The functional and radiographic outcome of fixation of trimalleolar fracture: A prospective study
Received: 26-Oct-2020 Accepted Date: Nov 26, 2020 ; Published: 08-Jan-2021, DOI: 10.37532/1897-2276.2021.16(1).2
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: Ankle injuries gain importance because body weight is transmitted through it and locomotion depends upon the stability of this joint. Trimalleolar fractures are one of the most complex fractures around ankle. As with all intra articular fractures, trimalleolar fractures necessitate reduction and stable internal fixation. The purpose of this study is to assess the functional and radiographic outcome and results of surgical treatment of trimalleolar fractures by specific modalities. To attain a proper anatomical alignment and stability of ankle joint and further applying a syndesmotic screw if needed. Materials and methods: A prospective review was conducted for 28 patients between January 2018 to December 2019 with closed trimalleolar fracture. Open reduction and internal fixation were done with specific modalities. Patients were evaluated with subjective and objective assessments of the patients’ ankles were done using a modification of the scoring system proposed by Olerud and Molander and radiologically by Kristenson criteria. The functional and radiographic outcome of ORIF and advantages of the procedures were recorded. Functional and radiographic evaluations were performed at immediate post op, 6 weeks, 3 months and 6 months, 1 year after surgery. At each follow up, patients were assessed for syndesmotic reduction, loss of fixation, and implant failure and any arthritis changes. The reduction in quality was evaluated on immediate postoperative radiography. Results: In the present study of 28 patients with trimalleolar fractures treated by open reduction and internal fixation. Excellent results were achieved in 23 (82.1%) patients, good in 4 (14.3%), and poor in 1 (3.6%) patient. The patient with poor result had mild pain with activities of daily living, diminution in the abilities to run and to do work, reduced motion of ankle and narrowing of joint space. Conclusions: Operative treatment for trimalleolar fractures results in good functional and radiographic outcome postoperatively. Anatomical reduction of the fracture is associated with better functional outcome. Early treatment without delay, anatomic reduction and fracture fixation, stringent postoperative mobilization and rehabilitation should help improve outcome in an operated trimalleolar fracture.
Keywords
trimalleolar fracture, posterior malleolus fracture, plating, tension band wiring
Introduction
Sir Robert Jones said “ankle is the most injured joint of the body but the least well treated” [1]. As with all intra articular fractures, trimalleolar fractures necessitate reduction and stable internal fixation [2-4]. Ankle fracture is one of the most common lower limb fractures [5] for they account for 9% of all fractures representing a significant portion of the trauma workload [6]. Ankle fractures usually affect young men and older women, however, below the age of 50 [7]; ankle fractures are the commonest in men. Two commonly used classification systems for ankle fractures include the Danis Weber AO classification and the Lauge-Hansen classification. There are several different methods of ankle fracture fixation, however the goal of treatment remains a stable anatomic reduction of talus in the ankle mortise and correction of the fibula length as a 1 mm lateral shift of the talus in the ankle mortise reduces the contact area by 42%, and displacement (or shortening) of the fibula more than 2 mm will lead to significant increases in joint contact pressures. Further research both biomechanically and clinically needs to be undertaken in order to clarify a preferable choice of fixation. Many of the fractures which are stable are reduced by conservative treatment and have given good result. The other unstable displaced and open fractures require open reduction internal fixation. The superiority of ORIF over closed treatment has been thoroughly demonstrated in literature. However, all studies have not obtained good results in cases of trimalleolar fractures. The purpose of this study is to assess the functional and radiographic outcome and results of surgical treatment of trimalleolar fractures by specific modalities of tension band wiring of medial malleoli or screw fixation of medial malleolus, plating of lateral malleoli, and screw or plate fixation of posterior malleoli, to attain a proper anatomical alignment and stability of ankle joint and further applying a syndesmotic screw if needed.
Materials and Methods
From January 2018 to December 2019, 28 trimalleolar fractures fixation were performed using specific modalities implant. The study was conducted at Amandeep Hospital, Amritsar, Punjab after obtaining the ethical clearance from institutional ethical committee. Initial management was done in the orthopedic emergency area, which included getting standard AP and lateral radiographs of the ankle joint. Distal neurovascular status and clinical signs to exclude compartment syndrome were assessed and documented. Patients with gross ankle dislocation were attempted to be reduced in the emergency itself under sedation after prior consent from the patient and relatives. A belowknee plaster slab was applied to immobilize the joint and analgesics were instituted. The limb was kept elevated to prevent excessive swelling. After routine blood investigations and preanesthesia clearance, patients were posted for surgery. An ankle CT scan was conducted in all cases as part of the pre-operative planning. Intravenous 1 gm cefazolin was administered 30 min prior to skin incision in the operating room after prior antibiotic sensitivity testing. Patient’s age between 18 to 85 years with close trimalleolar fractures were included in this study. Patients with open fractures, active infection at site of injury or other associated fractures in the body elsewhere were excluded. Patients with severe preexisting arthritis in the affected ankle joint, limp, or assisted walk due to some previous or ongoing pathology in the hip or knee joint either in ipsilateral or in contralateral limb were excluded from the study.
Operative Methods
There are several different methods of ankle fracture fixation, however the goal of Treatment remains a stable anatomic reduction of talus in the ankle mortise and correction of the fibula length as a 1 mm lateral shift of the talus in the ankle mortise reduces the contact area by 42% [3], and displacement (or shortening) of the fibula more than 2 mm will lead to significant increases in joint contact pressures. The choice of fixing the medial or lateral side first may be guided by the surgeon’s preference, but the ankle joint in these fractures is often very unstable.
We have followed the following sequence:
1. The fibular shaft is brought out to length and fixed
2. The Volkmann’s fragment (posterior malleolus) is reduced and fixed
3. The medial fracture is fixed
4. The integrity of the syndesmosis is restored
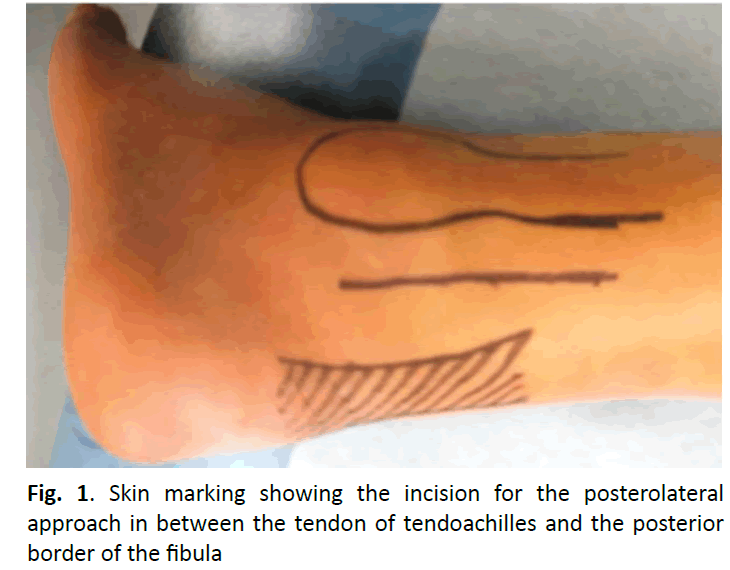
After the induction of appropriate anesthesia, the patient was first made to lie in a Semi-prone position on a radiolucent operating table. All bony prominences were well padded. The knees were slightly flexed by positioning a bolster underneath the ankles to obtain good ankle dorsiflexion for fracture reduction. A posterolateral approach was used by making an incision midway between the medial border of the fibula and the lateral border of tendoachilles (Fig. 1). The use of a pneumatic tourniquet in the initial part of our surgery was done to identify and isolate the sural nerve and lesser saphenous vein away from the surgical field. The sural nerve courses from medial to lateral part, and at a point 7 cm proximal to the tip of the lateral malleolus, the nerve is on an average 26 mm posterior to the edge of the fibula [8]. Careful soft tissue dissection and protection of the sural nerve is a must to prevent the formation of painful neuromas. The peroneal tendons were retracted further laterally and anteriorly to expose the fibula. The fibular fixation was carried out first. We provisionally fixed the fracture with K-wires and applied a 3.5 mm reconstruction plate, prebend fibular plate or one-third tubular plate in an antiglide fashion over the posterior or lateral surface of the fibula. Anatomical reduction of the lateral malleolus usually made the ankle stable and posterior malleolus reduced by itself due to ligamentotaxis by PITFL. The ankle stability was checked intraoperatively by performing a posterior drawer or posterior loading test of the foot with one hand and by stabilizing the distal leg with the other hand. In inadequate reductions or stabilization of the posterior malleolus, a talar subluxation under the distal articular surface was appreciated.
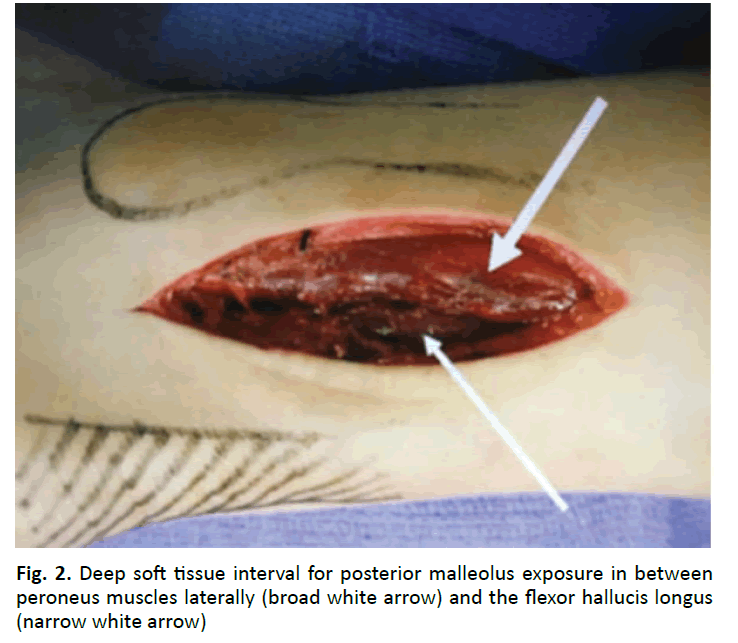
Fixation of posterior malleolus was carried out next. A deep interval between the peroneal tendons laterally and flexor hallucis longus medially (Fig. 2) was made, and soft tissue and periosteum were incised from a medial to lateral fashion to avoid injuring the PITFL. Also, care was taken not to injure posterior malleolar vessels, thereby preventing devascularization of the posterior malleolar fragments. The soft tissue, soft callus, and hematoma interposing in the fractured surfaces of the posterior malleolus were cleared with curette and saline irrigation. This was possible by a slight book opening technique in a craniocaudal direction of the posterior malleolus. This is achieved prior to fixation of the lateral malleolus since once stabilized by PITFL in its place the posterior malleolus is comparatively difficult to maneuver. The posterior malleolus was buttressed with a 3.5 mm recon plate, distal radius T-pate, or one-third tubular plate. The fibular translation test was then performed to check for the stability of the syndesmosis and, in none of the cases, we found syndesmosis to be unstable. No syndesmotic fixation was carried out in any of our cases. The posterolateral wound was irrigated, adequate hemostasis was achieved, and closure was performed. The second part of the surgery included fixation of the medial malleolus. An anteromedial approach was used to expose the medial malleolus, carefully protecting the great saphenous vein. The interposing periosteum was excised and fixation achieved with two 4 mm partially threaded cannulated screws or tension band wiring. The patient was subsequently discharged after a dressing change at 48 hours post-surgery. A below-knee plaster was maintained until 2 weeks postoperatively till Stitch removal. A strict non weight-bearing and ankle Range of Motion (ROM) exercises protocol was maintained until 6 weeks post-surgery. Follow-up at 6 weeks was done when radiographs of the ankle joint were repeated and partial weight-bearing with the help of walking aids was initiated. Regular monthly follow-ups were conducted. Full weight bearing was started once the clinical and radiological union was achieved. Ankle score, according to Olerud and Molander (Table 1), and ankle arthritis with weight bearing X-rays at 12 months of follow-up were documented in all cases [9,10].
| Parameter | Degree | Score |
|---|---|---|
| Pain | None | 25 |
| While walking on uneven surface | 20 | |
| While walking on even surface outdoors | 10 | |
| While walking indoors constant and severe | 5 | |
| Stiffness | None | 0 |
| Stiffness | 10 | |
| Swelling | None | 0 |
| Only in evenings | 10 | |
| Constant | 5 | |
| Stair-climbing | No problems | 0 |
| Impaired | 5 | |
| Impossible | 0 | |
| Running | Possible | 5 |
| Impossible | 0 | |
| Jumping | Possible | 5 |
| Impossible | 0 | |
| Squatting | No problems | 5 |
| Impossible | 0 | |
| Supports | None | 10 |
| Taping, Wrapping | 5 | |
| Stick or crutch | 0 | |
| Work, activities of daily life | Same as before injury | 20 |
| Loss of tempo | 15 | |
| Change to similar job | 15 | |
| Severely impaired work capacity | 0 |
A score of 90 to 100 is considered Excellent; 70 to 89- Good; 50 to 69 points- Fair and less than 50 is considered Poor.
Table 1. Scoring system devised by Olerud and Molendar (maximum 100 points).
Post-operative antibiotics were continued for a period ranging from 3 to 5 days depending on the presence of other injuries and therapy was prolonged if there were signs of infection. Once pain-free, patient was trained in non-weight bearing crutch walking and advised dorsiflexion and plantarflexion exercises.
Postoperative, assessment was done immediately then 6 weeks, 3 months, 6 months and 1 year according to Olerud and Molander functional scoring. Fractures were classified according to the Lauge- Hansen system and operated within 24 hours of presentation. Subjective and objective assessments of the patient’s ankles were done using a modification of the scoring system proposed by Olerud and Molander [9]. Patients were evaluated radiologically by Kristenson criteria [11] (Table 2).
| S. No. | Good |
|---|---|
| 1. | Talus-correctly placed |
| 2. | Medial malleolus-no displacement or fracture gap of less than 2 mm |
| 3. | Lateral malleolus-negligible lateral displacement and up to 2 mm of posterior displacement |
| 4. | Posterior malleolus-upward displacement of less than 2 mm |
| Fair | |
| 1. | Talus-correctly placed |
| 2. | Medial malleolus-no displacement or fracture gap of less than 2 mm |
| 3. | Lateral malleolus-negligible lateral displacement and up to 2 mm of posterior displacement |
| 4. | Posterior malleolus-upward displacement of less than 2 mm |
| Poor | |
| 1. | Talus-correctly placed |
| 2. | Medial malleolus-no displacement or fracture gap of less than 2 mm |
| 3. | Lateral malleolus-negligible lateral displacement and up to 2 mm of posterior displacement |
| 4. | Posterior malleolus-upward displacement of less than 2 mm |
Table 2: Kristenson’s criteria[11].
Postoperatively complications including non-union, delayed union, infection, implant failure, per-implant fracture, and Post traumatic arthritis were recorded.
Results
In our series, most of the patient affected by the fracture belongs to age group of 20-50 years, which were 15 (53.6%). The commonest mode of injury is road traffic accident (67.9%) and fall (32.1%). 12 were male patients (42.9%) and 16 were female patients (57.1%). 15 cases involved the right ankle and 13 cases involved the left ankle. The most common injury pattern seen was supination external rotation 19 patients (67.9%). In the present study group, 19 cases (67.9%) had a stay of more than 5 days while 9 cases (32.1%) had a stay of less than or equal to 5 days. The mean duration of stay was 4.9 days. Surgical technique used were open reduction and internal fixation of the lateral malleolus with semi tubular plate or recon plate; medial malleolus with cancellous screws or tension band wiring; posterior malleolus with cancellous screws or plate.
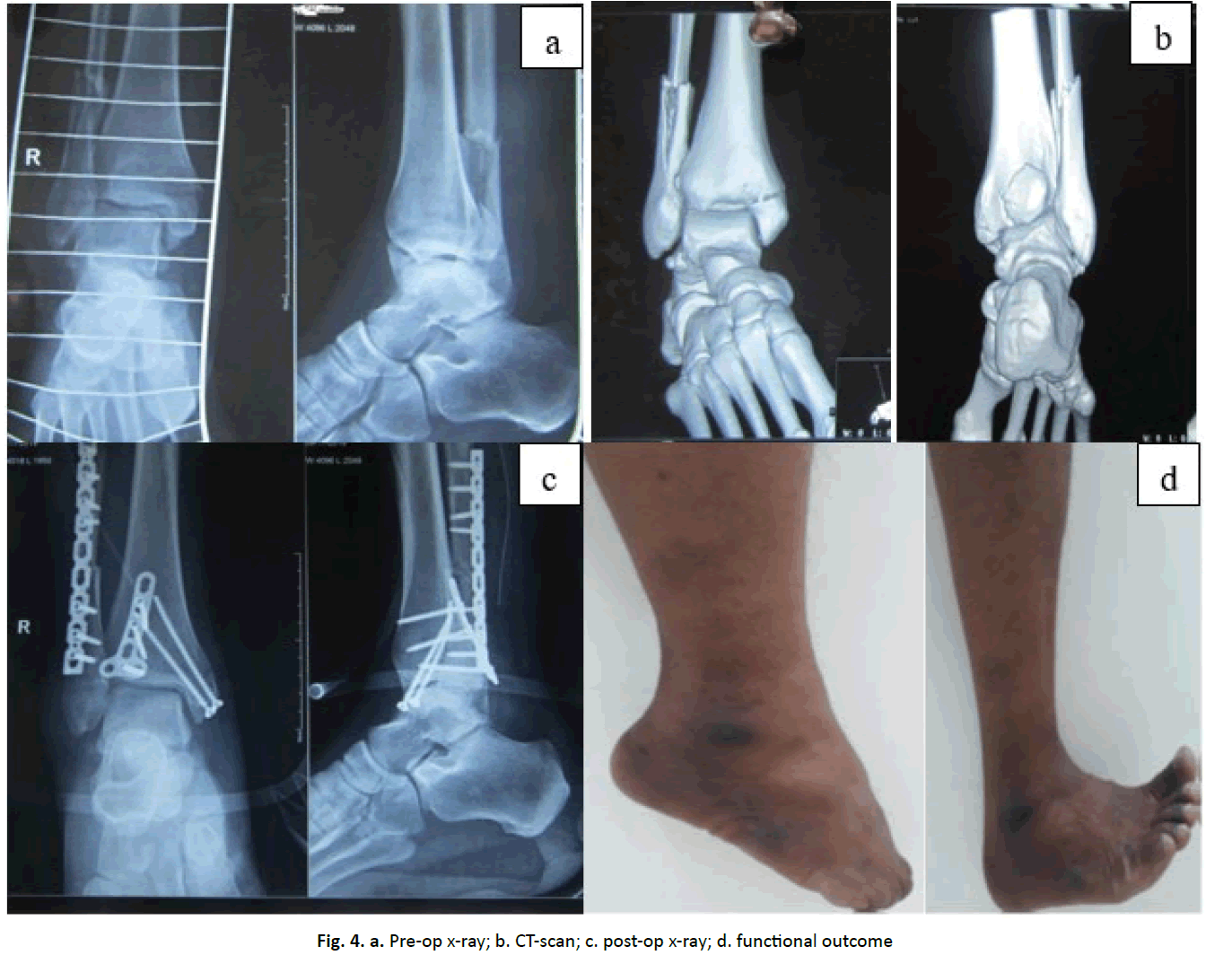
In the present study out of 28 patients, 2 patients presented with persistent swelling, 5 patients presented with residual pain while 7 patients presented with both of the complaints. In our study of 28 cases, 23 cases (82.1%) achieved excellent results and 4 cases (14.3%) achieved good results at 12 months follow up. No significant wound complications were noted. Operative treatment for ankle fractures results in good functional outcome post- operatively (Fig. 4). Anatomical reduction of the fracture was associated with better functional and radiological outcomes. Early management with guided weight bearing ensures good functional outcome.
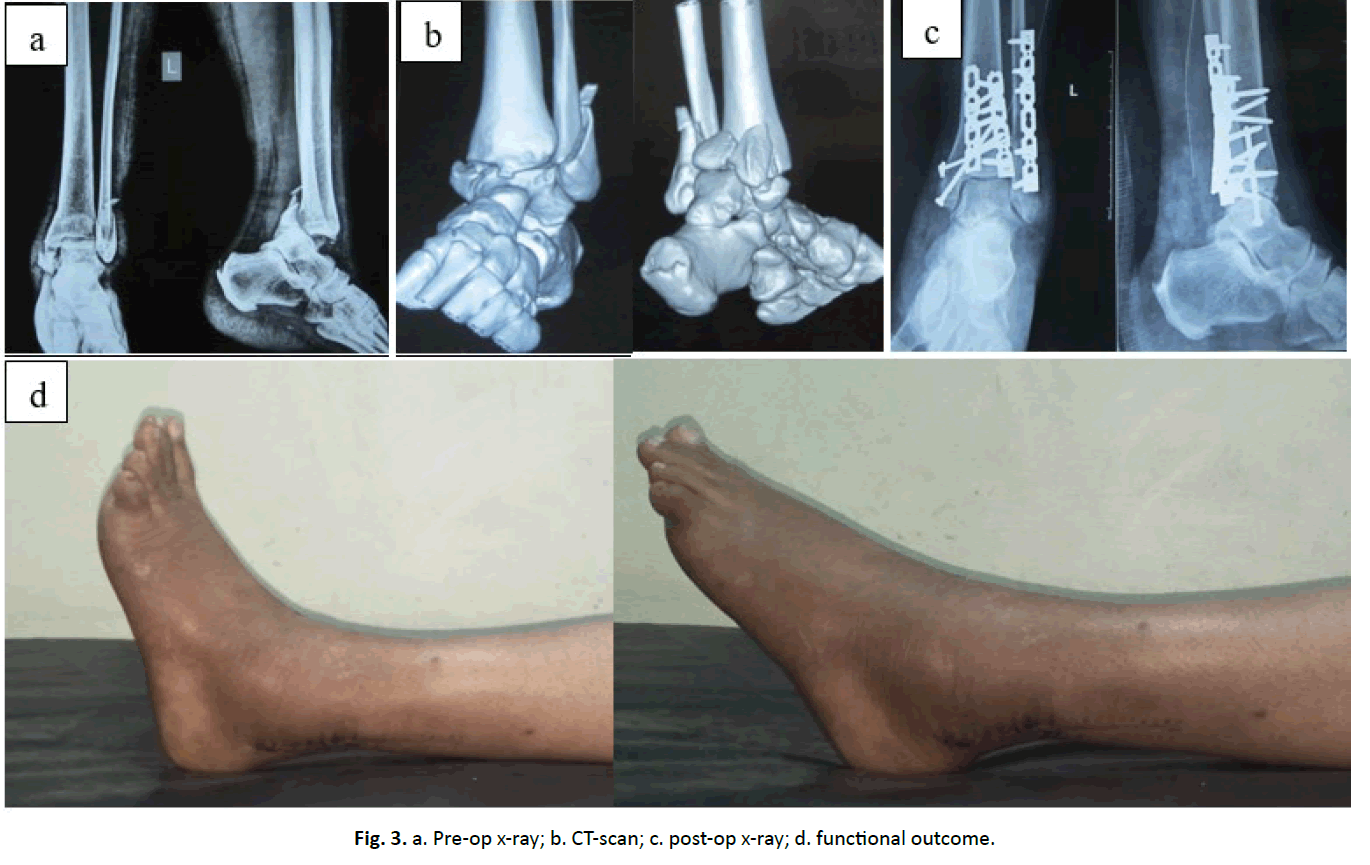
The average time to union and full weight bearing was 12.85 weeks (range 10-16 weeks). The average percentage of the restoration of ROM as compared to the contralateral ankle at the time of union was 90.2% of dorsiflexion, 91.8% of plantar flexion, 88.1% of inversion, and 85.1% of eversion. An excellent outcome in 23 patients and good outcome in 4 patients at the end of 12 months follow-up were concluded according to the Olerud and Molendar scoring system [9] (Table 1). Bargon criteria [10] for grading post-traumatic arthritis of the ankle joint at the end of 12 months with the help of weight-bearing ankle x-rays were assessed (Fig. 3). Only one patient had grade 2 arthritis, four patients had grade 1, while the rest had grade 0 arthritis. No complications related to soft tissue healing, pain, or hardware impingement or breakages were encountered.
Discussion
In the present study, the most common fracture pattern seen was supination-external rotation type of injury 19 cases (67.9%) followed by pronation external rotation type of injury 5 cases (17.9%). Studies by Weening et al. [12] in 2005, of about 425 ankle fractures demonstrated 30% of fractures to be due to supination external rotation type of injury. The least common being pronation dorsiflexion type of injury. The most common modality of fixation for the lateral malleolus and posterior malleolus were recon plate and for the medial malleolus was with 4 mm cannulated cancellous screws or tension band wiring. Syndesmotic screws were not used in any of the cases. Kortekangas et al. in 2014 in their study compared the functional and radiologic results of syndesmotic transfixation with no fixation in supination external rotation ankle fractures and found no significant difference in functional outcome or radiologic findings after a minimum follow up of 4 years [13].
On follow up at 6 weeks, 7 out of 28 patients had persistent swelling and residual pain, 5 patients had only residual pain and 2 patients had only persistent swelling. This is in concordance with a similar study done by Hong et al. [14] in 2014 in which he reported residual pain, swelling and ankle stiffness as the most common complications at 1 year follow up. The mean Olerud and Molendar score at 3-month post operation was 46.60, 6th month post operation was 80.17 and at 1-year post operation was 94.82. There was a statistically significant improvement in the scores from 3rd month to 6th month post-operation (p value 0.001). In our study total 23 patients had total score between 90-100, 4 patients had score between 75-89 and only 1 patient had score less than 75 which is comparable to previous study. Hong et al. in 2013 evaluated the functional outcome and limitation of sporting activities after trimalleolar ankle fractures. At 1 year follow up most patients gained good function and had good to excellent Olreud and Molander scores. However, out of the 47 patients, 26 (55.3%) had residual pain, 29 (61.7%) complained of stiffness and 21 (44.7%) had ankle swelling. Of the 33 (70.2%) patients who were involved in sporting activities prior to the ankle injury, 9 (27.3%) were able to return to pre injury level of sporting activities with no difficulties [15].
According to Kristenson’s radiological criteria out of 28; 23 (82.1%) patients have good result, 4 (14.3%) patients have fair result and 1 (3.6%) patient has poor result. Similarly, Khandelwal et al. [16] in their study recorded good result in 85% patients and fair result in 15% patients who were treated operatively.
There are several limitations of our study. The results of this study may be limited by measurement error. The physical measurements may be subject to both, observer’s errors and patient variability. Observer’s errors can arise from inconsistencies during the recording and reporting of measurements, including; variations in the placement of equipment. The study was conducted by a single observer hence there was no inter-observer bias. Patient variations however, may arise from the patient altering their effort or position when performing the physical assessments, or by reporting a better or worse functional score in response to external influences unrelated to their ankle at the time of completing the score.
The study is also limited to patients having surgical fixation for their fracture. These results therefore, cannot necessarily be compared to the outcome achieved with non-operative management or other modalities of treatment.
Conclusion
Operative treatment for trimalleolar fractures results in good functional and radiographic outcome postoperatively. Anatomical reduction of the fracture is associated with better functional outcome. Early treatment without delay, anatomic reduction and fracture fixation, stringent postoperative mobilization and rehabilitation should help improve outcome in an operated trimalleolar fracturet.
REFERENCES
- Shelton Marvin L.: Complication of fractures and dislocation of the ankle. In: Complications in orthopaedic surgery, Chapter 23, 3rd edn, Vol. 1, edt. EPPS, Charles H., Philadelphia: J.B. Lippincott Company. 1994;595-648.
- Beris A.E., Kabbani K.T., Xenakis T.A., et al.: Surgical treatment of malleolar fractures-a review of 144 patients. Clin Orthop Rel Res. 1997;341:90-98.
- Weber M.J.: Ankle fractures and dislocations. In: Operative Orthopaedics, Chapter-50, 2nd edn., Vol. 3, Ed. Chapman M.W., Madison M. Philadelphia: J.B. Lippincott Company. 1993;731-748.
- Baird R.A., Jackson S.T.: Fracture of the distal part of fibula with associated disruption of the deltoid ligament. J Bone Joint Surg. 1987;69A:1346-1352.
- Lash N., Horne G., Fielden J., et al.: Ankle Fractures: Functional and Lifestyle Outcomes at 2 Years. ANZ J Surg. 2002;72:724-730.
- Court-Brown C.M. Caesar. B.: Epidemiology of adult fractures: a review. Injury. 2006;37:691-697.
- Bugler K.E., White T.O., Thordarson D.B.: Focus on ankle fractures. J Bone Joint Surg. 2012;94:1107-1112.
- Lawrence S.J., Botte M.J.: The sural nerve in the foot and ankle: an anatomic study with clinical and surgical implications. Foot Ankle Int. 1994;15:490-494.
- Olerud C., Molander H.: A scoring scale for symptom evaluation after ankle fracture. Arch Orthop Trauma Surg. 1984;103:190-194.
- Bargon G.: X-ray morphological grading of post-traumatic arthrosis in the upper ankle joint. Hefte Unfallheilkd. 1978;133:28-34.
- Joy G., Patzakis M.J., Harvey J.P.: Precise evaluation of the reduction of severe ankle fractures. J Bone Joint Surg Am. 1974;56:979-93.
- Weening B., Bhandary M.: Predictors of functional outcome following transsyndesmotic screw fixation of ankle fractures. J Orthop Trauma. 2005;19:102-108.
- Kortenkangas T.H., Pakarinen H.J., Savola O., et al.: Syndesmotic fixation in supination-external rotation ankle fractures: a prospective randomised study. Foot Ankle Int. 2014;35:988-995.
- Hong C.C., Nashi N., Prasad R.S.: Impact of trimalleolar ankle fractures: how do patients fare post operatively? Foot Ankle Surg. 2014;20:48-51.
- Hong C.C., Roy S.P., Nashi N., et al.: Functional outcome and limitation of sporting activities after bimalleolar and trimalleolar ankle fractures. Foot Ankle Int. 2013;34:805-810.
- Kandelwal H., Rakesh S., Joshi P.S., et al.: Comparative study of conservative and surgical treatment of ankle fractures. Natl J Integr Res Med. 2015;6.



 Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.
Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.