Retrospective analysis of surgical outcomes of ACL reconstruction- A retrospective study
Received: 06-May-2022, Manuscript No. JOTSRR-22-62967; Editor assigned: 09-May-2022, Pre QC No. JOTSRR-22-62967 (PQ); Accepted Date: May 20, 2022 ; Reviewed: 11-May-2022 QC No. JOTSRR-22-62967 (Q); Revised: 16-May-2022, Manuscript No. JOTSRR-22-62967 (R); Published: 31-May-2022, DOI: 10.37532/18972276.2022.17 (1).70
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: Ligament disruption occurs without a fall or direct contact where deceleration along with valgus external rotation or hyper extension force comes into play.
Objective: to determine the clinical outcomes of arthroscopic ACL reconstruction in ACL tear patients reconstructed by semitendinosus and gracillis autograft by retrospective study.
Methods: Patients presenting with unilateral knee complaints in the orthopedic outpatient department of the hospital were evaluated by a thorough general and local clinical examination of the knee. Uninjured knees of normal subjects in supine position were taken as reference.
Results: Nearly all the patients have shown maximum improvement after the surgery with no instability whatsoever during routine and exertional activities. The quality of life of the patient has not been affected by the surgery and is same as it was before the trauma.
Conclusion: ACL reconstruction by semitendinosus-gracilis autograft with a torn anterior cruciate ligament in nearly all the patients who were available for follow up. Significant improvements in functional scores were noted.
Keywords
arthroscopic, ACL reconstruction, Semitendinosus-gracilis autograft.
INTRODUCTION
Anterior cruciate ligaments are an intra-articular, extra-synovial structure present in the central complex of knee joint. It functions in concert with all other anatomical structures in the knee joint to control and limit motion and to maintain both static and dynamic equilibrium. It is commonly injured in athletic activities like rugby, football, hockey, swimming, sprinting, gymnastics and motor vehicle accidents.
The knee joint allows for flexion and extension, but is more than a simple hinge joint demonstrating a rotational component [1]. Three bones articulate at the knee joint, the femur, tibia, and patella. Both the Tibiofemoral (TF) and Patellofemoral (PF) joints are contained within a common capsule. Articular cartilage covers both the medial and lateral condyles of the femur, the medial and lateral condyles of the tibia and inner surface of the patella. The Medial and lateral side of the knee are primarily stabilized by the medial and lateral collateral ligaments respectively. The Medial Collateral Ligament (MCL) is the broader of the two ligaments and is continuous with a semilunar cartilaginous cushion separating the medial condyle of the femur from the medial condyle of the tibia. This structure is known as the medial meniscus. The Lateral Collateral Ligament (LCL) is not attached to the lateral meniscus; it instead spans from the lateral femoral epicondyle to the head of the fibula. The MCL provides valgus stability to the knee whereas the LCL provides the knee with varus stability [2]. The cruciate ligaments are the primary stabilizers of the knee in the anterior and posterior directions. These ligaments are important in keeping the articular surfaces of the femur and tibia in contact, and stabilizing the knee in the sagittal plane. The PCL restricts posterior translation of the tibia on the femur while the ACL restricts anterior translation of the tibia on the femur.
The aim of surgical treatment is to restore knee stability, thereby allowing the patient to return to his original physical activity levels. Selection of appropriate graft in ACL reconstruction is important as allogenic tissue and prosthetic ligaments have shown discouraging results due to short half-life and decreased mechanical strength in contrast to autologous grafts which include bone patellar tendon bone, hamstrings (semitendinosus-gracilis), quadriceps bone, Achilles tendon and iliotibial band. The choice of graft and its fixation plays a key role in ACL reconstruction. An ideal graft would be one that provides as much strength as native anterior cruciate ligament, allows for secure fixation, has minimal harvest site morbidity, enables unrestricted rehabilitation and restores normal knee biomechanics and kinematics. The mid-third bone, patellar tendon bone and multiple stranded hamstring tendons (semitendinosus-gracilis) are the most frequently used auto-grafts today [3,4].
The bone-patellar tendon bone auto-graft is considered to be the “gold standard” because of the bone to bone healing that allows for an early and accelerated rehabilitation with documented good and excellent long term results [5-7].
Hence the study was conducted to determine the clinical outcomes of arthroscopic ACL reconstruction in ACL tear patients reconstructed by semitendinosus and gracillis auto-graft by retrospective study.
Materials and Methods
Patients presenting with unilateral knee complaints in the Orthopaedic outpatient department of the hospital were evaluated by a thorough general and local clinical examination of the knee. Uninjured knees of normal subjects in supine position were taken as reference. The following specific tests were performed for diagnosing ACL deficiency:
Lachman test
• Anterior drawer test
• Lateral pivot shift maneuver
• Injuries to the associated structures were assessed by performing the following clinical tests:
Valgus/ Varus stress test (for collateral ligaments)
• McMurray’s test (for menisci)
• Posterior drawer test (for posterior cruciate ligament)
• Reverse pivot shift test (for posterolateral complex)
Routine skiagrams of the affected knee were taken in standing position in anteroposterior and lateral views. MRI of the knee was done in cases with equivocal clinical findings.
Inclusion Criteria
• Clinical/radiological/arthroscopic evidence of ACL deficiency which is symptomatic
• Young and middle aged, active, motivated patients with future interest in professional/recreational sports or who are involved in vigorous activities, unwilling to change their active life style
• A normal contralateral knee
• The acute inflammatory phase of the injury has subsided and full range of motion and good quadriceps strength has been regained with no extensor lag (usually after 4-6 weeks of injury)
Exclusion criteria
Medial Collateral Ligament and Lateral Collateral Ligament tear
• Meniscal tear
• Bilateral anterior cruciate ligament deficiency
• Presence of fractures around the knee (tibial plateau, patella, femoral condyles)
• Patients with sedentary life style, not keen on pursuing sports in future, and having minimal disability
An informed consent was taken from the selected patients after explaining the procedure, its outcome, complication and the prolonged rehabilitation protocol to be followed subsequently
PREOPERATIVE PERIOD
After pre-anaesthetic check-up, a single dose of a third generation cephalosporin (ceftriaxone; 1 gm) and aminoglycoside (amikacin; 500 mg) was administered intravenously about half an hour prior to procedure.
Procedure
After giving adequate anaesthesia (spinal/spinal and epidural/general), the patient was placed in supine position. The affected knee was correctly identified. Lachmann and pivot shift test performed on the affected knee. High pneumatic electronic tourniquet applied. Scrubbing, painting and draping done. Using a sterile esmarch bandage the limb was exsanguinated, and the tourniquet inflated.
ARTHROSCOPY
Arthroscope was introduced and knee was examined systematically in the w sequence, starting from the suprapatellar pouch, then the patellofemoral joint, medial gutter, medial meniscus, intercondylar notch, lateral meniscus and lateral gutter after making high anterolateral portal.
Once all the pathologies were recorded a second anteromedial portal (working portal) was made at the inferior pole of patella, 1 cm medial to patellar tendon. All associated pathologies were dealt with appropriately like partial menisectomy for a meniscal tear that was unstable to probing, chondral defect shaving and removal of loose bodies.
HAMSTRING GRAFT
A longitudinal skin incision of about 4 cm was given, centered approximately 4 cm medial and just distal to the tibial tubercle or about three finger width below the medial joint line. Semitendinosus tendon was hooked under Pes Anserinus fascia. Deep fascial bands were dissected. Open-end stripper was passed over the tendon one by one and advanced carefully in line with it giving firm, steady but gentle pressure and simultaneously applying counter traction using the previously placed suture. Gracilis usually had a more muscular appearance after harvesting. Graft was harvested.
GRAFT PREPARATION
Grafts were placed on graft master board. They were stripped off their residual muscle fibers proximally using the blunt end of scalpel blade. They were placed together and using a number 5 ethibond suture a running baseball stitch was placed in both tendons in a Chinese finger trap configuration. The tendons were looped (using an mersilene tape around the stitched tendons) and passed through various holes in the graft sizer. Pre-stressing of the graft was done manually.
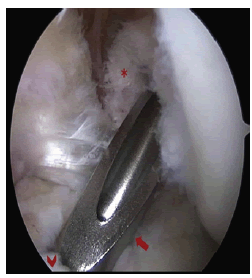
NOTCH PREPARATION
A torn ACL was usually visualized as failing to extend to its normal femoral attachment. The remaining ACL tissue was removed using the basket forceps and the area where graft is to be placed is shaved with electric shaver.
TUNNEL PLACEMENT: TIBIAL TUNNEL
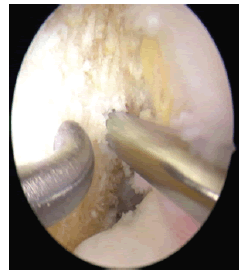
The tibial guide was introduced into the joint through the anteromedial portal after setting the inclination of the zig at 55 degrees. The aimer was placed on the center of the tibial foot print which lies about 6 mm anterior to the PCL in the midpoint and just medial to the posterior edge of the anterior horn of lateral meniscus (Figure 1).
The sleeve was inserted into the guide upto the tibial cortex (through the incision used for graft harvesting) at about 2 cm medial to the tibial tubercle and 4 cm below the joint line. A guide pin was drilled into the joint through the sleeve. The tunnel was then reamed with a cannulated headed reamer placed over the guide pin, starting from 8 mm size upto the size determined by graft sizer (Figure 2).
FEMORAL TUNNEL
Femoral offset guide was introduced into the joint through the tibial tunnel and engaged into “over the top” position with the knee in 90° flexion. The guide was aimed at 2 o’clock position in the left knee and 10 o’clock in the right knee. An appropriate sized offset guide was used so as to leave about 2 mm of posterior cortical wall after drilling the femoral tunnel (7 mm size for 10 mm reamed tunnel). The guide pin was then drilled through the intercondylar region and lateral femoral cortex to emerge out of the anterolateral aspect of the thigh. An appropriate sized cannulated calibrated reamer was threaded over the pin and femoral tunnel reamed upto the 40 mm mark on the calibrated reamer. The sharp edges of the femoral tunnel were smoothened by shaver and debris removed.
GRAFT PLACEMENT AND FIXATION
Hamstring Graft: The size specific tunnel (marking) hook was mounted on the C-ring of the femoral guide and inserted through the tibial tunnel into the femoral socket.
The guide pin sleeve was placed against the lateral femoral cortex and a 3 mm guide pin was drilled through it, in a direction slightly posterolateral to anteromedial in the coronal plane coming out through the medial skin.
The guide pin was then drilled back and forth a few times to loosen it for its easy removal subsequently. The outer cortex of the lateral femoral condyle was drilled over cortical reamer with a depth stop.
The fine the guide pin and the guide pin was pulled through the condyles. The tunnel hook was then withdrawn out pulling the loop of wire down through the femur and out of the tibial tunnel. The hook was then disengaged from the wire loop and the prepared tendon graft was loaded at its middle on to the wire loop. The graft was passed through the tibial tunnel and up into the femoral socket.
With the help of titanium endobutton, Merselene tape,ethibond no 2, vicryl no 1.the flip flop technique was adopted. The graft was then placed under tension and knee was cycled several times to remove “creep” from the graft construct. The knee was then placed in about 20-30 degrees of flexion; an appropriate sized headless Titanium screw (usually same size of the diameter of tibial tunnel) was inserted into the tibial tunnel until it was buried just below the cortex. If fixation was found to be inadequate, a staple was used in addition, just distal to the tibial tunnel.
CLOSURE
After giving adequate wash to the joint. The subcutaneous tissue was closed with an interrupted no. O vicryl suture and skin was closed with interrupted ethilon no. 2-0 sutures. The portal sites were closed with ethilon 2-0 suture. A sterile dressing was applied. After applying a pressure bandage, tourniquet deflated and tourniquet time noted. Knee was subsequently placed in a brace locked in extension.
POSTOPERATIVE CARE
Patient was encouraged to lie supine with foot end elevated for 24 hours, as spinal anaesthesia was given during procedure. He was encouraged to use ice packs to reduce the swelling. Round the clock analgesia (initially i.v., later oral) was administered to assist in physiotherapy. Wound inspection was done on 3rd postoperative day. Only if the wound was healthy and patient’s compliance for phvsiotherapy was assured, the patient was discharged on oral antibiotics. Sutures were removed on 14th postoperative day.
Results
The study comprised of a cohort of 50 patients with anterior cruciate ligament tear who were treated surgically by arthroscopic ACL reconstruction. Out of which forty five patients (90%) were males. The mean age was 30.7 (range 20 to 50). All the patients were examined in the OPD and operation theatre preoperatively. A scoring system “Tegner and Lysholm” score was used. Patients were scored based on this questionnaire.
Nearly all the patients with Anterior cruciate ligament tear had instability preoperatively which was not there after the operative management. Most of the patient resumed their respective activities 6 weeks after the surgery and were comfortable doing exertional activities after 6 months.
Most of these patients have complaints of pain and instability before the surgery. Most of the patients were engaged in some exertional activities (Table 1).
Table 1: Distribution of study subject
| Sport activity | Yes | No |
|---|---|---|
| N=50 | 40 | 10 |
Our study was a retrospective study of 50 patients Mean pre-op score was 59.1 which improved to 82.48 in 6 months after the arthroscopic ACL reconstruction and to 91.22 after 12 months and to 96.84 after 24 months respectively. Nearly all the patients have shown maximum improvement after the surgery with no instability whatsoever during routine and exertional activities. The quality of life of the patient has not been affected by the surgery and is same as it was before the trauma (Table 2).
Table 2: Distribution of knee symptoms
| Time duration | Poor (< 65) | Fair (65-83) | Good (84-90) | Excellent ( >90) |
|---|---|---|---|---|
| 6 months | 0 | 48% | 52% | 0% |
| 12 Months | 0 | 2% | 40% | 58% |
| 24 Months | 0 | 0 | 2% | 98% |
Discussion
Successful clinical outcomes following anterior cruciate reconstruction with hamstring graft have been reported by many authors [8, 9]. In our study anterior cruciate reconstruction with a hamstring graft resulted in a successful clinica outcome in almost all the patients who had come for follow-up.
Nebelung, et al. reviewed the results of twenty-nine anterior cruciate reconstructions with an autogenous semitendinosusand gracilis tendon and a femoral Endobutton 75). They graded 66% of the results as normal or nearly normal using the criteria of the International Knee Documentation Committee. In the present study, we analyzed the effectiveness of a semitendinosus- gracilis graft in eliminating symptomatic anterior tibial subluxation caused by a torn anterior cruciate ligament. Anterior tibial subluxation was eliminated in almost all the patients who had followed up for two years.
With the rehabilitation protocol used in our study, the majority of patients returned to a high functionalstatus in 6 months. No motion deficits or clinically important knee pain was noted at the followup examination. Other authors have reported success with similar rehabilitation protocols following anterior cruciate reconstruction [10]. We allow full weight-bearing with the knee in terminal extension in a brace in the immediate limited active and employ immediate passive range of motion following the reconstruction.
Hoffmann, et al. reported in the results sixty-five patients of anterior cruciate reconstruction with semitendinosus-gracilis graft and-Endobutton construct that was augmented with an extra-articular lateral repair [11].
In this study no patients who were treated by hamstring graft reconstruction for ACL tear didn’t require extra-articular lateral repair.
Bach, et al. reported a reoperation rate of 15% in a series of 103 patients evaluated two years after anterior cruciate reconstruction with a patellar tendon auto-graft. In this study all the patients were treated with hamstring graft and no reoperation was required [12].
In their study of 2500 consecutive arthroscopically assisted anterior cruciate reconstructions performed. Williams, et al. reported an infection rate of 0.03%; one patient had a superficial infection of the knee following the anterior cruciate reconstruction. In our study patients were treated effectively by a combination of parenteral and oral antibiotics for a total 2 weeks and NO postoperative infection was noted in the follow up patients [13].
Clinically relevant patellofemoral pain or loss of knee motion has been reported following anterior cruciate reconstruction with the patellar tendon but neither was observed in our study. The elimination of knee instability and the functional scores in our series were consistently good.
We did not observe any clinically relevant knee pain or motion loss at the time of follow-up. The absence of such morbid findings following anterior cruciate reconstruction with hamstring graft makes this method of reconstruction more desirable for the patients with ACL tear.
Conclusion
We found that ACL reconstruction by semitendinosus-gracilis autograft with a torn anterior cruciate ligament in nearly all the patients who were available for follow up. Significant improvements in functional scores were noted. Arthroscopic ACL reconstruction is an effective treatment option for patients with symptomatic ACL tears without any concerns regarding knee extensor mechanism or anterior knee pain.
Acknowledgement
Author would like to express his profound gratitude to all the participants.
Contribution details
Concept, design, manuscript editing, manuscript review process was carried out by all authors. Literature search, data acquisition, data analysis, statistical analysis and manuscript preparation were done by Ankur Singhal and Lalit Jain. Dr Ankit is the guarantor of this manuscript.
References
- Beynnon BD, Johnson RJ, Abate JA, et al.: Treatment of anterior cruciate ligament injuries, part I. Am Sports Med. 2005 Oct;33(10):1579-602. Google scholarCrossref
- Ross LM, Lamperti E.: Thieme atlas of anatomy: General anatomy and musculoskeletal system. 2006 Google scholarCrossref
- Bartlett R.J., Clatworthy M.G., Nguyen T.N.: Graft selection in reconstruction of the anterior cruciate ligament. J Bone Joint Surg Br. 2001 Jul;83(5):625-34. Google scholarCrossref
- Frank C.B., Jackson D.W.: Current concepts review-the science of reconstruction of the anterior cruciate ligament. JBJS. 1997 Oct 1;79(10):1556-76. Google scholarCrossref
- Yunes M., Richmond J.C., Engels E.A., et al.: Patellar versus hamstring tendons in anterior cruciate ligament reconstruction: a meta-analysis. Arthroscopy. J Arthrosc. Relat Surg. 2001 Mar 1;17(3):248-57.Google scholarCrossref
- Shelbourne K.D., Gray T.: Anterior cruciate ligament reconstruction with autogenous patellar tendon graft followed by accelerated rehabilitation: a two-to nine-year followup. Am j sports med. 1997 Nov;25(6):786-95.Google scholarCrossref
- Shelbourne K.D., Wilckens J.H.: Current concepts in anterior cruciate ligament rehabilitation. Orthop. rev. 1990 Nov 1;19(11):957-64.Google scholarCrossref
- Muneta T., Sekiya I., Ogiuchi T., et al.: Effects of aggressive early rehabilitation on the outcome of anterior cruciate ligament reconstruction with multi-strand semitendinosus tendon. Int. orthop. 1998 Dec;22(6):352-6.Google scholarCrossref
- Aglietti P., Buzzi R., Menchetti P.P., et al.: Arthroscopically assisted semitendinosus and gracilis tendon graft in reconstruction for acute anterior cruciate ligament injuries in athletes. Am j sports med. 1996 Nov;24(6):726-31. Google scholarCrossref
- Barber F.A.: Tripled semitendinosus–cancellous bone anterior cruciate ligament reconstruction with bioscrew fixation. Arthroscopy. J Arthrosc. Relat Surg. 1999 May 1;15(4):360-7.Google scholarCrossref
- Hoffmann F., Friebel H., Schiller M.: The semitendinosus tendon as replacement for the anterior cruciate ligament. Zentralblatt fur Chirurgie. 1998 Jan 1;123(9):994-1001.Google scholarCrossref
- Bach B.R., Levy M.E., Bojchuk J., et al.: Single-incision endoscopic anterior cruciate ligament reconstruction using patellar tendon autograft. Am j sports med. 1998 Jan;26(1):30-40.Google scholarCrossref
- Williams III R.J., Laurencin C.T., Warren R.F., et al.: Septic arthritis after arthroscopic anterior cruciate ligament reconstruction: diagnosis and management. Am J Sports Med.1997 Mar;25(2):261-7.Google scholarCrossref



 Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.
Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.