Sliding soleus flap - A useful flap in primary management of compound wounds of leg
Received: 22-Jun-2017 Accepted Date: Jul 04, 2017 ; Published: 06-Jul-2017
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: Lower leg trauma with compound wounds of leg with need for wound cover are common injuries encountered by plastic surgeons. Soleus flap is an extremely useful flap in acute management of compound fractures of lower leg especially middle and lower third. However, the soleus being in zone of trauma in such defects, reconstructive surgeons hesitate to use it primarily. This article proposes a novel way of using the soleus muscle by sliding it across the defect and not transecting its lower end as traditionally done. Although many of these wounds can be managed secondarily, addressing the wound primarily with the exposed soleus helps reduces need for more complex reconstructive surgery at a later surgical sitting.
Aims and objectives: The aim of this study is to assess the usefulness of the sliding soleus flap in covering compound wounds of middle and lower third of leg.
Material and methods: The study was conducted during the period between April 2010 to April 2015. The sliding soleus was used to cover 25 cases of lower leg trauma with middle and lower leg defects up to 10 cm above ankle joint.
Results: All the flaps survived though in some cases superficial necrosis was encountered. In these cases, the necrosis was debrided during dressings and did not require any operation theater intervention.
Conclusion: In the acute trauma scenario where the plastic surgeon is called upon to address compound fractures of tibia and fibula, it is recommended to close the exposed bone with sliding soleus flap. Here the soleus muscle is slided into defect without transection. The sliding soleus flap has three advantages. One it has vascularity of both dominant and minor vascular pedicle and is more reliable compared to either a proximal or reversed soleus flaps. The second advantage is that there is no functional deficit as the muscle is only transposed and not disconnected. Thirdly the reach of the soleus muscle for coverage of upper lower third leg defects can be achieved.
Keywords
Sliding soleus, Compound, Lower leg trauma, Bone, Flaps
Introduction
Lower leg trauma with compound wounds are very common injuries where the need for plastic surgeon is sought. Very often these cases are managed secondarily due to either non-availability of plastic surgeons or the orthopedic surgeons feel the bone work needs immediate attention and wound cover can be done by the reconstructive team of plastic surgeons at a later date.
However primary management of these compound wounds by the plastic surgeon has many advantages. Firstly, flap cover can be done in primary sitting with the same anaesthesia. Secondly the status of the surrounding muscles including viability can be ascertained by the plastic surgeon and bone is covered at earliest reducing chances of bone infection. Thirdly the plastic surgeon can guide the orthopedic team regarding placement of the pins of external fixation to suit the flap cover. Very often we see the pins of external fixator passing directly on wound or bone which can be avoided by presence of plastic surgeon.
The soleus muscle is a very versatile and robust muscle which is very useful in coverage of defects of middle third of the leg. Traditionally this muscle has been used for middle third leg defects and not for lower third defects as it has to be transposed after cutting the muscle at the musculotendinous junction. Secondly the bulk and function of soleus is lost when it has been cut at lower end.
We propose the sliding soleus flap for coverage of these defects. We have used the sliding soleus flap in 25 cases in the acute scenario when called upon by our orthopedic colleagues in compound fractures of lower leg. We call it sliding because the soleus is not divided and only is slided into the defect.
Subjects and Methods
The study was conducted during the period between April 2010 to April 2015 in a single hospital by a single plastic surgeon. The sliding soleus was used to cover 25 cases of lower leg trauma with middle and lower leg defects.17 cases were male patients and 8 female patients. The youngest patient was aged 7 years and oldest aged 74 years. Out of these 25 cases primary skin grafting was done in about 5 cases and in the rest 20 cases skin grafting was done secondarily after about 10 days. In 22 cases, there was associated fractures requiring external fixation. 3 cases had exposed bone but no fracture. In 5 cases, the defect was restricted to middle third, in 12 cases the defect involved middle and lower third and 8 cases involved only lower third defects. Defect sizes varied from largest 12 x 5 cm to smallest 4 x 3 cm (Table 1). Cases were followed up for minimum period of 6 months. Lower leg defects upto 10 cm from ankle were excluded as the soleus muscle becomes tendinous and forms the tendoachilles. Skeletal stabilization was only by external fixation and internal fixation was not done in any of compound wounds. Compound 3c fractures with vascular compromise were excluded.
| Age/Sex | Diagnosis | Defect size | Grafting type |
|---|---|---|---|
| 43/male | Compound fracture tibia | 12 × 5 cm | Secondary |
| 23/male | Compound fracture tibia and fibula | 11× 3 cm | Secondary |
| 35/male | Compound fracture tibia | 10 × 4 cm | Secondary |
| 30/male | Degloving with Exposed tibia | 8 × 5 cm | Secondary |
| 40/male | Compound fracture tibia | 7 × 4 cm | Primary |
| 20/female | Compound fracture tibia and fibula | 11 × 5 cm | Secondary |
| 25/male | Compound fracture tibia | 9 × 4 cm | Secondary |
| 17/male | Compound fracture tibia | 7 × 5 cm | Secondary |
| 74/male | Degloving with Exposed tibia | 6 × 5 cm | Secondary |
| 36/male | Compound fracture tibia and fibula | 10 × 5cm | Secondary |
| 18/male | Compound fracture tibia | 9 × 4 cm | Secondary |
| 7/female | Compound fracture tibia | 4 × 3 cm | Secondary |
| 55/male | Compound fracture tibia and fibula | 10 × 4 cm | Secondary |
| 60/female | Degloving with Exposed tibia | 9 × 5 cm | Secondary |
| 45/female | Compound fracture tibia | 10 × 4 cm | Secondary |
| 42/female | Compound fracture tibia | 12 × 4 cm | Secondary |
| 27/male | Compound fracture tibia and fibula | 8 × 4 cm | Secondary |
| 30/male | Compound fracture tibia | 11 × 4 cm | Secondary |
| 15/female | Compound fracture tibia | 10 × 5cm | Secondary |
| 54/male | Compound fracture tibia and fibula | 11 × 4 cm | Primary |
| 23/female | Compound fracture tibia | 10 × 4 cm | Primary |
| 43/male | Compound fracture tibia and fibula | 9 × 5 cm | Secondary |
| 56/male | Compound fracture tibia | 8 × 4 cm | Primary |
| 30/male | Compound fracture tibia | 9 × 4 cm | Primary |
Table 1: Defect sizes varied from largest 12 × 5 cm to smallest 4 × 3 cm.
Operative Technique
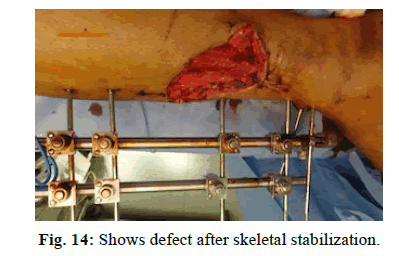
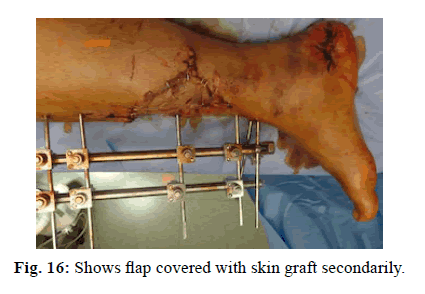
After the skeletal stabilization with external fixator in case of associated tibia fractures, the soleus is assessed for viability. Bleeding of muscle and muscle contraction on stimulation are useful in assessing viable muscle. The area of exposed bone is then assessed and the soleus muscle is gently separated from the other muscles by blunt dissection with fingers. The soleus muscle is then trans-posed anteriorly to cover the exposed tibia without cutting the muscle at its lower end. The muscle edges are stitched to surrounding soft tissue after covering the exposed bone. Sharp dissection is avoided to prevent injury to posterior tibial vessels. The use of relaxing incisions on epimysium to increase reach of muscle has been described but in our series, we did not require use of this method [1]. Majority of cases entire soleus muscle is not required and only part of sliding soleus muscle is sufficient to cover defect. In case of any doubt about the viability of soleus muscle, the skin grafting is done secondarily. Otherwise split skin graft can be done in primary sitting over the soleus muscle.
Presenting some of these illustrative examples.
Case 1
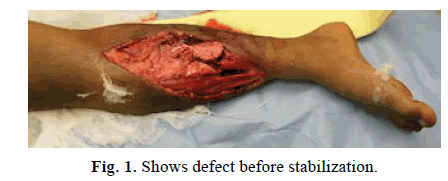
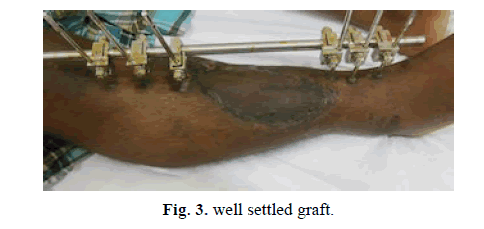
A 43-year-old male with compound fracture of tibia covered with soleus flap and skin grafted immediately (Figures 1-3).
Case 2
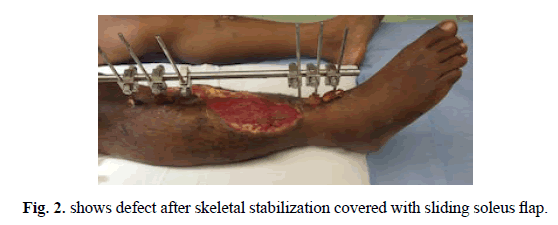
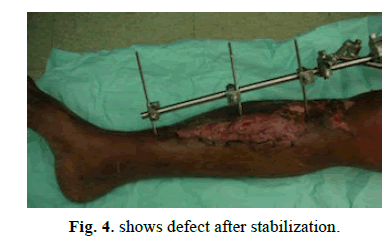
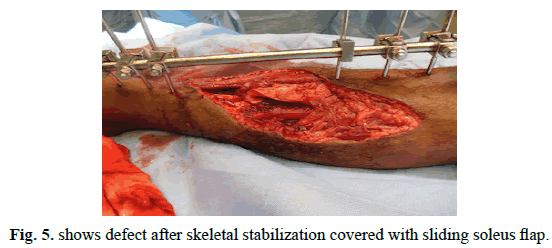
A 23-year-old male with compound fracture of tibia and fibula covered with sliding soleus and skin grafted secondarily (Figures 4-6).
Case 3
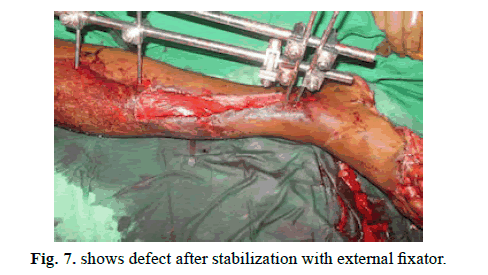
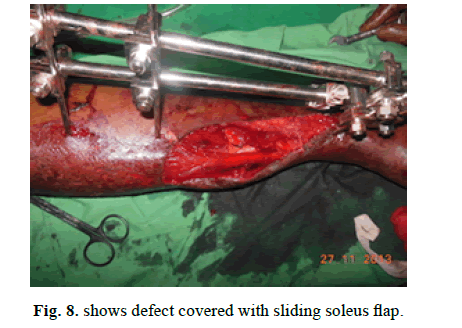
A 35-year-old male with compound fracture of tibia covered with sliding soleus flap and skin grafted secondarily (Figures 7-9).
Case 4
A 30-year-old male with exposed tibia following vehicle runover covered with sliding soleus flap (Figure 10-12).
Case 5
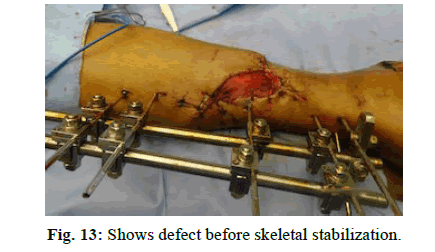
A 40-year-old male with compound fracture of tibia covered with sliding soleus flap cover (Figure 13-16).
Results
All the flaps survived and wounds healed. We did encounter superficial flap necrosis in some cases which were debrided during dressings without need for an operative theater intervention. Small raw areas following skin grafting were managed with dressings and secondary healing. We did delay the skin grafting primarily whenever there was doubtful vascular reliability of the muscle but did not encounter any significant muscle necrosis in any of our cases. Although only 5 of our cases were primarily skin grafted most of these cases are more recent as we were more confident of survival of the sliding soleus flap.
There was no functional impairment following the use of the sliding soleus flap in the form of gait disturbances or limp. Plantar flexion was not altered in any of cases done. Illizarov technique was used to treat 2 patients with bony non-union after flap settlement.
Discussion
The soleus muscle is a large, broad, flat muscle lying immediately deep to gastrocnemius muscle [2]. It contributes to the bulk of the calf, the soleus constituting approximately about 45% of leg circumference in proximal third of leg. At the tibial midpoint, the soleus constitutes approximately 35% of leg circumference. The muscle fibres converge into an aponeurosis that joins the tendon of gastrocnemius to form the achilles tendon. The muscle insertion is on the tendocalcaneus 6.0 +/- 1.7 cm above the calcaneus [3].
The soleus is a type II muscle with a dominant vascular pedicle and minor vascular pedicles [4].
Proximally based soleus, hemisoleus and soleus musculocutaneous flaps are exceptionally hearty and highly reliable. These flaps may fail if their proximal vascular pedicles or the major vascular supply of the limb are compromised by trauma or arteriosclerosis obliterans. The soleus has been used primarily for middle third defects with higher failure rates when used in lower third defects [5]. Reversed soleus flaps have reported failure rates greater than 21%. Accordingly, reversed soleus flaps usually are reserved for secondary salvage procedures [3].
Although the soleus is the prime ankle plantar flexor, functional deficit following transfer is lessened by both surgical maneuvers and synergistic muscle strengthening and alteration of gait. When hemisoleus flaps are used, the contralateral muscle belly remains in situ to preserve soleus function [6]. Soleus deficit not relieved by synergistic calf-muscle strengthening is compensated for by lessening of forward lean, earlier contralateral heel strike and shorter stride [3].
The sliding soleus flap has three advantages. One it has vascularity of both dominant and minor vascular pedicle and is more reliable compared to either a proximal or reversed soleus flaps. The second advantage is that there is no functional deficit as the muscle is only transposed and not disconnected. Thirdly the reach of the soleus muscle for coverage of upper lower third leg defects can be achieved as the muscle is only transposed and not divided.
Conclusion
The sliding soleus flap is a very useful flap in the acute trauma scenario of open compound wounds of lower leg. Providing good supply, the muscle reduces chance of bone infection, reduces need for multiple secondary surgeries and significantly reduces need for more complex reconstructive options.
In the acute trauma scenario where the plastic surgeon is called upon to address compound fractures of tibia and fibula, it is recommended to close the exposed bone with sliding soleus flap. Such wounds if not handled primarily will require either free flaps or cross leged flaps at a later sitting. Here the soleus muscle is slided into defect without transection. The sliding soleus flap has three advantages over traditional soleus flap. One it has vascularity of both dominant and minor vascular pedicle and is more reliable compared to either a proximal or reversed soleus flaps. The second ad-vantage is that there is no functional deficit as the muscle is only transposed and not disconnected. Thirdly the reach of the soleus muscle for coverage of upper lower third leg defects can be achieved as the muscle is only transposed and not divided. With these distinct advantages over the traditional soleus flap, the sliding soleus flap can be a very useful flap for reconstructive surgeons.
REFERENCES
- Wright J.K., Watkins R.P.: Use of the soleus muscle flap to cover part of the distal tibia. Plast Reconstr Surg. 1981; 68(6): 957-958.
- Nahai M.: Clinical atlas of muscle and musculocutaneous flaps. Mosby Company. 1979; 158.
- Grabb’s Encylopedia of flaps, (2nd edn). Lippincott-Raven publications. 1998; 1759-1763.
- Grabb and Smith’s Plastic surgery. (6th edn). Lippincott-Raven publication. Pg.44.
- Kauffman C.A., Lahoda L.U., Cederna P.S.: Use of soleus muscle flaps for coverage of distal third tibial defects. J Reconstr Microsurg. 2004; 20(8): 593-597.
- Ahmad I., Akhtar S., Rashidi E., et al: Hemisoleus muscle flap in the reconstruction of exposed bones in the lower limb. J Wound Care. 2013; 22(11): 635: 638-40, 642.









 Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.
Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.