All eligible patients who underwent surgical intervention were started with extended course of anti-tubercular chemotherapy pre-operatively at the time of diagnosis consisting of 2 months of intensive phase including four drugs (isoniazide, rifampicin, pyrazinamide and ethambutol) followed by 10-16 months of continuation phase based on patients clinical outcome including three drugs (isonazide, rifampicin and ethambutol [11].
SURGICAL TECHNIQUE
Trans-pleural anterior spinal fusion was done in all patients. The patient was placedin right lateral position with sand bag below the chest at the level of the lesion.
Incision was made along the rib in the mid-axillary line opposite the point of maximum convexity of kyphosis. This was usually two ribs higher than the centre of vertebral lesion. To remove the 3rd, 4th and 5th rib, ‘J’ shaped Para scapular incision was taken. The scapula was lifted off the chest wall after dividing the scapula-thoracic muscles. To remove the 6th rib, a slightly curved incision passing around the inferior angle of the scapula was taken. The 7th, 8th and 9th ribs were removed by a straight oblique incision along the ribs.
The superficial muscles were cut in layers while the periosteum of the chosen rib was cut as far forwards and backwards as possible. The rib was removed and kept sterile for use as bone graft later. A small incision was made in the rib bed. A self-retaining retractor was applied to open the space by retracting the ribs. After retracting the lungs, the paravertebral abscess and aorta were visualised. A vertical incision was made in the groove between the aorta and abscess necessary to expose the diseased vertebra. Intercostal vessels were exposed and ligated in continuity. Aorta was displaced forwards and medially away from the spine and the abscess was palpated across the front of the vertebral body. The abscess was opened by ‘H’ shaped incision. The flaps were retracted by means of stay sutures and the lesion was visualized after draining all the pus and debris. All the granulation tissue, sequestra, caseous material and pus was removed carefully till fresh bleeding bone was exposed on both sides. Cord was decompressed carefully. Slots were made in the normal vertebrae above and below the lesion in the coronal plane at about the midline. The distance between the slots was measured with caliper. The bone graft from the iliac crest was cut to the required size and inserted, while the kyphosis was sprung open and the pressure was released. The abscess was closed after through irrigation of the abscess cavity. Intercostal drainage tube was kept in the pleural cavity and the incision was closed in layers.
POST-OPERATIVE PROTOCOL AND FOLLOW UP
All patients were treated with strict bed rest for 6 weeks post-surgery. Surgical drain was usually removed after 72 hours. Patients were followed up at 6 weeks, 3 months, 6 months, 1 year and at 2 years post-operatively. At each follow up detailed clinical and neurological assessment was performed. Parameters such as weight, ESR, peripheral blood smear and sputum examination were routinely measured. Radiographs and MRI scan were taken at 3 months followed by every 6 months to assess for graft fusion and healing of lesion. Follow up of cases was done till a maximum duration of 2 years.
STATISTICAL ANALYSIS
The data was recorded on case sheet and then entered into MS-Excel worksheet. Further analysis was carried out using IBM SPSS Statistics 27.0. The nominal variables were presented using frequency and percentage. Chi-square test for significance was used to test the significance of association between variables. Z-test for single proportion was used to compare the proportions. The level of significance was set at 5% and all p-values less than 0.05 were treated as significant.
Results
The distribution of demographic and clinical characteristics of patients (n=17) is as shown in table 1.
| Age (years) | Male | Female | Total (n=17) | |
|---|---|---|---|---|
| 18-24 | 1 | 1 | 3 | |
| 25-34 | 2 | 5 | 7 | |
| 35-44 | 1 | 1 | 1 | |
| 45-54 | 0 | 3 | 3 | |
| 55-64 | 1 | 1 | 2 | |
| ≥ 65 | 1 | 0 | 1 | |
| 6 | 11 | 17 | ||
| Z= -1.213, p=0.2253, Not significant | ||||
| Associated medical comorbidities, n=17(%) | ||||
| Diabetes | 3(17.64) | p>0.05, Not significant | ||
| Hypertension | 3(17.64) | |||
| Ischaemic heart disease | 1(5.88) | |||
| Hypercholesterolaemia | 1(5.88) | |||
| Staging of tuberculous paraplegia, n=17(%) | ||||
| III | 11(64.70) | Chi-square=7.882, p=0.019, Significant at 5% level | ||
| IV | 4(23.52) | |||
| V | 2(11.76) | |||
| Duration of neurological symptoms at presentation. n=17(%) | ||||
| ≤1 month | 7 (41.17) | Chi-square=9.765, p=0.045, Significant at 5% level | ||
| 1 to 3 months | 6 (35.29) | |||
| 3 to 6 months | 2 (11.76) | |||
| 6 to 12 months | 1(5.88) | |||
| ≥12 months | 1 (5.88) | |||
Highest incidence of patients was seen between 25-34 years age group in both sexes. Higher female preponderance comprising of about two third (64.70%) of all patients was observed. Majority of patients (52.93%) belonged to low socio-economic class comprising of labourers and farmers who were engaged in strenuous physical activity. Among the associated symptoms along with neurological impairment, backache was the most consistent symptom reported by all patients (100%) followed majorly by constitutional symptoms (49.50%) and spinal deformity (29.26%). In terms of pre-operative staging of neurological impairment, almost two third (64.70%) of patients belonged to stage III. Although wide variation was observed, majority (76.47%) of patients presented within 3 months of onset of neurological impairment. Pulmonary tuberculosis was the most common (11.10%) associated tuberculosis lesion. The laboratory and radiological imaging characteristic findings are illustrated in table 2.
Table 2: Laboratory findings and radiological characteristics of patients (n=17)
| Pre-operative haemoglobin level (gm%), n=17(%) | ||
|---|---|---|
| 6.0-8.0 | 1 | |
| 8.1-10.0 | 4 | |
| 10.1-12 | 8 | |
| 12.1-14 | 3 | |
| ≥ 14 | 1 | |
| ESR (mm/hr at end of first hour) | Pre-operative | Post-operative |
| ≤ 20 | 1 | 2 |
| 20-40 | 2 | 12 |
| 41-60 | 3 | 2 |
| 61-80 | 2 | 1 |
| 81-100 | 6 | 0 |
| ≥ 100 | 3 | 0 |
| p<0.001, Significant at 1% level | ||
| Number of vertebra involved, n=17 (%) | ||
| One | 5 (29.41) | |
| Two | 8 (47.05) | |
| More than two | 4 (23.52) | |
| p>0.05, Not significant | ||
High proportion of patients (35.29%) had pre-operative ESR values ranging between 81-100 (mm/hr). All patients showed uniformly regressing trend of their respective ESR values in the post-operative period. A high proportion of patients had involvement of ≥2 vertebrae (70.57%). Although 7 patients (41.17%) showed clinically apparent and radiologically confirmed evidence of cold abscess, 2 (11.76%) additional patients had cold abscess identified intraoperative.
Table 3 depicts the degree of neurological recovery compared to pre-operative severity and time duration taken for recovery.
Table 3: Assessment of neurological and radiological outcome, (n=17)
| Degree of neurological recovery at final follow-up, n=17 | ||||||||
|---|---|---|---|---|---|---|---|---|
| Pre-operative stage of neurological impairment | Complete | Partial | None | Total | ||||
| III | 11 | - | - | 11 | ||||
| IV | 3 | 1 | - | 4 | ||||
| V | 0 | 1 | 1 | 2 | ||||
| Time taken for optimal neurological recovery, n=17 | ||||||||
| Time to recovery | Complete | Partial | None | |||||
| 6 weeks | 9 | - | - | |||||
| 3 months | 4 | - | - | |||||
| 6 months | 1 | 1 | - | |||||
| 12 months | - | - | - | |||||
| 24 months | - | 1 | 1 | |||||
| Radiological healing of lesion (months), n=17 | ||||||||
| 01-Mar | 4 | |||||||
| 03-Jun | 6 | |||||||
| 06-Sep | 4 | |||||||
| 09-Dec | 3 | |||||||
Complete recovery was seen in most patients (n=14) by the end of 3 months. Two patients, one each of stage IV and V severity had no neurological improvement at final follow-up. More than half (58.82%) of patients showed radiological evidence of healing of lesion within first 6 months of post-operatively.
Discussion
In the present study, amongst the 17 patients operated for thoracic spinal tuberculosis with advanced neurological deficit who were evaluated, 14 patients (82.35%) achieved complete or near complete neurological recovery within 3 months, while 2 patients (11.76%) had partial recovery (ambulation with some support) and 1 patient (5.88%) failed to show any improvement at final follow-up. Our results are comparable to findings reported by Tuli SM et al. in his later series of tuberculous paraplegic patients analysed between year 1987 and 2000. In his series with more than 400 patients, 85% had complete recovery, 8% had partial recovery and negligible recovery was seen in 7% of patients [12]. Results of the present study are also in line with findings reported by other studies [13,14].
Development of neurological complications is most commonly seen in thoracic spine affection because of narrow spinal canal diameter in this region as well as physiological thoracic kyphosis which forces pathological lesion into the spinal canal. Incidence of neurological deficit in patients with spinal tuberculosis can vary widely from 23% to 76% [15]. Left untreated it can progress to paraplegia or tetraplegia.
Transpleural anterior spinal decompression and fusion was performed in all patients with additional instrumented stabilization in patients with loss of >2 vertebral body height (n=3, 17.64%). Anterior spinal fusion as popularized by Hodgson et al was favoured in the present study as it allows complete extirpation of the diseased focus via direct access to pathological site as well as placement of bone graft under compressive loads for reliable fusion [16,17]. Posterior spinal fusion on the other hand removes posterior healthy parts of the vertebrae leaving the spine unstable and also fails to directly address the pathological focus lying anteriorly. Intra-operative surgical findings in various combinations including granulation tissue (70.58%), cold abscess (52.94%), bony sequestra (58.82%) and disc sequestra (52.94%) encountered in our patients were comparable to findings reported in other studies [18,19].
High proportion (70.58%) of all patients in the present study had involvement of two or more vertebrae. Garg et al. has reported that affection of 2 or more vertebra is a predictor for poor outcome [20]. About three fourth (76.47%) of all patients presented within 3 months to the hospital after development of neurological impairment which was comparable with rates reported by Tuli. SM. et al in his series of 100 patients with neurological complications. High prevalence and awareness regarding tuberculosis in the study area may have prompted patients to seek medical treatment early. Early recovery in our study can be attributed to thorough and complete debridement of tuberculous lesion by radical anterior approach and sound bony fusion. The average duration of stay of patients in the hospital was 60 days with range varying from 30 to 90 days. While Hodgson et al reported average stay in hospital of 5 months and 14 days, Tuli SM et al observed a variation form 3 months to 9 months [21].
Inspite of higher female preponderance and majority of patients predominantly between 25 and 34 years age group, analysis of age and gender distribution revealed no statistically significant difference on final patient outcomes. These findings are in line with other study by Sharma et al [22]. Unlike gender, younger age however has been reported to carry favourable prognostic outcome [23]. Diabetes (17.64%) and hypertension (17.64%) was the most common associated medical comorbidity. Comparatively better surgical outcome in younger patients has been reported by other studies in the literature while elderly patients above 50 years are associated with poorer outcomes [24,25].
Although anti-tubercular chemotherapy has been the mainstay of treatment in both complicated and uncomplicated cases, surgical management is crucial for certain indications of spinal tuberculosis such as lack of adequate response to chemotherapy or recurrence, presence of severe neurological involvement at the time of presentation, static or even worsening of neurological symptoms even after initiating chemotherapy, severe debilitating pain, advanced deformity and instability [26-28]. All patients in our series underwent anterior spinal fusion through transpleural approach and reported good outcomes. Meta-analytic studies in recent literature claim that there is no significant difference in long term outcomes between anterior and posterior approaches as long as decompression of anteriorly based pathological lesion is addressed adequately. In addition, all-posterior instrumentation provides similar clinical outcome as compared to anterior [29,30].
No intra-operative complications were encountered with the surgical technique. Immediate post-operatively 1 patient developed broncho-pneumonia while 2 patients had superficial wound infection. Late post-operative complications such as sinus formation and bed sore were reported in 2 patients respectively. All complications resolved after adequate conservative management without the need for revision surgery.
Conclusion
From the present study we conclude that transpleural anterior decompression and fusion with or without instrumentation gives good neurological and functional outcomes in tuberculous paraplegic patients of thoracic spinal affection as it allows complete decompression with accurate visual assessment of extent of pathological focus.
REFERENCES
- Taylor G., et al.:"First report of Mycobacterium bovis DNA in human remains from the Iron Age." Microbiology. 2007; 153:1243-1249.
- Garg R.K., Malhotra H.S., Kumar N.:Spinal Tuberculosis: Still a Great Mimic. Neurol India. 2019;67:1402-1404
- McLain R.F., Isada C.:Spinal tuberculosis deserves a place on the radar screen. Cleve Clin J Med. 2004;71:537-539
- Gautam MP.:Pott’s spine and Pott’s paraplegia. J Nep Med Assoc. 2005;44:106-115
- Jain A.K.:Treatment of tuberculosis of the spine withneurologic complications in symposium on Osteo-articulartuberculosis. ClinOrthopRel Res. 2002;398:75-84
[Google Scholar] [Crossref]
- Shetty A., Kanna R.M., Rajasekaran S.:TB spine—Current aspects on clinical presentation, diagnosis, and management options. Semin Spine Surg. 2016;28:150.
- Rajasekaran S., et al.:Spinal Tuberculosis: Current Concepts. Global Spine J. 2018;8:96-108.
- Taylor G., et al.:"First report of Mycobacterium bovis DNA in human remains from the Iron Age." Microbiology. 2007; 153:1243-1249.
- Garg R.K., Malhotra H.S., Kumar N.:Spinal Tuberculosis: Still a Great Mimic. Neurol India. 2019;67:1402-1404
- McLain R.F., Isada C.:Spinal tuberculosis deserves a place on the radar screen. Cleve Clin J Med. 2004;71:537-539
- Gautam MP.:Pott’s spine and Pott’s paraplegia. J Nep Med Assoc. 2005;44:106-115
- Jain A.K.:Treatment of tuberculosis of the spine withneurologic complications in symposium on Osteo-articulartuberculosis. ClinOrthopRel Res. 2002;398:75-84
[Google Scholar] [Crossref]
- Shetty A., Kanna R.M., Rajasekaran S.:TB spine—Current aspects on clinical presentation, diagnosis, and management options. Semin Spine Surg. 2016;28:150.
- Rajasekaran S., et al.:Spinal Tuberculosis: Current Concepts. Global Spine J. 2018;8:96-108.
- Kotil K., Alan M.S., Bilge T.:Medical management of Pott disease in the thoracic and lumbar spine: a prospective clinical study. J Neurosurg Spine. 2007;6:222-228.
[Google Scholar][Crossref]
- Wang X., Li J., Lü G., et al.:Single-stage posterior instrumentation and anterior debridement for active tuberculosis of the thoracic and lumbar spine with kyphotic deformity. Int Orthop. 2012;36:373-380.
- Benli T., Kaya A., Acaroglu E.:Anterior instrumentation in tuberculous spondylitis: is it effective and safe?. Clin Orthop Relat Res. 2007;460:108-116. [Google Scholar] [Crossref]
- Tuli S.M.:Results of treatment of spinal tuberculosis by "middle-path" regime. J Bone Joint Surg Br. 1975;57:13-23.
- Goel M.K.:Treatment of Pott's paraplegia by operation. J Bone Joint Surg Br. 1967;49:674-681.
- Garg R.K., et al.:Evaluation of prognostic factors in medically treated patients of spinal tuberculosis. Rheumatol Int. 2013; 33:3009-3015.
- Hodgson A.R., et al.:A clinical study of 100 consecutive cases of Pott’s paraplegia. Clin. Orthop Relat Res. 1964;36:128-150.
[Google Scholar] [Crossref]
- Sharma A., et al.:Demographics of tuberculosis of spine and factors affecting neurological improvement in patients suffering from tuberculosis of spine: a retrospective analysis of 312 cases. Spinal Cord. 2017;55:59-63.
[Google Scholar] [Crossref ]
- Park D.W., et al.:Outcome and management of spinal tuberculosis according to the severity of disease: a retrospective study of 137adult patients at Korean teaching hospitals. Spine. 2007;32:130-135.
- Moon M.S., et al.:Pott’s paraplegia in patients with severely deformed dorsal or dorsolumbar spines: treatment and prognosis. Spinal Cord. 2003;41:164-171.
- Sai Kiran NA.:Surgical results in patients with tuberculosis of the spine and severe lower-extremity motor deficits: a retrospective study of 48 patients. J Neurosurg Spine. 2007;6:320-326.
- Rajasekaran S, Khandelwal G.:Drug therapy in spinal tuberculosis. Eur Spine J. 2013;22:587-593.
- Wilkinson MC.:Tuberculosis of the spine treated by chemotherapy and operative debridement. A long-term follow-up study. J Bone Joint Surg Am. 1969;51:1331-1342.
[Google Scholar] [Crossref]
- Zhang Z., et al.:The outcomes of chemotherapy only treatment on mild spinal tuberculosis. J Orthop Surg Res. 2016;11:49.
- Muheremu. A., et al.:Study on anterior and posterior approaches for spinal tuberculosis: a meta-analysis. Eur J Orthop Surg Traumatol 2014; 25: 69-76.
- Yang. P.,et al.:Clinical efficacy of posterior versus anterior instrumentation for the treatment of spinal tuberculosis in adults: a meta-analysis. J Orthop Surg Res 2014; 9: 10.
Abstract
Background: Advanced neurological complication following thoracic spinal tuberculosis can cause significant morbidity requiring surgical intervention. The aim of the present study was to evaluate the results of transpleural anterior decompression and fusion with or without instrumentation in tuberculous paraplegic patients of thoracic spinal affection.
Methods: A prospective study was conducted on all eligible patients with modified Tuli SM classification system stage III-V neurological impairment following thoracic spinal tuberculosis and who underwent transpleural anterior decompression and fusion at a tertiary care hospital between July 2016 and September 2019. The nominal variables were presented using frequency and percentage. Chi-square test for significance was used to test the significance of association between variables. Z-test for single proportion was used to compare the proportions. The level of significance was set at 5% and all p-values less than 0.05 were treated as significant.
Results: Seventeen patients met the inclusion criteria with highest incidence between 25-34 years age group in both sexes. Of all patients (n=17), 14 patients (82.35%) achieved complete or near complete neurological recovery within 3 months, while 2 patients (11.76%) had partial recovery (ambulation with some support) and 1 patient (5.88%) failed to show any improvement at final follow-up.
Conclusion: Surgical management involving transpleural anterior decompression and fusion with or without instrumentation gives good neurological and functional outcomes in tuberculous paraplegic patients of thoracic spinal affection as it allows through and complete decompression of pathological focus by directly addressing the pathological focus under vision.
Keywords
spine, tuberculosis, thoracic, paraplegia, decompression



 Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.
Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.