The timeliness of ankle fracture management from presentation to discharge; our experience from a district general hospital
2 Foundation Year 2 Doctor, Heartlands Hospital, Birmingham, United Kingdom
3 Trauma and Orthopaedic Consultant Surgeon, Heartlands Hospital, Birmingham, United Kingdom
Received: 02-May-2018 Accepted Date: Sep 14, 2018 ; Published: 20-Sep-2018
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Introduction: Unstable ankle fractures are a common presentation and operative intervention has proven to improve patient outcomes. Each stage of patient management can have an impact on patient length of stay and clinical outcome. Materials and Methods: From April 2017 to December 2017, we retrospectively analysed the data of 49 patients with a diagnosis of an unstable ankle fracture. The patient journey was assessed from presentation to the ED right through to discharge. Post-operative notes were also reviewed. Data was obtained through our Trauma Audit and Research Network (TARN). Results: 49 patients had surgical fixation for their ankle fracture. Whilst in the ED, less than 50% of the patients had a radiographic diagnosis of an ankle fracture within 30 minutes of arrival. 25 patients were admitted to the ward within 4 hours, with some patients having to wait more than 9 hours.27 patients (more than 50%) had their surgery within 2 days after being admitted, in comparison to 6 patients who had to wait more than 6 days for their operation. The former were found to have shorter hospital length of stay post-operatively. 47 out of the 49 patients were given chemical thromboprophylaxis, all patients were advised to not weight bear for a minimum of 6 weeks, and no post-operative morbidity or mortality was encountered. Conclusion: Ankle fracture fixation, sooner rather than later, does reduce post-operative hospital LOS. There is evidence to support no added benefit to post-operative chemical thromboprohylaxis, in low risk patients, and is something we should consider
Keywords
Ankle fracture, Surgery, Waiting times, Length of stay,Thromboprophylaxis
Introduction
Ankle fractures are relatively common and carry with them the potential for significant morbidity if not managed appropriately. We see a bimodal distribution of these types of injuries, ranging from young active patients, sustaining high energy trauma to elderly patients often with multiple comorbidities [1] They are the second most common trauma presentation of the lower limb [2] with a yearly incidence of approximately 187 per 100,000 [3].
Following surgical intervention for ankle fracture management, patients are at risk of developing post-traumatic osteoarthritis which can seriously impact their quality of life and potentially leave them with impaired function. For certain patients, these risks are slightly increased. Elderly people especially, can be at risk of developing wound complications, infection and failure of fixation. In the most severe cases, this can lead to amputation and even mortality [1].
Over recent years there has been a swing in the pendulum, and close contact casting has offered us a non-invasive option for managing ankle fractures in patients who may otherwise be at risk following operative intervention. However, even with this option, surgery still plays a key role in the management of unstable ankle fractures.
In this study we reviewed the patient journey from initial presentation right through to their post-operative period, within our district general hospital. The aim of doing this was to assess how well we perform at these different levels of care, whilst also being able to identify areas for improvement and change.
Materials and Methods
This is a retrospective cohort study of ankle fractures managed by Open Reduction And Internal Fixation (ORIF) in our unit. The data was collected through our Trauma Audit and Research Network (TARN) database. The individual datasets were then analyzed and data collected. Ankle fractures which were open and/or intraarticular were excluded from this study. Also excluded were polytrauma patients and patients deemed to have a stable ankle fracture (not requiring surgical intervention). Over a 9 month period (April 2017 to December 2017) we had a total of 49 patients with an unstable ankle fracture that underwent open reduction and internal fixation of their. In addition to this we also reviewed the medical notes for these patients as well as their operative notes.
Results
Demographics
From the 49 patients, 23 (47%) patients were male and 26 patients (53%) female. 22 patients (45%) were younger than 40, and of the remainder, 15 (31%) were greater than 56 years old. Tables 1 and 2 demonstrate these results.
| Gender | No. of patients |
|---|---|
| Male | 23 (47%) |
| Female | 26 (53%) |
Table 1: Distribution of male: female patients.
| Age Range | No. of patients |
|---|---|
| <25 | 11 (22%) |
| 26-40 | 11 (22%) |
| 41-55 | 12 (25%) |
| >56 | 15 (31%) |
Table 2: Age range of ankle fracture patients.
Time to Diagnostic X-Ray
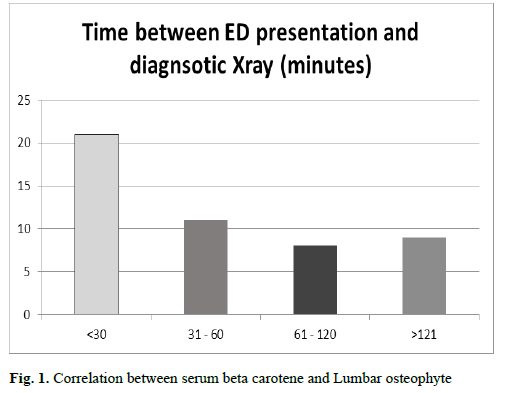
Whilst in the Emergency Department (ED), for 21 patients (43%), it took less than 30 minutes for them to have a diagnostic X-ray. 32 patients (65%) had their X-ray within the first hour of arriving to ED. And for 9 patients, it took more than 2 hours for them to have had their diagnostic X-ray. These findings are demonstrated in Fig. 1.
Time Between X-Ray and Ward Admission
There were 46 patients in total that were admitted to the trauma and orthopedic ward from ED. The remaining 3 patients from our cohort were discharged from ED and were later contacted with a date to come in for their surgery. More than half of this group (25 patients, 55%) arrived to the ward within 4 hours after presenting to ED. The remaining 21 patients were in the ED for more than 4 hours before being moved to the ward – and for 5 patients this wait before being admitted went on for more than 9 hours. Table 3 demonstrates these findings.
| Time between X-ray to ward admission (hours) | No of patients |
|---|---|
| 1 – 4 | 25 |
| 4 – 6 | 9 |
| 6 – 9 | 7 |
| >9 | 5 |
Table 3: The length of time between having had a diagnostic X-ray and being admitted to the ward.
Time to Surgery
From arriving to the ward, 27 patients (55%) had surgery within 2 days. Of them, 16 (59%) were below the age of 40. Of the remaining 11 patients that underwent surgery within 2 days, 5 (19%) were between 41 and 55 years of age, whilst the outstanding 6 patients (22%) were over the age of 56.
6 patients (12%) had their surgery beyond 6 days; and half of these were patients who were not admitted to the ward, rather they were discharged from ED and later contacted with a date to come in for their planned ankle surgery, as demonstrated in Table 4.
| Age (years) | |||||
|---|---|---|---|---|---|
| Time to Surgery (days) | <25 | 26-40 | 41-55 | >56 | Total |
| 0-2 | 9 | 7 | 5 | 6 | 27 |
| 3-5 | 1 | 2 | 5 | 8 | 16 |
| >6 | 1 | 2 | 2 | 1 | 6 |
Table 4: Variation in time to theatre and correlation with patient age.
Age v/s Length of Stay (Los)
Following the patients’ surgery, we looked at how many days these patients were in hospital before being discharged, either home or to a rehabilitation facility. We categorized the patient LOS as early (between 0-2 days post op), middle (between 3-7 days post op) and late (more than 8 days post op). Pre-operatively, 3 of the 49 patients were discharged and advised to return for a specific date for their surgery, and were therefore excluded from this sub-analysis.
We found that all of the patients under the age of 25 (10 in total) were discharged early (within 2 days post-surgery). As the age range increased, we saw fewer patients being discharged early and in fact an increase in the number of patients being discharged late. Table 5 demonstrates these findings.
| Age | Total | ||||
|---|---|---|---|---|---|
| LOS (days) | <25 | 26-40 | 41-55 | >56 | |
| 0-2 (Early) | 10 | 8 | 6 | 4 | 28 |
| 3-7 (Middle) | 0 | 3 | 3 | 5 | 12 |
| >8 (Late) | 0 | 0 | 2 | 4 | 6 |
Table 5: Patient post-operative LOS and correlation with patient age.
Time to Surgery v/s Hospital Length of Stay
We can see from the data that, in total, 27 patients were discharged early, and of these, 20 patients (74%) had surgery within two days of their admission. 16 patients in total waited between 3-5 days for their surgery, and following this, the majority of this group (9 patients, 56%) were discharged more than 2 days post-surgery. 3 patients in total waited more than 6 days for their surgery, and there was no significant correlation with these patients being discharged late. Table 6 highlights these findings.
| Post-operative hospital LOS (days) | Total | |||
|---|---|---|---|---|
| Time To Surgery | 43102 | 43166 | >8 | |
| 0-2 | 20 | 4 | 3 | 27 |
| 43164 | 7 | 7 | 2 | 16 |
| >6 | 1 | 1 | 1 | 3 |
| Total | 28 | 12 | 6 | 46 |
Table 6: Correlation between time to surgery and post-operative hospital LOS.
Post-operative Plan
All 49 patients were deemed low-risk with regards to the development of Venous Thromboembolism (VTE). And with this in mind, 47 of the total 49 patients (96%) were given 2 weeks of Low Molecular Weight Heparin (LMWH) upon discharge. 1 patient was given aspirin, and the only 15 year old patient was not discharged on any anticoagulation. All 49 patients were discharged and instructed not to weight bear on that affected limb for a minimum of 6 weeks.
From reviewing the post-operative notes and clinic attendance letters, no patient required revision surgery, developed a Deep Vein Thrombosis (DVT) or Pulmonary Embolus (PE) and only 1 patient developed a post-operative UTI, which resolved with oral antibiotics.
Discussion
The purpose of this study was to evaluate our performance in the management of patients who require surgical fixation for a closed unstable ankle fracture. Through the variables assessed, we feel we have gained a realistic idea into how such patients are managed both pre and post-operatively.
Ankle fracture fixation is not without its risks, and early surgical intervention has been proven to be associated with fewer complications [4,5]. Published data supports early intervention for ankle fractures, and this helps to lower the risk of wound infection or breakdown, whilst also facilitating improved functional outcome [6].
Although our patient numbers were small, our data did suggest that early surgical intervention leads to a decrease in hospital stay,which in itself is favorable and has been shown to be associated with an reduced risk of post-operative infections, improved patient outcomes and high levels of patient satisfaction. A study of the length of the time between the diagnosis of an ankle fracture and operative intervention and the length of subsequent hospital stay was undertaken in 2001 which concluded that the delay in operative fixation beyond 24 hours from injury was associated with an increased post-operative length of stay [7].
Management of ankle fractures initially begins in the ED, where patients undergo a medical assessment before having radiographs to confirm the diagnosis. The sheer volume of patients that attend the ED with life and/or limb threatening conditions, with poor staffing levels and limited hospital beds, will come at a cost of delays to patient care. The knock-on effect of a hospital full to capacity and bed blocking in the ED will lead to delays in when patients are seen/reviewed and ultimately when they can be transferred (to the X-ray department or to the ward) [8,9]. The managerial pillars surrounding this setup will ultimately lead to the delays in patient transfers, as highlighted in this study [10].
We found that more than half of the fractured ankle patients in this study were admitted to the ward within 4 hours of arrival to ED. Without being able to compare this result to patients admitted to wards under other specialties, it is difficult to quantify how good, or bad, this result maybe.
Surgical fixation of ankle fractures requires consideration of the patient’s medical fitness for theatre in addition to the soft tissue status which can often dictate when it is safe to proceed. Through this study we reviewed the time to theatre for these patients, but of course we fully understand that it is not necessarily theatre capacities which can be the limiting factor affecting this step in the patients’ management.
47 of the 49 patients in this study were discharged on a 2 week course of LMWH. The use of post-operative chemical thromboprophylaxis is generally still up for debate. One metaanalysis suggested that isolated foot and ankle surgery has a lower incidence of clinically apparent VTE when compared to other lower limb procedures, and this rate is not significantly reduced using low molecular weight heparin. The incidence of clinically apparent VTE following foot and ankle surgery is reported to be less than 1% without using chemical prophylaxis [11]. Within a study of 45,949 ankle fracture patients the rate of DVT, PE and mortality was 0.12%, 0.17% and 0.37%, respectively. Within the same study, it reported that chemical prophylaxis does not reduce the risk of VTE and therefore is not advocated in the post-operative period following ankle fracture fixation [12].
There is no doubt that there is increased risk of developing VTE in patients with a previous episode of VTE, obesity, use of oral contraceptives, and prolonged periods of immobilization. Owing to this, in addition to evaluating the risk of development of postoperative DVT, in such patients, one has to question the risks vs. benefits of surgery at all [13].
There is significant variation amongst orthopedic surgeons when deciding on the period of non-weight bearing after fixation of ankle fractures, with fracture configuration, medical comorbidities, implant choice and quality of fixation, all playing key roles. All patients in this study were advised to remain non-weight bearing (NWB) for an initial period of 6 weeks, with a 2 week check to inspect the wound and assess progress. There have been some studies which have abandoned the post-operative NWB period and allow patient to weight bear as tolerated from day 1. These studies went on to show that early weight-bearing (EWB) was associated with better functional outcome, shorter hospital stay, and earlier return to work [14-16].
Conclusion
In conclusion, our retrospective cohort study of closed ankle fracture management demonstrates an overall satisfactory level of care which is, generally speaking, uniform in its approach and postoperative plans. Of course there is always room for improvement, especially in patient transfer when in the ED, and also when listing patients for theatre. Earlier surgical fixation will not only help to reduce the post-operative hospital length of stay for these patients but will also help in reducing the financial burden associated with this. We encourage other units to evaluate their own performances to ensure that standards are met and patients are given the optimum level of care.
REFERENCES
- Mehta S.S., Rees K., Cutler L., et al.: Understanding risks and complications in the management of ankle fractures. Indian J Orthop. 2014;48(5):445-452.
- Bugler K.E., White T.O., Thordarson D.B.: Focus on Ankle Fractures. J Bone Joint Surg Br. 2012; 94:1107-1112.
- Hasselman C.T., Vogt M.T., Stone K.L., et al.: Foot and ankle fractures in elderly white women. Incidence and risk factors. J Bone Joint Surg Am. 2003;85(5):820-824,.
- Breederveld R.S., Van Straaten J., Patka P., et al.: Immediate or delayed operative treatment of fractures of the ankle. Injury. 1988;19:436-438.
- Hess F., Sommer C.: Minimally invasive plate osteosynthesis of the distal fibula with the locking compression plate: first experience of 20 cases. J Orthop Trauma. 2011;25(2):110-115.
- Schepers T., De Vries M.R., Van Lieshout E.M.M., et al.: The timing of ankle fracture surgery and the effect on infectious complications; A case series and systematic review of the literature. Int Orthop. 2013;37(3):489-494.
- James L.A., Sookhan N., Subar D.: Timing of operative intervention in the management of acutely fractured ankles and the cost implications. Injury. 2001; 32(6): 469-472.
- Jarvis P.R.E.: Improving emergency department patient flow. Clin Exp Emerg Med.2016;3(2):63-68.
- Department of Health: Improving emergency care in England. Sixteenth Report of Session 2004–05.
- Forster A.J., Stiell I., Wells G., et al.: The effect of hospital occupancy on emergency department length of stay and patient disposition. Acad Emerg Med. 2003;10(2): 127-133.
- Calder J.D., Freeman R., Arverud E D.: Meta-analysis and suggested guidelines for prevention of venous thromboembolism (VTE) in foot and ankle surgery. Knee Surg Sports Traumatol Arthrosc. 2016; 24(4): 1409-1420.
- Jameson S.S., Augustine A., James P.: Venous thromboembolic events following foot and ankle surgery in the English National Health Service. J Bone Joint Surg Br. 2011;93:490-497.
- Stankowski T., Aboul-Hassan S.S., Stepinski P., et al.: Thromboembolic complications after an ankle joint open fracture in a patient with a history of deep vein thrombosis in the lower limbs. Kardiochir Torakochirurgia Pol. 2017;14(1):47-49.
- Simanski C., Maegele M., Lefering R.: Functional treatment and early weightbearing after an ankle fracture: a prospective study. J Orthop Trauma. 2006;20(2):108-114,.
- Gul A., Batra S., Mehmood S., et al.: Immediate unprotected weight-bearing of operatively treated ankle fractures. Acta Orthop Belg. 2007;73(3):360-365.
- Honigmann P., Goldhahn S., Rosenkranz J.: After treatment of malleolar fractures following ORIF-functional compared to protected functional in a vacuum-stabilized orthesis: a randomized controlled trial. Arch Orthop Trauma Surg. 2007;127:195-203.



 Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.
Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.