The Hindfoot Nail Entry Point
2 Professor, Chief of Orthopedics, Department of Orthopedics & Surgery, University of Louisville Hospital, Louisville, Kentucky, USA
3 Orthopedic Surgery Resident, Department of Orthopedics, Surgery, University of Louisville Hospital, Louisville, Kentucky, USA
4 Podiatry resident, University of Louisville Hospital, Louisville, Kentucky, USA
5 Orthopedic Surgery Fellow, Department of Orthopedic Surgery, Harborview Medical Center/University of Washington, Seattle, Washington, USA, Email: david.seligson@louisville.edu
6 Associate Professor, Department of Orthopedic Surgery, Harborview Medical Center/University of Washington, Seattle, Washington, USA
Received: 12-Mar-2023, Manuscript No. jotsrr-23-91385; Editor assigned: 14-Mar-2023, Pre QC No. jotsrr-23-91385 (PQ); Accepted Date: Mar 27, 2023 ; Reviewed: 24-Mar-2023 QC No. jotsrr-23-91385 (Q); Revised: 26-Mar-2023, Manuscript No. jotsrr-23-91385 (R); Published: 28-Mar-2023
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: Tibiotalocalcaneal arthrodesis is a procedure for pain relief and deformity correction by creating a rigid fusion of tibiotalar and subtalar joints. Hindfoot nails have been identified as one of the most common current methods used in the procedure. Establishing the correct entry point for a hindfoot nail is critical to ensure acceptable hindfoot alignment which is physiologically known to be associated with valgus. Our research aims to use a cadaveric model to assess the anatomic angle to be considered in potential hindfoot nails.
Materials and methods: 6 fresh-frozen transtibial amputated cadaveric specimens, with no known prior deformity, surgical intervention, or trauma, were evaluated. Two 6.5-mm guide pins were advanced in antegrade and retrograde directions till a point of intersection was detected by fluoroscopy. The hindfoot angle was measured in every specimen.
Results: The hindfoot angle, in degrees, for each of the six cadaveric specimens was as follows: 7.1, 6.8, 5.3, 10.1, 6.3, and 8.1. The mean hindfoot angle for the six specimens was 7.3 +/- 1.6 degrees.
Conclusion: Our analysis shows that a hindfoot nail with approximately 7.3 degrees of valgus will enhance positioning of the nail inside calcaneus, talus, and distal tibia. This angle permits axial loading through the nail which is the most biomechanically stable structure.
References
Biotechnology Article Blog | Auto Insurance in Illinois Computer Technologies Articles Blog | Car Insurance in Washington and Georgia Blog | Cordblood Journals Electronic Technologies Articles Blog | Dental Care Journals Emerging Technologies Articles Blog | Best Betting Sites in Italy Environmental Technologies Articles Blog | Car Insurance in Texas Medical Technologies Articles Blog | Casino Sites in Italy Micro Technologies Articles Blog - Find Lawyer in Oklahoma Military Technologies Articles Blog - Find Lawyer in South Carolina Nano Technologies Articles Blog | Best Betting Sites in Argentina Nft Technologies ArticlesKeywords
Tibiotalocalcaneal arthrodesis, Cadaveric, Hindfoot alignment, Hindfoot nail, Hindfoot angle, Arthrodesis, Retrograde intramedullary nail
Introduction
Tibiotalocalcaneal Arthrodesis (TTCA) is a procedure of pain relief and deformity correction by creating a rigid fusion of tibiotalar and subtalar joints [1]. It can be used as the primary treatment for complex hindfoot fractures or ankle fractures in the elderly and those with multiple comorbidities [2]. It can also be used in the treatment of failed arthrodesis, necrosis of the talus, post-traumatic arthritis, fracture malunion or nonunion, Charcot arthropathy, and comminuted distal tibial fractures in diabetic and morbidly obese patients [3,4]. Furthermore, it can be a useful pain-relieving procedure for many patients who have severe pain or ankle deformities.
While the literature has identified many methods of TTCA, the most common current methods include the use of crossed cancellous bone screws, plates, or a hindfoot retrograde intramedullary nail [5]. Establishing the correct entry point for a hindfoot nail is critical to ensure acceptable alignment of tibiotalar and subtalar joints. Classically, hindfoot alignment was determined using a long axial or hindfoot alignment view [6]. Studies in the general population using these radiographic methods in normal asymptomatic feet record values between 2 and 5 degrees of valgus [7]. Clinical measurements of the hindfoot alignment, through measuring the standing tibiocalcaneal angle (STCA), range between 5.61 and 6.50 degrees of valgus [8]. These results suggest that the hindfoot is physiologically associated with valgus [9]. This implies that an entry point, located more medially in the calcaneus, is required to restore normal alignment, and allow true axial loading through the limb [10].
However, one must be careful of critical structures that lie on the medial side of the hindfoot that can be injured during nail entry including, but not limited to, lateral plantar neurovascular bundle, posterior tibial artery, tibial nerve, posterior tibial tendon, flexor hallucis longus tendon, and flexor digitorum longus tendons [11]. Moreover, an inappropriate entry point of the nail can cause technical failure, including malalignment and peri-implant fracture.
However, to our knowledge, no anatomic studies have focused on determining the optimal anatomic angle of the nail that is needed to match the native valgus of the hindfoot. Our primary aim was to use a cadaveric model to determine the anatomic angle that should be considered in potential hindfoot nails.
Materials and Methods
In January 2018, at the orthopedic department in our university hospital, and following our Institutional Review Board (IRB) approval of the study, six fresh-frozen transtibial amputated cadaveric specimens were evaluated. All cadavers had no known prior deformity, surgical intervention, or trauma.
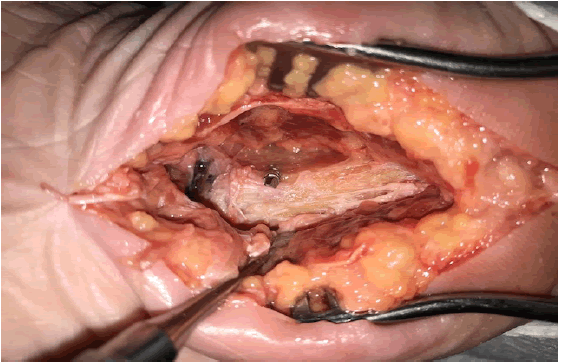
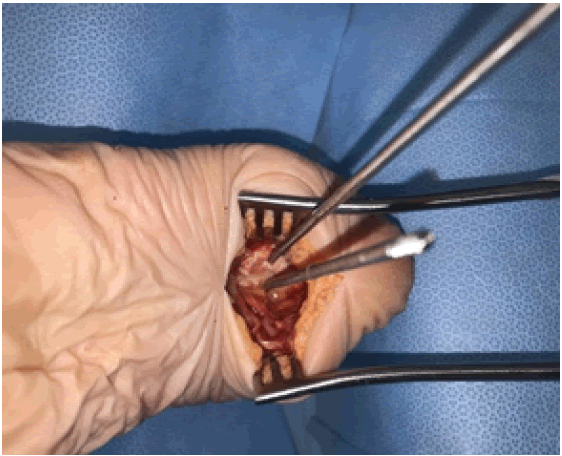
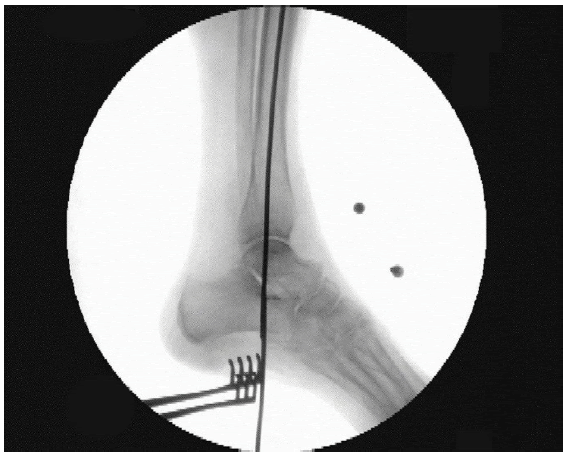
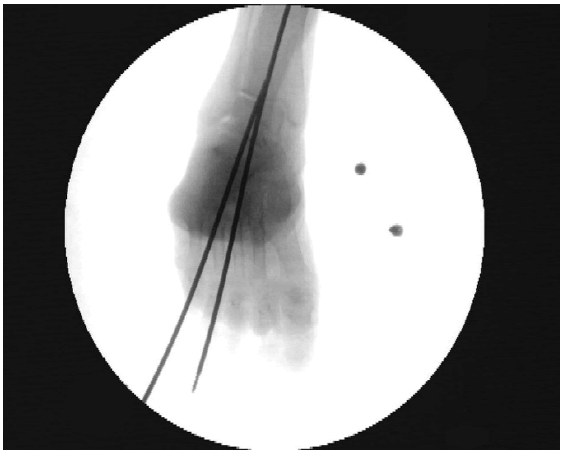
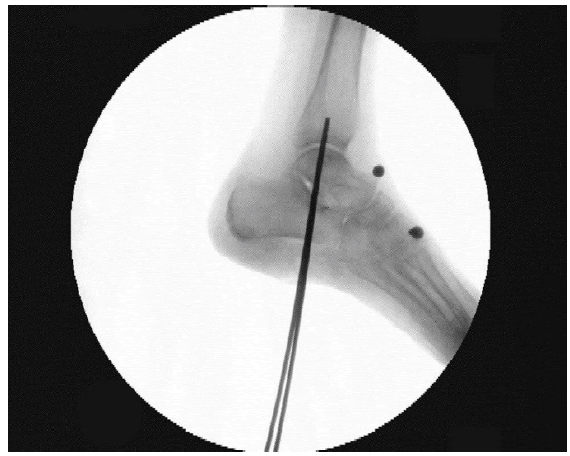
A three-centimeter midline incision was made on the hindfoot’s plantar aspect and adequate dissection was made to the calcaneus via the plantar fascia. The calcaneus’ medial and lateral boundaries were exposed. 26.5-mm guide pins were prepared. The first guide pin was placed proximally in the center of the tibial intramedullary canal and advanced distally through tibial plafond, talus, calcaneus, plantar fascia, and skin (Fig.1). The second guide pin was located on the axial center point of the calcaneus and advanced proximally through calcaneus, talus, and tibial plafond (Fig. 2). The two pins were advanced in opposite directions till a point of intersection was detected using different fluoroscopy images (Fig. 3-5). These images were then printed, and a goniometer was used to measure the angle between the two pins. This angle was deemed the native valgus of the hindfoot.
Results
We studied 6 fresh-frozen cadaveric specimens (3 female and 3 male cadavers, aged between 47 years and 70 years, with a mean of 58.5 years). The hindfoot angle, in degrees, for each of the 6 cadaveric specimens was as follows: 7.1, 6.8, 5.3, 10.1, 6.3, and 8.1. The mean hindfoot angle for the six specimens was 7.3 +/- 1.6 degrees.
Discussion
The hindfoot arthrodesis nail has been established as a useful tool for treatment of multiple orthopedic pathologies. Its use allows for early weight-bearing and provides minimal insult to soft tissues, which can be key in elderly patients or those with multiple comorbidities.
Clinical evaluation and previous studies have suggested that there is a certain amount of valgus in the native hindfoot [6-8]. It is important that this be taken into consideration when establishing the entry point for placing a hindfoot nail. Current hindfoot nails available for implantation are either straight or valgus-curved. Historically, straight retrograde intramedullary nails have been associated with many complications, such as plantar neurovascular damage, poor alignment of the hindfoot and stress reactions, particularly in the tibial isthmus region [11-15]. Those complications have significantly limited the clinical use of straight retrograde nails to conduct TTCA [16].
Valgus-curved retrograde intramedullary nails have been designed to overcome the aforementioned shortcomings associated with straight nails [16]. Castro et al. discussed the overall importance of using a nail with a valgus curve in TTCA to allow the nail to be inserted centrally in the calcaneus and subsequently into the medullary canal of the tibia [17]. Fang et al. concluded that TTCA using a short, retrograde, valguscurved intramedullary nail is an effective technique for achieving solid fusion and good hindfoot alignment in patients with serious hindfoot disorders [16]. McKenzie et al. compared bone contact surface in the calcaneus between straight and valgus-curved hindfoot nails. They found that the latter had significantly more bone contact surface area than the former [18]. Callahan et al. mentioned that a valgus-curved nail will provide increased distance from structures at risk, namely the lateral plantar nerve, by moving the point laterally [19, 20].
Conclusion
That said, evidence showed that valgus-curved hindfoot nails were more beneficial and anatomy respecting than straight nails. But no studies have been done to confirm that the available nails with 5 degrees of valgus are adequate. Our study demonstrates that, on average, a hindfoot nail with approximately 7.3 degrees of valgus would result in better nail positioning within calcaneus, talus, and distal tibia. This angle allows for axial loading through the nail, which is the most biomechanically stable construct.
References
- Quill GE. The use of a second-generation intramedullary nail in the fixation of difficult ankle and hindfoot arthrodesis. Am J Orthop. 1999;1:23-31. [Google Scholar] [CrossRef]
- Taylor BC, Hansen DC, Harrison R, et al. Primary retrograde tibiotalocalcaneal nailing for fragility ankle fractures. Iowa Orthop. J. 2016;36:75. [Google Scholar] [CrossRef]
- Kuhn S, Appelmann P, Mehler D, et al. Retrograde tibial nailing: a minimally invasive and biomechanically superior alternative to angle-stable plate osteosynthesis in distal tibia fractures. J. orthop. surg. res. 2014;9(1):1-8. [Google Scholar] [CrossRef]
- Massari L, Gildone A, Zerbinati F. Tibiotalocalcaneal arthrodesis by retrograde intramedullary nailing as a ‘salvage procedure’: clinical, radiographic and baropodometric evaluation of three cases. Foot ankle surg. 2002 ;8(1):3-12. [Google Scholar] [CrossRef]
- Bennett GL, Cameron B, Njus G. Tibiotalocalcaneal arthrodesis: a biomechanical assessment of stability. Foot ankle int. 2005;26(7):530-6. [Google Scholar] [CrossRef]
- Ostendorf B, Mattes-György K, Reichelt DC, et al Early detection of bony alterations in rheumatoid and erosive arthritis of finger joints with high-resolution single photon emission computed tomography, and differentiation between them. Skelet. radiol. 2010 ;39:55-61. [Google Scholar] [CrossRef]
- Strash WW, Berardo P. Radiographic assessment of the hindfoot and ankle. Clin. Podiatr. Med. Surg. 2004 ;21(3):295-304. [Google Scholar] [CrossRef]
- Haight HJ, Dahm DL, Smith J, et al. Measuring standing hindfoot alignment: reliability of goniometric and visual measurements. Arch. phys. med. rehabil. 2005 ;86(3):571-5. [Google Scholar] [CrossRef]
- Caixeta TB, Calábria Júnior MO, Castro RV, et al. Tibiotalocalcaneal arthrodesis with retrograde intramedullary nailing: 29 patients' clinical and functional evaluation. Rev. Bras. Ortop. 2014;49:56-61. [Google Scholar] [CrossRef]
- Kuhn S, Appelmann P, Pairon P, et al. Retrograde tibial nail: Anatomical implantation and surgical feasibility study. Acta Chir Ortho Trauma Cech. 2015 ;82:203-8. [Google Scholar] [CrossRef]
- Mückley T, Ullm S, Petrovitch A, et al. Comparison of two intramedullary nails for tibiotalocalcaneal fusion: anatomic and radiographic considerations. Foot ankle int. 2007;28(5):605-13. [Google Scholar] [CrossRef]
- Chou LB, Mann RA, Yaszay B, et al. Tibiotalocalcaneal arthrodesis. Foot ankle int. 2000;21(10):804-8. [Google Scholar] [CrossRef]
- Thordarson DB, Chang D. Stress fractures and tibial cortical hypertrophy after tibiotalocalcaneal arthrodesis with an intramedullary nail. Foot ankle int. 1999;20(8):497-500. [Google Scholar] [CrossRef]
- Anderson T, Linder L, Rydholm U, et al. Tibio-talocalcaneal arthrodesis as a primary proce-dure using a retrograde intramedullary nail: A retrospective study of 26 patients with rheumatoid arthritis. Acta orthop. 2005 ;76(4):580-7. [Google Scholar] [CrossRef]
- Goebel M, Mckley T, Gerdesmeyer L, Militz M, Bhren V. Die kombinierte Kompressionsmarknagelarthrodese von OSG und USG. Unfallchirurg. 2003;8(106):633-41. [Google Scholar] [CrossRef]
- Franceschi F, Franceschetti E, Torre G, et al. Tibiotalocalcaneal arthrodesis using an intramedullary nail: a systematic review. Knee Surg. Sports Traumatol. Arthrosc. 2016;24:1316-25. [Google Scholar] [CrossRef]
- Castro M, Winson IG, Grujic L, et al. Advancing technology: the hindfoot arthrodesis nail. AO Dialogue. 2009;1(09):26-28 [Google Scholar] [Cross ref]
- McKenzie S, Molina D, Morris RP, et al. Bone Contact of a Straight versus an Angled Tibiotalocalcaneal Arthrodesis Intramedullary Nail. [Google Scholar] [CrossRef]
- Callahan R, Juliano P, Aydogan U, et al. Avoiding pitfalls of tibiotalocalcaneal nail malposition with internal rotation axial heel view. Foot Ankle Spec. 2018;11(6):543-7. [Google Scholar] [CrossRef]
- Moorjani N, Buckingham R, Winson I. Optimal insertion site for intramedullary nails during combined ankle and subtalar arthrodesis. Foot ankle surg. 1998;4(1):21-6. [Google Scholar] [CrossRef]



 Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.
Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.