Results of orthopedic surgery in non-ambulatory adolescents with cerebral palsy complicated by hip dislocation
Received: 09-Jun-2017 Accepted Date: Jul 17, 2017 ; Published: 21-Jul-2017
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: The aim of the study was to evaluate efficiency of the Proximal Femoral Resection Arthroplasty (PFRA) and Subtrochanteric Valgus Osteotomy of the femur (SVO) associated with femoral head resection for pain control, improvement of postural management, hygiene and verticalization with total weight-bearing.
Methods: This retrospective study compared two groups of patients undergone the PFRA (10 cases, 17 hips) and SVO (27 patients, 40 hips). Patients presented level V of GMFCS (Gross Motor Function Classification System) in 13 cases, and level IV of GMFCS in 24 cases. The mean age was 14.1 ± 2.3.
Results: We did not observe any difference between the methods from the point of view of pain control, postural management, comfortable sitting position and hygiene. The verticalization with total weight-bearing was achieved only after SVO with femoral head resection associated with simultaneous knee and foot deformity correction performed with the principles of Single-Event Multilevel Orthopaedic Surgery (SEMLS).
Conclusion: Both methods allow to control pain syndrome, to achieve satisfactory postural management, comfortable sitting position, and hygiene. But only SVO with simultaneous knee and foot deformity correction provides supported standing with weight-bearing providing mechanical loading.
Keywords
Proximal femoral resection arthroplasty, Knee, Foot, Orthopaedic surgery
Introduction
Hip dislocation in patients with cerebral palsy is common especially in the most severe mentally challenged and non-ambulatory individuals. The incidence of hip subluxation or dislocation in patients classified as level III, IV and V by the Gross Motor Function Classification System (GMFCS) varies from 33% to 75% [1-3].
Hip dislocation in spastic quadriplegic patients is often associated with severe pain syndrome, difficulties with sitting position, sleeping, decubitus ulcerations, perineal hygiene [4-6]. The incidence of severe pain varies from 50% to 75% [3,5,7]. Pain related to hip dislocation is considered the main factor impairing the quality of life in quadriplegic spastic young adults [8].
The young patients benefit from reconstructive surgery [7,9]. On the other hand, if the hip cannot be reduced due to cartilage degeneration, femoral head and acetabulum deformities, in the adolescent or adult salvage procedures are able to provide pain relief and functional improvement [1,10-13]. Different approaches are proposed and used for palliative surgery in CP tetraplegic adolescents and adults: Proximal Femoral Resection Arthroplasty (PFRA) [1,11], Subtrochanteric Valgus Osteotomy (SVO) [10,14,15], proximal femur prosthetic interposition arthroplasty [7,12,16], hip arthrodesis [7,13]. These procedures aim to obtain a pain-free hip with sufficient passive range of motion, comfortable upright sitting position and improved perineal hygiene. On the other hand, CP patients with dislocated painful hip very often have severe flexion contracture of knee joints and foot deformities impairing use of shoes [17,18]. Furthermore, the passive verticalization is considered important to prevent severe osteoporosis and to maintain favorable conditions for function of visceral organs and to ameliorate socialization of patients [19,20]. From this point of view, the surgical procedure for hip dislocation problem should be simultaneously performed with correction of knee and foot deformities.
The purpose of our retrospective study was to evaluate the results of PFRA and SVO performed with simultaneous correction of knee and foot deformities by assessing treatment outcomes, especially regarding the degree of pain relief, improvement of sitting ability, perineal care, ability to passive verticalization.
Patients and Methods
We reviewed non-ambulatory patients treated in our institution between 2012 and 2015 for chronic painful hip subluxation or dislocation. The patients were included in this study if they had a diagnosis of cerebral palsy, had undergone palliative hip surgery associated or not with simultaneous corrections of knee and foot deformities, and had, at least, 12 months of follow-up. Criteria for operation were dislocation of the hip, and severe problems such as pain, sitting problems, difficulties with perineal care, severe flexion contracture of the knee joint and foot deformity correction, loss of ability for passive verticalization.
In post-operative period, patients were reviewed every three months for the first year and then one time every 12 months. The pain level was evaluated using the Wong-Baker FACES® Pain Rating Scale [21]. The level 3-4 (“hurts a little more”) was considered as critical. Duration of comfortable upright sitting position (sitting tolerance), ability for passive verticalization in a stander with weight-bearing and problems with perineal care were noted as well. Anteroposterior radiographs of pelvis were taken before surgery, on the day of surgery, and compared with those taken at the latest follow-up examination – to assess proximal femoral migration, heterotopic bone formation [4], bone consolidation and position of implants.
Statistical Analysis
Statistics was analyzed by means of the Attestat software (Attestation Software, Las Vegas, NV, USA). For the descriptive statistics, mean values of criteria and their standard deviation were defined.
This study was reviewed and approved by the Ethics Committee of our Institution.
Operative Technique
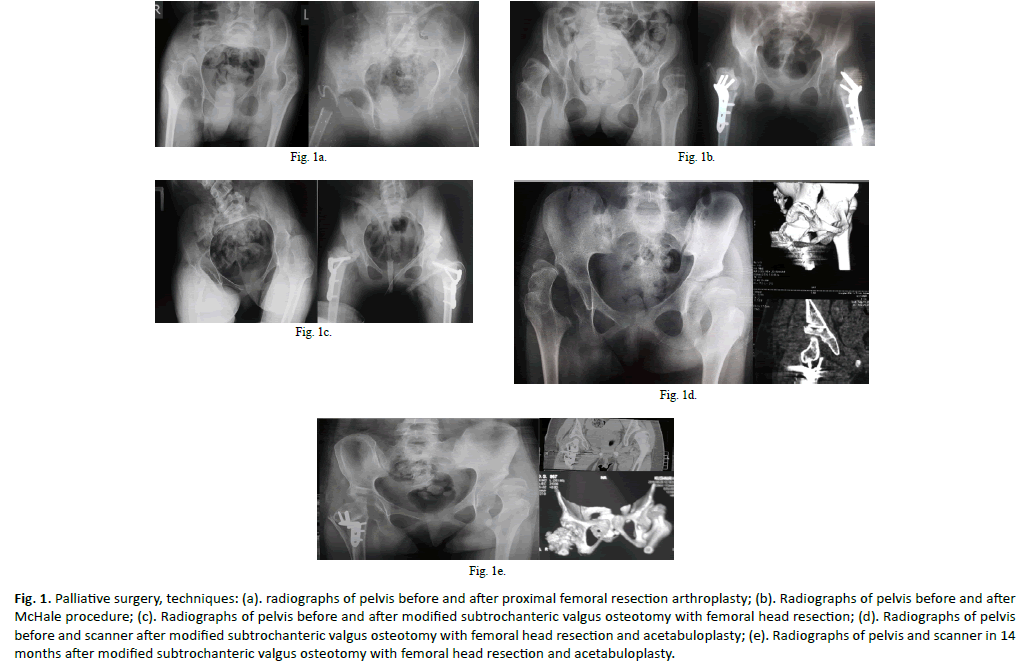
In this series of patients three surgical techniques were used: PFRA [1], SVO (McHale procedure) with femoral head resection [10] and our modification of SVO with femoral resection (Figure. 1).
Figure 1: Palliative surgery, techniques: (a). radiographs of pelvis before and after proximal femoral resection arthroplasty; (b). Radiographs of pelvis before and after McHale procedure; (c). Radiographs of pelvis before and after modified subtrochanteric valgus osteotomy with femoral head resection; (d). Radiographs of pelvis before and scanner after modified subtrochanteric valgus osteotomy with femoral head resection and acetabuloplasty; (e). Radiographs of pelvis and scanner in 14 months after modified subtrochanteric valgus osteotomy with femoral head resection and acetabuloplasty.
The Watson-Jones approach was used for the proximal femoral resection arthroplasty. Interposition technique involved suturing the iliopsoas and gluteal muscles to the hip capsule and covering the femoral shaft stump by suturing the vastus lateralis to the muscles and soft-tissues on the medial side. Post-operatively, patients had long leg cast with antirotating device for 3 to 6 weeks or external monolateral fixator in 2 cases for 2 weeks followed with orthosis. The PFRA finds its indications in patients of the level V of the GMFCS and if the further verticalization with weight-bearing cannot be expected.
In SVO procedure, the hip was exposed through Watson-Jones approach as well. In order to increase passive ROM, especially, external and internal rotation and flexion, we enlarged the valgisation wedge of bone so as to place the lesser trochanter at the level superior to greater trochanter when the Milch post-osteotomy angle [22] is inferior to 90°. That closing wedge osteotomy implies to achieve an angulation between bone fragments over 75° (modified SVO). In 5 patients, a reconstruction of oblique and shallow acetabulum was necessary to ameliorate the abutment of the lesser trochanter against to the acetabulum. An acetabuloplastylike osteotomy was performed with interposition of bone graft of femoral wedge osteotomy. The position of the lesser trochanter into acetabulum was stabilized by capsulorrhaphy with advanced limbs of the “T” and its attachment to the periosteum and vastus lateralis proximal insertion on the intertrochanteric zone. Preserved adductors longus and brevis contribute the appropriate position of the lesser trochanter into acetabulum. Patients had long leg cast with antirotating device and abduction pillow for 4 to 6 weeks. We used the SVO in patients classified as level IV and V by the GMFCS, if further passive verticalization with weight-bearing was expected and included in rehabilitation program.
There were not any features of surgical technique of femoral distal extension osteotomy, patella advancement, hamstring lengthening, triple foot arthrodesis, talonavicular arthrodesis, I metatarsal phalangeal joint fusion, bunion correction and triceps lengthening [17,18].
No routine heterotopic ossification prophylaxis was used postoperatively in all patients. The patients undergone SVO were authorized to standing with total weight-bearing by the 3rd postoperative week due to a locked mode of osteosynthesis.
Results
We retrospectively analyzed 42 medical charts of patients with CP complicated with hip subluxation or dislocation and hospitalized for orthopedic surgery. Only 37 patients (57 hips) corresponded to inclusion criteria and were involved into the study.
The average follow-up was 19.3 months (range 12-49 months). The average age at the time of surgery was 14.1 ± 2.31 years (range 10-18 years). The patients undergone PFRA procedure were all classified as level V of the GMFCS. There were 3 patients of level V and 24 patients of level IV of the GMFCS in the group of SVO.
Moderate (30° to 80°) flexion contracture of the knee was observed in 19 patients, in these patients the sitting ability was not deteriorated due to knee contracture but standing was impossible. In 9 cases, we observed severe flexion contracture of the knee (more than 90°) which caused additional difficulties for sitting position. Foot deformities with shoe wear problem were observed in 19 patients. There were hallux valgus and bunions associated with degenerative changes in the first metatarsophalangeal joint in 17 cases.
In total, 57 surgeries were performed. In 20 patients, limb surgeries were performed consecutively within four to ten weeks; and in 17 cases the operation was unilateral. Within the 57 surgeries, 222 particular surgical procedures were carried out at an average of 3.89 per surgery (Table 1) according to the principles of singleevent multilevel orthopedic surgery.
| Procedures | Group PFRA | Group SVO |
|---|---|---|
| PFRA | 17 | - |
| SVO (McHale procedure) | - | 7 |
| Modified SVO | - | 33 |
| Acetabuloplasty | - | 7 |
| Femoral distal extension osteotomy (partial extension of the tibia achieved) | 11 | - |
| Femoral distal extension osteotomy (full of the tibia extension) | - | 24 |
| Tenotomy of the tibialis anterior | 6 | - |
| Triple arthrodesis | - | 12 |
| Talonavicular arthrodesis | 7 | - |
| Hamstring lengthening | 10 | 43 |
| Triceps lengthening | 6 | 4 |
| Gastrocnemius lengthening | - | 14 |
| Great toe metatarsophalangeal joint arthrodesis | 4 | 17 |
Table 1: Surgical procedures.
Average estimated blood loss for the all series was 157.2 ± 37.5 ml. There were no significant differences in estimated blood loss between groups (Table 2). However, the transfusion was done in 6 cases of PFRA, and in 16 cases in SVO group.
| Before surgery | In 24 h | In 48 h | ||||
|---|---|---|---|---|---|---|
| PFRA group | SVOgroup | PFRA group | SVO group | PFRA group | SVO group | |
| Number of erythrocytes (×106/ml) | 5.2 ± 0.6 (4.22 – 6.12) |
4.7 ± 0.3 (4.25 – 5.22) |
4.0 ± 0.7 (2.68-5.06) |
3.6 ± 0.6 (2.44-4.96) |
4.1 ± 0.6 (3.33-4.97) |
3.8 ± 0.6 (2.73-5.19) |
| Hemoglobin (g/l) | 138.0 ± 13.9 (112-161) |
134.1 ± 11.5 (115-158) |
107.6 ± 19.8 (75-132) |
101.5 ± 20.2 (68-129) |
107.4 ± 10.4 (98-124) |
109.0 ± 17.4 (85-138) |
Table 2: Indices of hematogram.
Preoperatively, all patients had experienced severe pain and needed daily pain medication. Post-operatively, in PFRA group we observed progressive decrease of pain syndrome until 1 to 3 in 8 cases by the 3rd-6th month after surgery. Two patients of this group had not any change of pain syndrome because of diffuse heterotopic bone formation (1 case) or technical error (capsular and muscular soft-tissue interposition was not done). In SVO group the pain syndrome was decreasing (1 to 4) in 24 patients during 3 to 6 months postoperatively. In three cases, the initial hip pain level remained the same due to heterotopic ossification (1 case) or conflict between acetabulum and hardware (2 cases). The occurrence of pain syndrome of the level 3-4 or higher in three situations: in the most comfortable spontaneous position, at every-day standard activity, during rehabilitation sessions is summarized in Table 3. The both procedures were efficient to decrease pain syndrome and results are good and excellent in 90% in PFRA group and 92.5% in SVO group at the latest follow-up control. All the cases of persisting hip pain were related to heterotopic ossifications. The pain caused due to mechanical hardware conflict was resolved by material removal.
| Group | Positions | Before surgery | In 6 months after surgery | In 12-18 months after surgery |
|---|---|---|---|---|
| PFRA | The most comfortable position | 4/10 | 2/10 | 0/10 |
| Every-day standard activity | 10/10 | 4/10 | 1/10 | |
| Rehabilitation sessions | 10/10 | 4/10 | 1/10 | |
| SVO | The most comfortable position | 22/27 | 6/27 | 1/27 |
| Every-day standard activity | 27/27 | 12/27 | 2/27 | |
| Rehabilitation sessions | 27/27 | 14/27 | 2/27 |
Table 3: Number of patients having pain syndrome 3 and more in different situations.
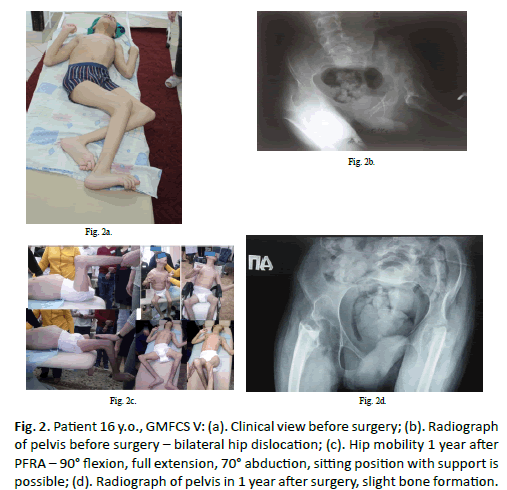
At the latest follow-up point the passive hip flexion in PFRA group was 90° to 120° in 12 hips (Figure. 2), 70° to 85° in 3 hips, the extension was full or with deficiency inferior to 10° in all these patients. We observed satisfactory ROM of abduction in 15 hips: 30° to 70°. Only in one case heterotopic ossification has limited ROM 60° to 90° flexion, and 0° to 10° of abduction (right side) and -20° to 0° of abduction (left side). The passive ROM was improved in 11 knee joints operated with distal femoral extension osteotomy: deficiency of extension from 30° to 60° with flexion from 90° to 110° as outcomes.
Figure 2: Patient 16 y.o., GMFCS V: (a). Clinical view before surgery; (b). Radiograph of pelvis before surgery – bilateral hip dislocation; (c). Hip mobility 1 year after PFRA – 90° flexion, full extension, 70° abduction, sitting position with support is possible; (d). Radiograph of pelvis in 1 year after surgery, slight bone formation.
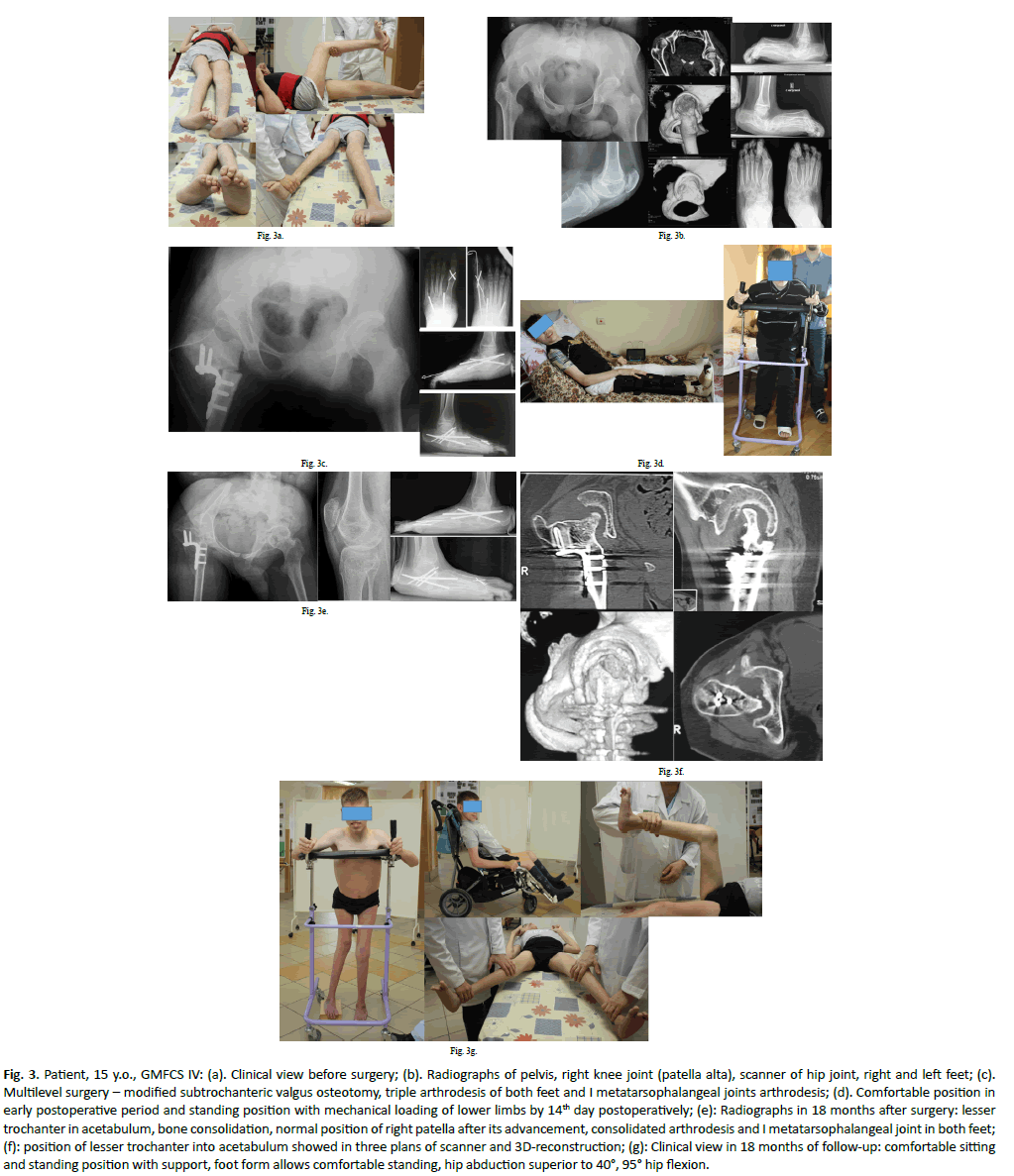
At final exam in the SVO group, the passive hip flexion was measured from 90° to 110° in 29 hips (Figure. 3), 60° to 85° in 10 hips, the extension was not full in 19 hips (deficiency from 10° to 25°). We observed satisfactory ROM of abduction in 30 hips: 30° to 60°. In all 7 cases after McHale procedure and only in 2 cases after modified SVO the maximal passive abduction of 20°-30° was achieved. The passive full knee extension was obtained in all 24 cases operated with distal femoral osteotomy. Only in 4 patients we observed limited knee extension (in average 12°) but supported standing with weight-bearing remained possible. Table 4 summarizes abilities for sitting, passive verticalization, and perineal hygiene.
Figure 3: Patient, 15 y.o., GMFCS IV: (a). Clinical view before surgery; (b). Radiographs of pelvis, right knee joint (patella alta), scanner of hip joint, right and left feet; (c). Multilevel surgery – modified subtrochanteric valgus osteotomy, triple arthrodesis of both feet and I metatarsophalangeal joints arthrodesis; (d). Comfortable position in early postoperative period and standing position with mechanical loading of lower limbs by 14th day postoperatively; (e): Radiographs in 18 months after surgery: lesser trochanter in acetabulum, bone consolidation, normal position of right patella after its advancement, consolidated arthrodesis and I metatarsophalangeal joint in both feet; (f): position of lesser trochanter into acetabulum showed in three plans of scanner and 3D-reconstruction; (g): Clinical view in 18 months of follow-up: comfortable sitting and standing position with support, foot form allows comfortable standing, hip abduction superior to 40°, 95° hip flexion.
| Positions | PFRA | SVO |
|---|---|---|
| There is no comfortable sitting position, sitting ability is limited to less than 30 min. wheelchair modifications would not improve it | 1/10 | 1/27 |
| Comfortable sitting position tolerated 1 to 2 hours | 3/10 | 14/27 |
| Sitting position tolerated without time limitation. including traveling | 6/10 | 12/27 |
| Standing position with weight-bearing 1 hour and more per day is possible | 0/10 | 25/27 |
| Satisfaction with perineal care (improvement since surgery) | 9/10 | 26/27 |
Table 4: Outcomes of PFRA and SVO procedures based on sitting tolerance, possibility of passive verticalization and satisfaction with perineal care (number of patients/total of patients).
Correction of foot deformities allowed to improve shoe wear in both groups and to have appropriate mechanical loading in patients of SVO group.
In total, we observed favorable outcomes of both procedures. Only one patient in each group was considered without improvement. The sitting position tolerance was slightly superior in patients undergone PFRA, but a standing posture has been achieved only after SVO procedure.
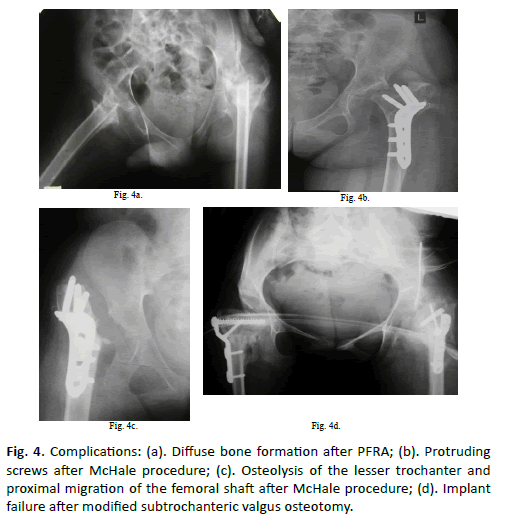
The mean proximal femoral migration at the last follow-up was 2.8 cm in the PFRA group, but only in one case it had clinical significance: direct contact between femur and acetabulum due to inappropriate surgical technique. We observed one case of diffuse ossification (type III) after PFRA procedure (Figure. 4) leading to pain syndrome and limitation of ROM. The patients of PFRA group had other complications: delayed wound-healing (1 case), prolonged pain lasting over 6 months (1 case) required a secondary surgery (Castle procedure), external wire migration of foot arthrodesis (1 case) required its removal, femoral fracture occurred without trauma (3 cases) when conservative treatment was applied. In the SVO group complications included (Figure. 4): excessive bone formation due to implant failure and secondary displacement associated with prolonged pain and limitation of ROM, mechanical conflict between screws and pelvis with pain during passive mobilization (3 cases) required hardware removal in 5 to 6 months after surgery, aseptic osteolysis of lesser trochanter, proximal femoral migration and excessive external rotation of the leg. Hardware removal with derotation osteotomy in 7 months after initial surgery was necessary for the last complication but the standing position with weightbearing has been failed. There was no delayed bone consolidation in patients underwent SVO. For all series, we observed three cases of superficial decubitus eliminated with local treatment.
Discussion
The palliative procedures are indicated for treatment of unreconstructable subluxated or dislocated hip in patients with CP in GMFCS levels IV-V [1,2,5-7,10,13]. Palliative procedures aim to provide the pain relief, function improvement and amelioration of quality of life [5,6,11,12,14]. Proximal Femoral Resection Arthroplasty [1,11] and Subtrochanteric Valgus Osteotomy [10,14,15] are the most appropriate and accepted procedures. Lots of colleagues don’t support use of hip arthrodesis or total hip arthroplasty in non-ambulatory CP patients because of mediocre functional outcome and higher rate of complications of these procedures [4-7,11,13,15].
On the other hand, the lack of weight bearing and biomechanical loading is a part of everyday routine of patients with cerebral palsy in GMFCS levels IV-V and increases risk of fractures related to osteopenia [23]. Mechanical loading is important for improving bone strength. The regular daily use of standing devices in patients who are unable to stand alone provides a fourfold reduction of fractures without trauma and should be advocated [19]. The hip palliative surgery should be able to provide standing position with weight bearing and be simultaneously performed with lower limb deformity and contracture correction. This approach corresponds to principles of single-event multilevel orthopedic surgery [24,25].
The proximal femoral resection arthroplasty described by Castle et al. [1] is indicated in non-ambulatory quadriplegic CP patients with chronic painful hip dislocation associated with impaired sitting ability and perineal care [2,4,11]. In literature, the mean age of patients undergone this salvage procedure varies from 14 years 4 months to 26.6 years [4,11,26-28]. In our study, PFRA was performed at the age of 15.7 ± 1.7 years old that is similar to series of Abu-Rajab et al. [26].
The postoperative results obtained with this technique were satisfactory regarding pain relief in 90% to 100% of cases [4,26,27]. The increased hip mobility allowed to obtain improvement in perineal care in 62-100% of cases [4,11,26]. In long term followup, more comfortable sitting position with support for longer pain-free intervals than before surgery was noted in all the studies [4,11,16,26-28]. The use of proximal femur prosthetic interposition may be an option close to principles of PFRA procedure [7,12,13]. But the reoperation rate seems to be higher [12].
In our study, the pain relief was obtained in 9 of 10 patients undergone PFRA in long term follow-up. This decrease of hip pain was associated with good tolerance of sitting position and satisfaction with perineal care in 9 cases (90%). Simultaneous correction of severe flexion knee contracture and foot deformities allowed to increase the quality of life for these patients regarding comfortable sitting position and shoewearing. But in the literature the approach of palliative hip surgery and simultaneous knee and foot orthopaedic procedures is not mentioned.
Subtrochanteric Valgus Osteotomy with or without resection of femoral head is also an option of palliative procedure and results in improvement of hip function and allows better perineal care [10,13-15]. This procedure appears to be less invasive and to have fewer complications, such as heterotopic ossifications and proximal migration of the femoral shaft, in comparison to PFRA [10,14,16]. The subtrochanteric valgus osteotomy provides complete pain relief in 60-92.7% of cases, and significant amelioration in the rest of patients [10,14,15,29]. Hip pain decrease was associated with improvement of sitting position with support and satisfaction with perineal hygiene in majority of series [10,15,16,29]. The hip abduction of 35°or more was achieved in 69.2% and hip flexion at least 90° was observed in 76.9% of patients [5,7,10,15,16].
In our series, we observed significant decrease or complete disappearance of hip pain in 92.6% of cases in every-day activity and rehabilitation sessions. Increased hip mobility and pain relief allowed improvement of passive sitting ability with support in 26 patients (96.3%). These outcomes are similar to results published in literature [5,7,10,15,16]. Our modified SVO procedure allowed an early verticalization with full weight-bearing in stander due to osteosynthesis with locked plates. In literature, mechanical loading of operated limb started in 6 to 8 weeks postoperatively if the bone fixation was performed with a regular plate [10,15,29]. Albiñana et al. described a high incidence of transfusion after SVO procedure – in 100% of cases [4]. Only after 16 surgeries (40%) the blood transfusion was obligatory in our study. The incidence of complications in palliative hip surgeries in patients with CP varies from 1.8% to 62.5% [3,6,11,14,16,26,27]. Comparison of PFRA with SVO from the point of view of complications is contradictory. Hwang et al. [6] had overall 32.4% complication rate in a series of 37 PFRA and emphasized an advantage of arthroplastic resection in comparison to SVO. Leet et al. [29] note significantly fewer cases of proximal femur migration and related pain syndrome as well as other surgical complications in patients undergone the McHale procedure. Wright et al. [16] don’t find any difference between procedures. We noted 6 complications after PFRA surgeries (41.2%) and 6 complications following valgus osteotomy (15%) but with similar reoperation rate. Severe grade of the heterotopic para-articular ossification is often observed after PFRA [4,26,27,30]. In literature, we found only one case of excessive heterotopic ossifications appeared after McHale procedure [15]. In our patients, there was 1 case of diffuse ossification after PFRA which deteriorated ROM and led to severe pain.
Hogan et al. [30], Van Riet et al. [15] reported a high incidence of secondary displacement related to use of non-locking plates in osteoporotic bones in McHale procedure. Mechanical conflict between protruding screws and pelvic bone that causes pain is a specific complication of SVO procedure [15]. We observed this problem only if the plates with proximal screws oriented toward acetabulum were used. Horizontal (perpendicular to plate) position of the proximal screw excluded this conflict in all cases in our series. There is only one case of proximal femoral migration mentioned in the available literature [15]. We had a case of lesser trochanter osteolysis observed in 6 months after McHale procedure followed with proximal femoral migration.
Other complications mentioned in the published series were: fibrous hip ankylosis of the hip after SVO because of prolonged immobilization [15], deep vein thrombosis, upper gastrointestinal bleeding in immediate postoperative period [11], two patients died by 4th and 11th postoperative day [11]. We did not observe these kinds of complications in our series.
In few studies comparing hip salvage surgeries comparative studies improvement of pain relief, comfortable sitting and perineal hygiene occurred following both types of surgery without significant differences between the groups [6,29]. In our series, a favorable outcome observed in 90% in the PFRA group and in 96,3% in the SVO group. But Leet et al. [29] found that for patients who underwent SVO duration of hospitalization was shorter and rate of complications was lower. Furthermore, Kolman et al. [13] emphasized, most of complications of SVO are implant related and should be amenable to plate and screws removal versus complications of PFRA which are related to procedure itself. In our study, there four cases of complications related to implant. Three of them were eliminated after hardware removal.
In our study, the SVO was not more aggressive and traumatic than PFRA. The both procedures provided an expected outcome in more than 90% of patients. We consider that verticalization in a stander with mechanical loading of lower limbs is one of goals of orthopaedic surgery. Thus, the hip palliative surgery should provide pelvic support and be associated with correction of knee flexion contracture and foot deformities. In that complex procedure, uniting palliative and reconstructive surgeries, we should respect principles of Single-Event Multi Level Orthopaedic Surgery such as multilevel correction of deformities, less aggressive technique, less bleeding, implant appropriate for osteosynthesis of osteoporotic bones etc. [24,25].
Weight bearing during supported standing has favorable impact on bone mineral density, cardiopulmonary and bowel/bladder function, and psychological status [8,19,20,23]. In our series, the early mechanical loading of lower limbs in standers was able because of locked plates application. This approach allowed to avoid a secondary displacement of bone fragments except one case. In the late postoperative period, not a single patient undergone SVO had a fracture. Whereas, we noted three fractures of the femur in patients undergone PFRA, who did not support standing position. So, we presume the supported standing with weight-bearing as one of the aims of orthopedic surgery in non-ambulatory CP patients of levels IV-V of the GMFCS.
In our opinion, the PFRA finds its indications in selected patients of level V of the GMFCS only if the further supported standing cannot be expected for some reasons. But severe knee flexion contractures and foot deformities should be corrected in order to improve supported sitting comfort, shoe wearing, to prevent skin breakdown and to maintain the better quality of life.
Conclusion
The surgery in non-ambulatory adolescents and adults with cerebral palsy having painful chronic subluxation or dislocated unreconstructible hip should aim to obtain a pain-free hip with sufficient passive ROM, comfortable upright sitting position, improved possibility for perineal hygiene and ability for supported standing with mechanical loading of lower limbs.
The PFRA as well as the SVO allows to obtain the first three objectives. But only the subtrochanteric valgus proximal femoral osteotomy, especially in modified technique, provides the verticalization of patients with mechanical loading of lower limb and only on condition if knee contractures and foot deformities are simultaneously corrected. Appropriate surgical technique and implants, combination of palliative and reconstructive procedures allow to resolve orthopaedic problems in these patients using single-event multilevel surgery.
REFERENCES
- Castle M.E., Schneider C.: Proximal femoral resection-interposition arthroplasty. J Bone Joint Surg Am. 1978; 60(8): 1051-1054.
- Ackerly S., Vitztum C., Rockley B., et al. Proximal femoral resection for subluxation or dislocation of the hip in spastic quadriplegia. Dev Med Child Neurol. 2003; 45(7): 436-440.
- Jóźwiak M., Walczak M., Idzior M.: Appearance of spastic hip pain in cerebral palsy children. Chir Narzadow Ruchu Pol. 2005; 70(2): 101-104.
- Albiñana J., Gonzalez-Moran G.: Painful spastic hip dislocation: proximal femoral resection. Iowa Orthop J. 2002; 22: 61-65.
- DeSouza R.C., Mansano M.V., Bovo M., et al.: Hip salvage surgery in cerebral palsy cases: a systematic review. Rev Bras Ortop. 2015; 50(3): 254-259
- Hwang J.H., Varte L., Kim H.W., et al.: Salvage procedures for the painful chronically dislocated hip in cerebral palsy. Bone Joint J. 2016; 98-B(1): 137-143.
- Root L.: Surgical treatment for hip pain in the adult cerebral palsy patient. Dev Med Child Neurol. 2009; 51 Suppl 4: 84-91.
- Krebs A., Strobl W.M., Grill F.: Neurogenic hip dislocation in cerebral palsy: quality of life and results after hip reconstruction. J Child Orthop. 2008; 2(2): 125-131.
- Reidy K., Heidt C., Dierauer S., et al.: A balanced approach for stable hips in children with cerebral palsy: a combination of moderate VDRO and pelvic osteotomy. J Child Orthop. 2016; 10(4): 281-288.
- McHale K.A., Bagg M., Nason S.S.: Treatment of the chronically dislocated hip in adolescents with cerebral palsy with femoral head resection and sub-trochanteric valgus osteotomy. J Pediatr Orthop. 1990; 10(4): 504-509.
- Knaus A., Terjesen T.: Proximal femoral resection arthroplasty for patients with cerebral palsy and dislocated hips: 20 patients followed for 1-6 years. Acta Orthop. 2009; 80(1): 32-36.
- Silverio A.L., Nguyen S.V., Schlechter J.A., et al.: Proximal femur prosthetic interposition arthroplasty for painful dislocated hips in children with cerebral palsy. J Child Orthop. 2016; 10(6): 657-664.
- Kolman S.E., Ruzbarsky J.J., Spiegel D.A., et al.: Salvage options in the cerebral palsy hip: A systematic review. J Pediatr Orthop. 2016; 36(6): 645-650.
- Schejbalova A., Havlas V., Trc T.: Irreducible dislocation of the hip in cerebral palsy patients treated by Schanz proximal femoral valgus osteotomy. Int Orthop. 2009; 33(6): 1713-1717.
- Van Riet A., Moens P.: The McHale procedure in the treatment of the painful chronically dislocated hip in adolescents and adults with cerebral palsy. Acta Orthop Belg. 2009; 75(2): 181-188.
- Wright P.B., Ruder J., Birnbaum M.A., et al.: Outcomes after salvage procedures for the painful dislocated hip in cerebral palsy. J Pediatr Orthop. 2013; 33(5): 505-510.
- Kolodziej L., Dobiecki K., Sadlik B.: Surgical treatment of advanced, stiff neurologic cavovarus foot in adults. Ortop Traumatol Rehabil. 2013; 15(4): 325-333.
- Bozinovski Z., Popovski N.: Operative treatment of the knee contractures in cerebral palsy patients. Med Arch. 2014; 68(3): 182-183.
- UddenfeldtWort U., Nordmark E., Wagner P., et al.: Fractures in children with cerebral palsy: a total population study. Dev Med Child Neurol. 2013; 55(9): 821-826.
- McPhee P.G., Gorter J.W., Cotie L.M., et al.: Descriptive data on cardiovascular and metabolic risk factors in ambulatory and non-ambulatory adults with cerebral palsy. Data Brief. 2015; 5: 967-970.
- Wong D.L., Baker C.M.: Smiling faces as anchor for pain intensity scales. Pain. 2001; 89(2-3): 295-300.
- Milch H.: The pelvic support osteotomy. 1941. Clin Orthop Relat Res. 1989; 249: 4-11.
- Caulton J.M., Ward K.A., Alsop C.W., et al.: A randomised controlled trial of standing programme on bone mineral density in non-ambulant children with cerebral palsy. Arch Dis Child. 2004; 89(2): 131-135.
- McGinley J.L., Dobson F., Ganeshalingam R., et al.: Single-event multilevel surgery for children with cerebral palsy: a systematic review. Dev Med Child Neurol. 2012; 54(2): 117-128.
- Popkov D.A., Zmanovskaya V.A., Gubina E.B., et al.: The results of single-event multilevel orthopedic surgeries and the early rehabilitation used in complex with botulinum toxin treatment in patients with spastic forms of cerebral palsy. Zh Nevrol PsikhiatrIm S S Korsakova. 2015; 115(4): 41-8.
- Abu-Rajab R.B., Bennet G.C.: Proximal femoral resection-interposition arthroplasty in cerebral palsy. J Pediatr Orthop B. 2007; 16(3): 181-184.
- Widmann R.F., Do T.T., Doyle S.M., et al.: Resection arthroplasty of the hip for patients with cerebral palsy: an outcome study. J Pediatr Orthop. 1999; 19(6): 805-810.
- Muthusamy K., Chu H.Y., Friesen R.M., et al. Femoral head resection as a salvage procedure for the severely dysplastic hip in non-ambulatory children with cerebral palsy. J Pediatr Orthop. 2008; 28(8): 884-889.
- Leet A.I., Chhor K., Launay F., et al.: Femoral head resection for painful hip subluxation in cerebral palsy: Is valgus osteotomy in conjunction with femoral head resection preferable to proximal femoral head resection and traction? J Pediatr Orthop. 2005; 25(1): 70-73.
- Hogan K.A., Blake M., Gross R.H.: Subtrochanteric valgus osteotomy for chronically dislocated, painful spastic hips. J Bone Joint Surg Am. 2006; 88(12): 2624-2631.



 Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.
Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.