Surgical outcomes of arthroscopic rotator cuff repair with modified Mason-Allen suture technique combined with microfracture procedure at the attachment site
2 E Hospital, Vietnam
3 Hanoi Medical University, Hanoi, Vietnam, Email: abc@gmail.com
4 Tam Anh hospital, Vietnam, Email: abc@gmail.com
5 Saint-Paul hospital, Hanoi, Vietnam, Email: dungbacsy@dungbacsy.com
Received: 03-Mar-2021 Accepted Date: Mar 17, 2021 ; Published: 30-Mar-2021, DOI: 10.37532/1897-2276.2021.16(1).10
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: Rotator Cuff Tear (RCT) is a lesion that cannot be reversed, usually requiring surgery. Several techniques have been introduced to repair RCT. In general, the purposes of these techniques are aimed at restoring the mechanical strength of the tendons, reducing the rate of tendon re-tear and increasing the rate of tendon healing, thereby increasing functional outcomes after surgery. Material and Methods: This prospective longitudinal followup study included 60 patients of full-thickness RCT who underwent arthroscopic rotator cuff repair with modified Mason-Allen suture technique combined with microfracture procedure at the attachment site between January 2019 and March 2020. The patients were evaluated functional results after surgery based on ASES score and UCLA score. Tendon healing was assessed based on MRI according to Sugaya classification. The average ASES scores before and after surgery were 28.02 ± 15.36 and 96.35 ± 4.57, respectively. The average UCLA score after surgery was 33.07 ± 1.83. Forty-one out of 60 patients had postoperative MRI, showing type I, type II, type III, type IV, and type V tendon healing respectively in 23 patients (56.1%), 9 patients (22.0%), 4 patients (9.8%), 2 patients (4.9%), and 3 patients (7.3%). Conclusions: The arthroscopic modified Mason Allen suture technique combined with microfracture procedure at the attachment site for the treatment of rotator cuff tear had good postoperative results, especially in patients with small and moderate tears in terms of the rate of tendon healing and postoperative shoulder function.
Keywords
rotator cuff tear, modified Mason Allen, microfracture
Introduction
Rotator cuff tear is a common cause of shoulder pain and mobility restriction [1]. RCT cannot be reversed and often require surgical intervention. Rotator cuff repair is an important treatment for RCT and has been shown to have good long-term results [2-3]. However, postoperative tendon re-tear is still recorded with the rate varying from 4-94% [4-7]. Many factors, including both the patients and the surgeons, can affect postoperative tendon healing. Surgeon-related factors that may affect tendon healing outcomes include suture techniques, rehabilitation, and biological factors used in surgery (platelet-rich plasma and mesenchymal stem cells) [8].
Single-row repair is the first known classic in arthroscopic rotator cuff repair. In this technique, the anchors are placed in an anterior-posterior line into the greater tuberosity, each anchor spaced a few millimeters apart [9]. In 2003, Scheibel and Habermeyer introduced the single-row modified Mason-Allen technique in arthroscopic cuff repair. There have been many studies showings the biomechanical superiority of this technique compared to other single-row repair techniques in terms of the attachment site coverage, tension resistance, space reduction, and clinical results [10].
Several authors have investigated the associated factors that increase the rate of postoperative tendon healing and have found that poor quality of bone and tendon tissue can affect tendon-to-bone healing. This is thought to be the main cause of tendon failure or re-tearing [11-13]. Some authors have acknowledged that current techniques for increasing tendon perfusion such as cortical grinding do not provide sufficient and optimal vascular supply for the repaired tendon. They argue that the deep holes in the greater tuberosity (bone marrow outlet) may facilitate the release of factors from the bone marrow such as stem cells, growth factors, and other proteins that help active and increase tendon-to-bone healing [14, 15]. From the above problems, we conduct a study to evaluate the surgical outcomes of arthroscopic rotator cuff repair with a modified Mason-Allen suture technique combined with a microfracture procedure at the attachment site.
Materials and Methods
This prospective longitudinal follow-up study included 60 patients with rotator cuff tear who underwent arthroscopic rotator cuff repair using single-row modified Mason-Allen suture technique by Scheibel and Habermeyer [10], combined with microfracture procedure at the attachment site follow the techniques of Stephen J Snyder and Guiseppe Milano [14,15].
Surgical Technique
Surgery was performed under general anesthesia with the patient in a beach chair position.
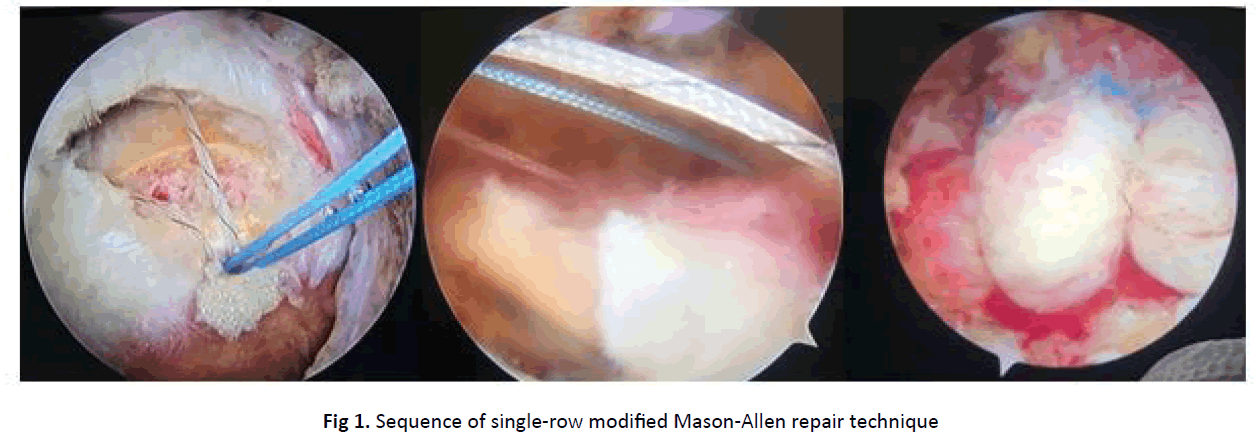
• Sequence of single-row modified Mason-Allen repair technique by Scheibel and Habermeyer [10]:
• Horizontal mattress suture is performed first
• Vertical simple suture is performed later, which will pass through the middle and more medial compared to the mattress suture (Figure 1)
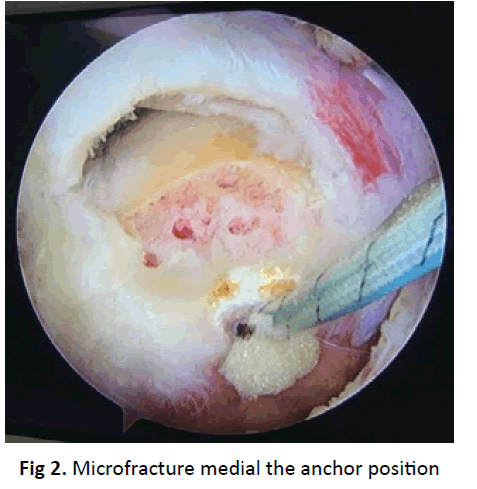
• Microfracture procedure at the attachment site: using an arthroscopic microfracture pick with a diameter of 1.5 mm. Create microscopic holes medial the anchor position (Figure 2)
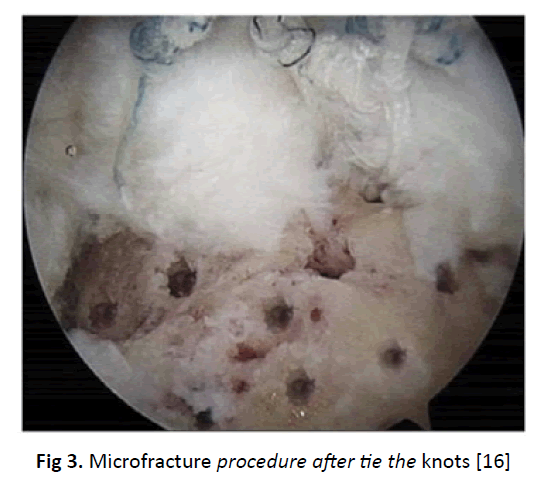
• Tie the horizontal mattress suture first. Next, tie the knot of the remaining simple vertical suture
• After tying all the knots, the area lateral of the anchors and rotator cuff tendon is revealed and more microfracture holes are created (Figure 3)
Figure 3:Microfracture procedure after tie the knots [16].
Data Collection and Analysis
• The degree of RCT according to the classification of Cofield R.H [16]
• Functional assessment after surgery based on UCLA and ASES scoring system [17, 18]. ASES and UCLA scores were assessed at the time of final follow-up (6 months or more).
• Evaluation of tendon healing on MRI based on classification of Sugaya [19, 20] at the time after surgery over 6 months. The MRI imaging was evaluated by an independent experienced radiologist. The difference between the groups was evaluated by Fisher’s exact test. Values of p<0.05 are considered statistically significant.
The study has been approved by the Institutional Review Board of Hanoi Medical University. Statistics were analyzed using the 15.0 statistical software.
Results
The lesion size according to Cofield’s classification was shown in Table 1. Medium tear accounted for the most proportion with 36.6% of patients, large tear accounted for 31.7% of patients, small tear accounted for 20% of patients, a massive tear had the least rate with 11.7% of patients.
| Tear size | N | Percentage |
|---|---|---|
| Massive tear | 7 | 11.7 |
| Large tear | 19 | 31.7 |
| Medium tear | 22 | 36.6 |
| Small tear | 12 | 20 |
| Total | 60 | 100 |
Table 1. Tear size according Cofield R.H classification.
Postoperative MRI was performed on 41 out of 60 patients. The results of tendon healing according to Sugaya’s classification were shown in Table 2. Most cases have type I and type II tendon healing (78%).
The relationship between tendon healing on postoperative MRI and preoperative tear size was shown in Table 3. All 100% of small and medium tear had achieved continuous tendon healing on post-op MRI, in which there were 2 cases of type III tendon healing in the medium tear group (tendon are thinner than usual, but no tendon discontinuity).
| Tendon healing type | N | Percentage |
|---|---|---|
| Type I | 23 | 56.1 |
| Type II | 9 | 21.9 |
| Type III | 4 | 9.8 |
| Type IV | 2 | 4.9 |
| Type V | 3 | 7.3 |
| Total | 41 | 100 |
Table 2.Tendon healing on post-op MRI according to Sugaya classification.
| Tear size/ Tendon healing |
Massive (%) |
Large (%) |
Medium (%) |
Small (%) |
Total | p-value |
|---|---|---|---|---|---|---|
| Type I | 1 (4.4) | 3 (13.0) | 13 (56.5) | 6 (26.1) | 23 (100) | 0.03 |
| Type II | 0 | 5 (55.6) | 2 (22.2) | 2 (22.2) | 9 (100) | |
| Type III | 0 | 2 (50.0) | 2 (50.0) | 0 | 4 (100) | |
| Type IV | 1 (50.0) | 1 (50.0) | 0 | 0 | 2 (100) | |
| Type V | 1 (33.3) | 2 (66.7) | 0 | 0 | 3 (100) | |
| Total | 3 (7.3) | 13 (31.7) | 17 (41.5) | 8 (19.5) | 41 (100) |
Table 3. The ralationship between tendon healing on MRI and severity of tear
| Average ASES score | Mean ± SD | Min-max | p-value |
|---|---|---|---|
| Pre-op ASES score | 28.02 ± 15.36 | 1.67-75 | <0.001 |
| Post-op ASES score | 96.35 ± 4.57 | 76.67-100 |
Table 4. Preoperative and postoperative ASES score .
ASES scores before and after surgery was shown in Table 4. The average ASES score after surgery was 96.35, clearly improved compared to before surgery. The lowest and highest post-op ASES score in this study were 76.67 and 100, respectively. Some patients were able to confidently return to playing tennis, weight training, carrying the babies, carrying heavy objects almost as they did before the injury.
The average post-op UCLA score was 33.07 ± 1.83 (range 17-35). According to the UCLA score, all 100% of patients had good and excellent results.
Discussion
This study had 60 patients with an average follow-up time of 18.52 ± 4.71 months (range 11 months-26 months). Among these patients, according to Cofield R.H classification, medium tear accounted for the most (36.6%), and large tear accounted for the second rate (31.7%) [16]. The characteristic of the disease often appears with pain and limited movement due to pain. Most patients were trying to endure or bought medication by themselves or use traditional treatment. Therefore, patients came to us when the disease has been for a long time, so the morphology of small tears accounted for a low rate compared to others.
As a result, we had average preoperative and postoperative ASES scores of 28.02 ± 15.36 and 96.35 ± 4.57, respectively. Comparing the average ASES scores before and after surgery by “t-test”, the difference was statistically significant with p<0.001.
Although there are no studies in Vietnam comparing the results between conservative and surgical treatment, our patients often had previous medical treatment with NSAIDs, sometimes oral or injected corticosteroids. Furthermore, until the present time, there is no specific treatment for RCT. Therefore, it can be considered as a preoperative shoulder function as a self-control group. And based on the above results, we found that arthroscopic rotator cuff repair had very good results.
The authors such as Gartman, Ruotolo [21,22] have compared the results of conservative surgical treatment, they found that conservative treatment results were usually not good as the surgical tendon repair even though it was open repair, arthroscopic assisted mini-open repair, or arthroscopic repair. In addition to the ASES score, we used UCLA scores to evaluate postoperative shoulder function. The average postoperative UCLA score was 33.07, all patients had good or excellent results, of which 21 cases were excellent (35%), 39 cases were good (65%). All patients were satisfied with the results of the surgery. This result is also relatively consistent with other authors [23-25].
We use the Sugaya classification of tendon healing because it includes not only structural properties but also the signal strength within the tendon. This classification achieves a high level of reliability between orthopedists and radiologists. Sugaya classification system has better reliability than Goutallier (0.39-0.55) and Warner system (0.49-0.54) [15, 26]. It is also the most used system in the evaluation of tendon healing after rotator cuff repair, has been used in 33 studies [7].
According to Saccomanno M.F et al., tendon healing after rotator cuff repair is a prominent problem, especially for large and massive tears [27]. Several studies have shown a correlation between clinical outcomes with rotator tendon integrity on postoperative MRI. Tendon integrity is important for patient outcomes as better function and better pain relief [26, 28]. Only 41 of 60 (68.33%) patients agreed to have postoperative MRI due to the cost of MRI scan. Moreover, the patients found that the postoperative results were good, so only a few patients agreed to have post-op MRI. According to Sugaya classification on 41 patients in this study, the number of cases with the healed tendon (type I, II, III) accounted for the majority with 36 patients (87.8%), only 5 patients (12.2%) with the non-healed tendon (type IV, V).
In our study, the rate of the non-healed tendon was 12.2%, which was lower than that of Cho N.S et al. in 2011 (33.3%) [36]. This high rate of tendon healing may be because our study had a small sample size, not all 100% of patients undergoing post-op MRI to assess tendon healing. Besides, patients with small and medium tear sizes accounting for a high rate of 56.67% (34 patients). Or this high rate of tendon healing may be due to our technical change. In 2004, Benjamin Ma et al. reported the experimental results on sheep tendons, which suggested that modified Mason-Allen suture was biomechanical better than the other single-row suture techniques in rotator cuff repair [28]. Lorbach et al., Khalil, and Rashwan in their empirical and clinical studies also showed that arthroscopic modified Mason-Allen suture could achieve biomechanical results comparable to the suture-bridge technique and reduce the number of anchors used [29, 30]. The cases of small and medium tear size in our study have shown the superiority of this technique, with 100% of healing tendon and no re-tear.
Another important part is that we use microfracture procedure in the surgical process, which is a viable method to obtain bone marrow stem cells [15, 29-34], and possibly it is a positive factor in increasing the rate of tendon healing. However, most of the patients in our study were at the age of 45 years or older, this is the age at high risk of osteoporosis, so the creation of microfracture was carried out very carefully. We used a small K-wire with a diameter of 1.2 mm to pre-leak bone quality and based on that to estimate the location, distance, and some microfracture lesions that would be created. Snyder and Burns [14, 35] have the first report on the use of the “bone punching” technique in arthroscopic rotator cuff repair. Then, Jo et al. [31, 32] reported two consecutive studies of a method of making multiple holes in the greater tuberosity to generate bone marrow cell sources, showing the significantly lower re-tear rate in the double-row suture technique, however, the clinical difference was not significant
Recently, Milano et al. [15] randomly assigned 80 rotator cuff tear patients to two groups with the same suture technique, but the difference between the two groups was the presence and absence of microfracture procedure at the greater tuberosity. Although the authors did not see any difference between the two groups, after classifying patients according to lesion size, they found that the microfracture group showed a better tendon healing rate in the patients with the large lesion. Prabjit et al. in their meta-analysis based on data sources from MEDLINE, Embase, PubMed, Cochrane Central Register of Controlled Trials, and clinicaltrials.gov also showed that using microfracture procedures has reduced the rate of postoperative tendon re-tear [35].
Conclusion
Through the study evaluating 60 patients who underwent arthroscopic rotator cuff repair using modified Mason-Allen suture and microfracture procedure at the attachment site, we found that this surgical method has very good results. The rate of postoperative tendon healing was high, for the small and medium tear group, 100% has no tendon re-tear. Postoperative ASES score improved much compared to before surgery. All 100% of patients achieved good and excellent results according to the UCLA score. All patients were satisfied with the results of the surgery.
REFERENCES
- Frank J.B., ElAttrache N.S., Dines J.S., et al.:. Repair site integrity after arthroscopic transosseous-equivalent suture-bridge rotator cuff repair. Am J Sports Med. 2008;36:1496-503
- Gulotta L.V., Nho S.J., Dodson C.C., et al.: Prospective evaluation of arthroscopic rotator cuff repairs at 5 years: Part II–prognostic factors for clinical and radiographic outcomes. J Shoulder Elbow Sur. 2011;20:941-6.
- Galatz L.M., Griggs S., Cameron BD., et al.: Prospective longitudinal analysis of postoperative shoulder function: A ten-year follow-up study of full-thickness rotator cuff tears. JBJS. 2001;83:1052-6.
- Cole B.J., McCarty III L.P., Kang R.W., et al.: Arthroscopic rotator cuff repair: prospective functional outcome and repair integrity at minimum 2-year follow-up. J Shoulder Elbow Sur. 2007;16:579-85
- Lafosse L., Brozska R., Toussaint B., et al.: The outcome and structural integrity of arthroscopic rotator cuff repair with use of the double-row suture anchor technique. JBJS. 2007;89:1533-41.
- Galanopoulos I., Ilias A., Karliaftis K., et al.: The impact of retear on the clinical outcome after rotator cuff repair using open or arthroscopic techniques-A systematic review. Open Orthop J. 2017;11:95–107.
- Malavolta E.A., Assunção J.H., Ramos F.F., et al.: Serial structural MRI evaluation of arthroscopy rotator cuff repair: Does Sugaya’s classification correlate with the postoperative clinical outcomes?. Arch Ortho Trauma Sur. 2016;136:791-7
- Abtahi A.M., Granger E.K., Tashjian R.Z., et al.: Factors affecting healing after arthroscopic rotator cuff repair. World J Ortho. 2015;6:211
- McDermott J.D., Abrams J.S.: Techniques in Arthroscopic Rotator Cuff Repair: Single-Row Repair: The Preferred Approach. Tech Shoulder Elbow Sur. 2015;16:1-5.
- Scheibel M.T., Habermeyer P.: A modified Mason-Allen technique for rotator cuff repair using suture anchors. Arthroscopy: J Arthro Rel Sur. 2003;19:330-3
- Meyer D.C., Fucentese S.F., Koller B., et al.: Association of osteopenia of the humeral head with full-thickness rotator cuff tears. J Shoulder Elbow Sur. 2004;13:333-7
- Melis B., DeFranco M.J., Chuinard C., et al.: Natural history of fatty infiltration and atrophy of the supraspinatus muscle in rotator cuff tears. Cli Ortho Rel Res. 2010;468:1498-505
- Gulotta L.V., Nho S.J., Dodson C.C., et al.: HSS, Arthroscopic Rotator Cuff Registry. Prospective evaluation of arthroscopic rotator cuff repairs at 5 years: Part II-prognostic factors for clinical and radiographic outcomes. J Shoulder Elbow Surg. 2011;20:941-6.
- Snyder S.J., Burns J.: Rotator cuff healing and the bone marrow “crimson duvet” from clinical observations to science. Tech Shoulder Elbow Sur. 2009;10:130-7
- Milano G., Saccomanno M.F., Careri S., et al.: Efficacy of marrow-stimulating technique in arthroscopic rotator cuff repair: a prospective randomized study. Arthroscopy: J Arthro Rel Sur. 2013;29:802-10
- Cofield R.H.: Subscapular muscle transposition for repair of chronic rotator cuff tears. Sur, Gynecol Obstetric. 1982;154:667-72.
- Richards R.R., An K.N., Bigliani L.U., et al.: A standardized method for the assessment of shoulder function. J Shoulder Elbow Sur. 1994;3:347-52
- Kirkley A., Griffin S., Dainty K.: Scoring systems for the functional assessment of the shoulder. Arthroscopy: J Arthro Rel Sur. 2003;19:1109-20
- Sugaya H., Maeda K., Matsuki K., et al.: Repair integrity and functional outcome after arthroscopic double-row rotator cuff repair. J Bone Joint Sur. 2007;89-A:953-960.
- Barth J., Fotiadis E., Barthelemy R., et al.: Ultrasonic evaluation of the repair integrity can predict functional outcomes after arthroscopic double-row rotator cuff repair. Knee Sur, Sports Traumatol, Arthro. 2015;23:376-85
- Gartsman G.M.: Arthroscopic acromioplasty for lesions of the rotator cuff. J Bone Joint Sur. 1990;72:169-80.
- Ruotolo C., Nottage W.M.: Surgical and nonsurgical management of rotator cuff tears. Arthroscopy: J Arthroscopic Rel Sur. 2002;18:527-31.
- Park J.Y., Lhee S.H., Choi J.H., et al.: Comparison of the clinical outcomes of single-and double-row repairs in rotator cuff tears. Am J Sports Med. 2008;36:1310-6
- Ma H.L., Chiang E.R., Wu H.T., et al.: Clinical outcome and imaging of arthroscopic single-row and double-row rotator cuff repair: a prospective randomized trial. Arthroscopy: J Arthro Rel Sur. 2012;28:16-24
- Mazzocca A.D., Millett P.J., Guanche C.A., et al.: Arthroscopic single-row versus double-row suture anchor rotator cuff repair. Am J Sports Med. 2005;33:1861-8
- Yoshida M., Collin P., Josseaume T., et al.: Post-operative rotator cuff integrity, based on Sugaya’s classification, can reflect abduction muscle strength of the shoulder. Knee Sur Sports Traumatol Arthro. 2018;26:161-8.
- Saccomanno M.F., Cazzato G., Fodale M., et al.: Magnetic resonance imaging criteria for the assessment of the rotator cuff after repair: A systematic review. Knee Sur Sports Traumatol Arthro. 2015;23:423-42
- Ma C.B., MacGillivray J.D., Clabeaux J., et al.: Biomechanical evaluation of arthroscopic rotator cuff stitches. JBJS. 2004;86:1211-6.
- Lorbach O., Anagnostakos K., Vees J., et al.: Three-dimensional evaluation of the cyclic loading behavior of different rotator cuff reconstructions. Arthroscopy: J Arthro Rel Sur. 2010;26:S95-105
- Khalil M.H., Rashwan A.S.: Arthroscopic rotator cuff repair using modified Mason-Allen versus double row suture bridge techniques. 2018;54:49-54
- Jo C.H., Shin J.S., Park I.W., et al.: Multiple channeling improves the structural integrity of rotator cuff repair. Am J Sports Med. 2013;41:2650-7
- Jo C.H., Yoon K.S., Lee J.H., et al.: The effect of multiple channeling on the structural integrity of repaired rotator cuff. Knee Sur Sports Traumatol Arthro. 2011;19:2098-107
- Song N., Armstrong A.D., Li F., et al.: Multipotent mesenchymal stem cells from human subacromial bursa: Potential for cell based tendon tissue engineering. Tissue Engineer Part A. 2014;20:239-49
- Ahmad C.S., Stewart A.M., Izquierdo R., et al.: Tendon-bone interface motion in transosseous suture and suture anchor rotator cuff repair techniques. Am J Sports Med. 2005;33:1667-71
- Ajrawat P., Dwyer T., Almasri M., et al.: Bone marrow stimulation decreases retear rates after primary arthroscopic rotator cuff repair: a systematic review and meta-analysis. J Shoulder Elbow Sur. 2019;28:782-91
- Cho N.S., Lee B.G., Rhee Y.G.: Arthroscopic rotator cuff repair using a suture bridge technique: is the repair integrity actually maintained?. Am J Sports Med. 2011;39:2108-16.



 Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.
Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.