The Use of orthoplastic techniques for the treatment of lower extremity osteomyelitis and its response to inflammatory markers employing transitional muscle flaps
2 Chicago Foot and Ankle Deformity Correction Center, Department of Surgery Presence, St. Joseph Hospital/Chicago, USA, Email: egodpm@gmail.com
3 Dr. Marks, Craig, and Associates, Rocky River, Ohio, USA
4 Community Foot Specialists, Dayton, Ohio, USA
5 Total Foot Cares, Lakewood, Ohio, USA
Received: 26-Dec-2017 Accepted Date: Jan 10, 2018 ; Published: 13-Jan-2018
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Treating chronic wounds of the lower extremity with underlying osteomyelitis remains challenging. When standard local wound therapy modalities fail, and salvageable treatment options are exhausted, debridement of infected bone and soft tissue with flap coverage augmentation can be a consideration prior to amputation. We propose the first article in the literature on monitoring inflammation labs for resolution of osteomyelitis with reconstructive approach in limb salvage by harvesting muscle flap for coverage of soft tissue deficits overlying resected infected bone. The evaluation of successful outcome is determined by wound closure with resolution of elevated inflammatory labs in a case-control study. Three patients were retrospectively analyzed and successful outcome was achieved in all cases in a short-term follow-up of 16 months. Muscle transpositional flaps should be considered as an alternative salvage procedure prior to amputation.
Keywords
Osteomyelitis, Limb salvage, Muscle transpositional flaps, Amputation
Introduction
Preservation of lower extremity has become paramount with limb salvage rates increasing over the last two decades [1]. Significant soft tissue defects of the lower extremity remain challenging to reconstruct, especially in the heel region due to its poor soft tissue coverage. Increased difficulty occurs when underlying osteomyelitis or exposed hardware is involved. Many treatment options are being utilized ranging from local wound care products, negative pressure wound therapy, and split thickness skin grafts, depending on the wound deficit characteristics (i.e., depth, width, location, and the extent of underlying exposed structures). The patient’s functionality, health, and long-term survival rate are also evaluated and considered in treatment plans. When soft tissue deficits fail to heal by secondary intention, flaps are a consideration. Many authors have reported successful outcomes with radical wound and bone debridement along with augmentation of vascularized tissue transfer [2].
Free fasciocutaneous flaps for lower extremity reconstruction have been reported less frequently in literature due to their lack of bulk and inability to fill dead spaces [3]. Free flaps are time consuming, require sophisticated equipment, and a well-trained surgical team [4]. Furthermore, free flaps have a failure rate as high as 33% [2]. On the other hand, muscle flaps conform better to three-dimension wounds, obliterate dead spaces, and decrease risk of infection by improving the vascularity.
Transpositional muscle flaps are gaining impetus as an alternative surgical option for preserving limbs. Over the past three decades, reconstruction of wound defects using muscle transpositional flaps have gained popularity and yielded excellent success rates in many published series. This reconstructive procedure addresses not only soft tissue coverage but also takes into consideration functional recovery, infection control, and cosmetic outcomes [5]. Muscle transposition flaps provides an adequate wound base for proliferation, covers vital underlying structures, and improves host defenses by providing oxygen while acting as a conduit for systemic antibiotic delivery [6]. This surgical technique, in combination with advanced wound products such as, bilayer synthetic graft and split thickness skin graft (STSG) serves as a limb salvage procedure [7].
Several cases of muscle transpositional flaps for limb salvage have been previously reported in the foot and ankle but monitoring the resolution of osteomyelitis have not. In the present study, we present the first small case series of three patients who underwent muscle transpositional flaps (Peroneal brevis and partial Soleus muscle belly) as an alternative limb salvage procedure for chronic osteomyelitis by the resolution of inflammatory labs in a short term follow up of four to sixteen months postoperatively.
Patients
From April 2015 to August 2016, three participants developed chronic ulcerations with underlying osteomyelitis were evaluated and treated by the primary author’s practice (CC) in Westlake, Ohio. All patients failed local wound care with antibiotic therapy. Patients with osteomyelitis underwent partial resection of the infected bone. All patients had muscle transpositional flap performed with augmentation of fenestrated multilayer wound matrix synthetic graft, negative pressure wound therapy, and application of external fixator. At four weeks postoperatively, STSG was harvested and applied to the muscle transpositional flap site. All patients had a minimum of six weeks of intravenous antibiotics as recommended by the infectious disease team.
All patients were evaluated for muscle flap survival, healing of wound defect, normalization of inflammatory labs with new labs monthly until the healing of the wound defect, and ability to ambulate independently. Patients who met these parameters were deemed as a successful outcome.
Case 1
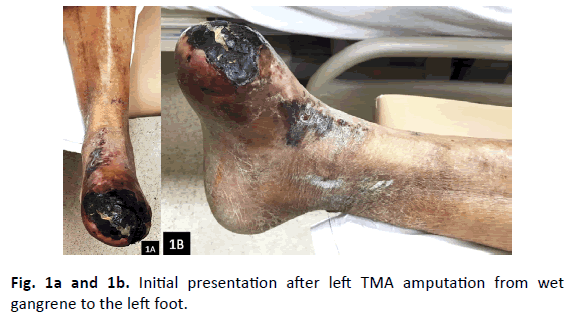
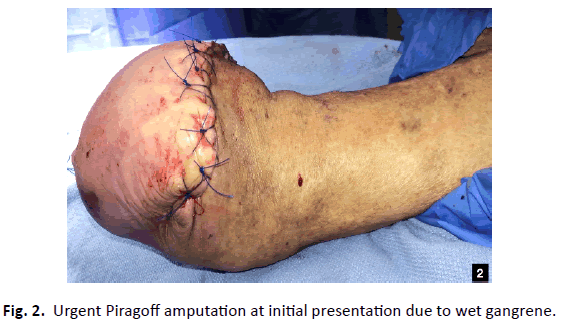
A 67-year-old male with a past medial history (PMH) of insulin dependent diabetes mellitus (IDDM), end stage renal disease (ESRD) on hemodialysis (HD), coronary artery disease (CAD) with aorta valve replacement, peripheral arterial disease (PAD), hypertension (HTN), hyperlipidemia (HLD), and cerebral vascular accident (CVA) presented for a second opinion after a transmetatarsal amputation (TMA) from wet gangrene to his left foot (Fig. 1a and 1b). The dorsalis pedis (DP), posterior tibial (PT), and peroneal arteries were monophasic on Doppler examination to the left lower extremity (LLE). His left TMA stump had reoccurrence of gangrene, measuring 8 cm × 5 cm with five milliliters (mL) of purulent drainage and proximal streaking. Decision was made to proceed with an urgent Piragoff amputation (Fig. 2). Post-operatively, patient had a computed tomography angiography (CTA) that indicated stenosis of the superficial femoral artery (SFA) and popliteal artery with occlusion of the anterior, PT, and peroneal arteries. The patient underwent angioplasty to the left tibioperoneal trunk and peroneal artery. Unfortunately, the patient had a non-healing surgical dehiscence with underlying osteomyelitis after three months of local wound care (Fig. 3a and 3b). Prior to proceeding with below knee amputation, decision was made to proceed with a partial resection of the infected tibia with Peroneal brevis (P. brevis) muscle transpositional flap as the limb salvage procedure (Table 1).
| Age/Sex | Wound Location | Wound Size (cm) | Infection | ESR Pre/Post (mm/hr) | CRP Pre/Post (mg/dL) |
|---|---|---|---|---|---|
| 67 M | Left Piragoff Amputation Stump | 8.0 × 5.0 × 5.0 | Osteomyelitis | 85/35 | 76.6/20.2 |
| 64 F | Right heel ulcer | 7.2 × 4.9 × 0.2 | Osteomyelitis | 41/30 | 87.5/10.9 |
| 51 M | Right heel ulcer | 5.3 × 4.7 × 1.5 | Osteomyelitis | 101/32 | 93/20 |
Table 1. Case series of patient’s age, sex, wound location, wound size, infection, preoperative and post-operative ESR and CRP.
Case 2
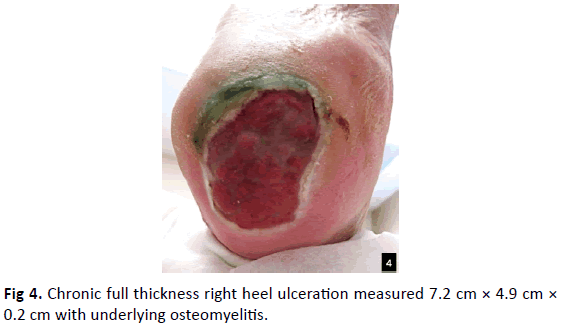
A 64-year-old female with PMH of PAD, hypothyroidism, HTN, venous insufficiency, IDDM, lymphedema, and seizure disorder presented with right chronic decubitus heel ulceration with underlying osteomyelitis (Fig. 4). Patient failed local wound care for one year. On physical exam, patient’s DP, PT, and peroneal pulses were monophasic bilaterally. There was a full thickness ulceration to the right heel that measured 7.2 cm × 4.9 cm × 0.2 cm with a mixed fibrogranular base. The wound did not probe to bone but there was moderate serous drainage present. The patient’s CTA indicated occlusion to the left femeropopliteal and right peroneal artery. The patient underwent left popoliteal and right peroneal artherectomy. Decision was made to proceed with a partial calcanectomy and P. brevis muscle transpositional flap.
Case 3
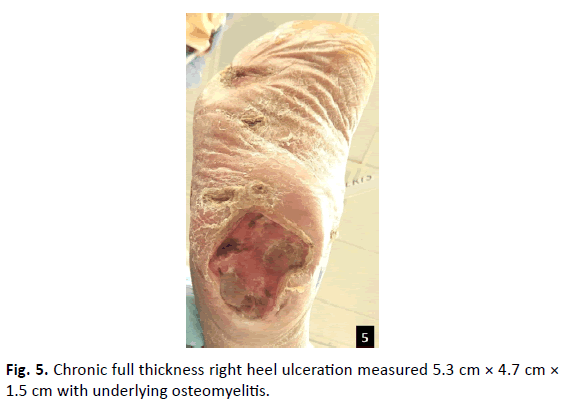
A 51-year-old male with PMH of chronic peripheral vascular disease, IDDM, ESRD on HD, anemia, CAD with percutaneous coronary angioplasty (PTCA), left above knee amputation (AKA), and right TMA presented with infected right decubitus heel ulceration with underlying osteomyelitis (Fig. 5). On physical examination, the patient’s DP, PT, and peroneal arteries were weakly monophasic. There was a full thickness ulceration to the right heel, measured 5.3 cm × 4.7 cm × 1.5 cm with a mixed fibrogranular base. The ulceration probed to bone and undermined the posterior calcaneus by three centimeters. The patient’s CTA indicated stenosis of the SFA with occlusion of the femerotibial trunk and peroneal artery; therefore, he underwent artherectomy of the SFA, femerotibial trunk, and peroneal artery. After failing multiple operative room debridement and synthetic grafts, options of limb salvage versus transtibial amputation were offered to the patient and his family. The patient and his wife refused amputation and wanted to proceed with partial calcanectomy with soleus muscle transpositional flap (Table 1).
Operative technique
Prior to surgery, 60 milliliters (mL) of patient’s peripheral blood was drawn and spun down to prepare for Platelet-rich plasma (PRP) and platelet-poor plasma (PPP) using the MAGELLAN® technology to be injected intraoperatively. 60 mL of bone marrow aspirate (BMA) was harvested from the proximal tibia in the beginning of the surgical case and spun down into bone marrow aspirate concentrate (BMAC) with the MAGELLAN® technology for later injection intraoperatively.
The non-healing wound was then resected down to bone (Fig. 6) and sent for pathology examination. Partial infected bone was then resected and sent for microbiology and pathology examination.
A linear incision was made overlying the fibula. The specific muscle belly for the case was exposed (P. brevis, or Soleus muscle) and detached from its proximal origin site and the distal pedicle was left attached (Fig. 7). Intraoperative Doppler was utilized for the confirmation of the intact pedicle. The muscle belly was then tunneled, transposed, and sutured to the wound (Fig. 8). BMAC and PRP were injected by fenestrating into the transposed muscle flap and PPP was sprayed onto the muscle belly harvest site to enhance its healing potential. The muscle belly was then augmented with a bilayer wound matrix synthetic graft (Fig. 9) and negative pressure wound therapy.
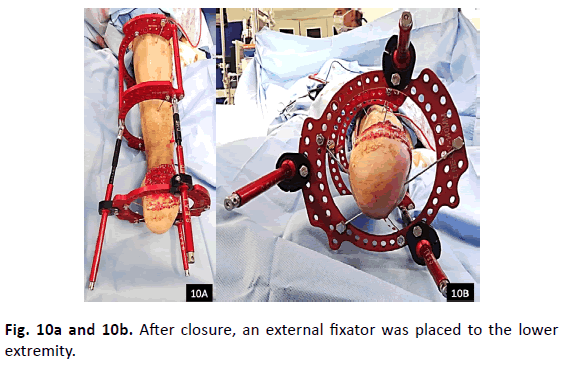
A Jackson-Pratt (JP) Drain® was placed to the lateral leg incision site prior to closure. An external fixator was then placed (Fig. 10A & 10B) onto the lower extremity.
Results
Case 1
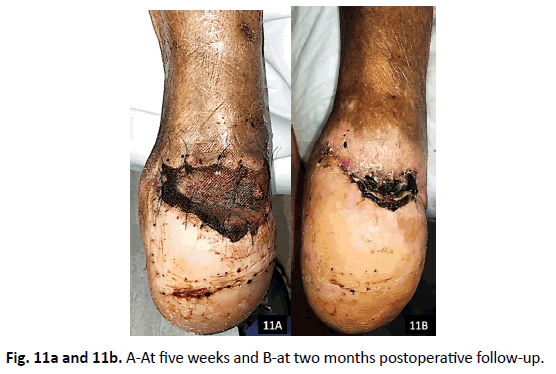
Pre-operatively, patient’s C-reactive protein (CRP) was 76.6 mg/ dL and erythrocyte sedimentation rate (ESR) was 85 mm/hr. Postoperatively at 2 months, both CRP and ESR decreased to 20.2 mg/dL and 35 mm/hr. The patient’s microbiology was positive for Citrobacter freundii complex, Klebsiella pneumonia, and Vancomycin-resistant Enterococcus faecium. Pathology confirmed osteomyelitis to the tibia and the patient was placed on six weeks of Meropenem per infectious disease. The patient healed uneventfully (Fig. 11a and 11b) and resumed weight bearing in prosthesis with an assistant device. Unfortunately, at four months postoperatively, the patient suffered a cardiopulmonary arrest resulting in death (Table 1).
Case 2
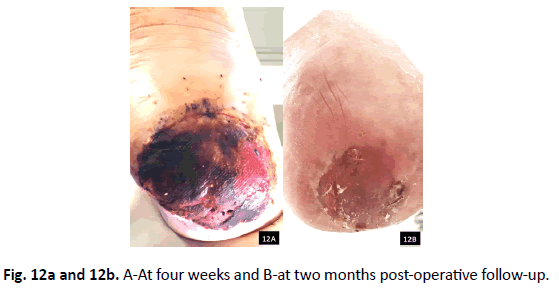
Pre-operatively, patient’s CRP was 87.5 mg/dL and ESR was 41 mm/hr. Post-operatively at 2 months, CRP decreased to 10.9 mg/ dL and ESR decreased to 30 mm/hr. Patient’s microbiology was positive for Methicillin-resistant Staphlococcus aureus (MRSA), Pseudomonas aeruginosa, Providencia rettgeri, Streptococcus anginosus. Pathology confirmed osteomyelitis to the calcaneus. The patient was placed on six weeks of IV Daptomycin and Zosyn per infectious disease. She healed uneventfully (Fig. 12a and 12b) and started weight bearing two months postoperatively. She ambulated with a custom prosthesis to compensate for her calcaneal gait. One-year postop, patient continues to be healed weight bearing in custom brace.
Case 3
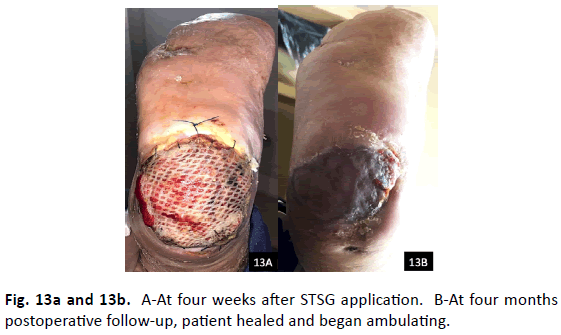
Preoperatively, the patient’s CRP was 93 mg/dL and ESR was 101 mm/hr. Post-operatively at 4 months, the CRP decreased to 20 mg/ dL and ESR decreased to 77 mm/hr. The patient’s microbiology was positive for MRSA, Stenotrophomonas × Maltophilia, and Enterococcus faecalis and pathology came back as both acute and chronic osteomyelitis. The patient was placed on six weeks of IV Vancomycin and Ceftazidime per infectious disease. He had significant drainage postoperatively, which required a longer course of negative pressure wound therapy, two operative debridements, and another STSG harvest and application (Fig. 13a). Four months postoperatively, the patient’s surgical site healed, and he began ambulating (Fig. 13b). Patient continued to be healed 16 months postoperatively (Table 1).
Discussion
The successful treatment of osteomyelitis or exposed hardware in the lower extremity with significant soft tissue defect continued to present a formidable challenge. Aggressive debridement, wound care, antibiotics are usually required [8,9]. When standard wound therapy modalities fail, radical debridements with muscle flap coverage should be considered prior to amputation as muscle transpositional flaps have been shown to have favorable outcomes in cases of infection and osteomyelitis due to its rich vascularity [10].
Eren et al. were the first authors to present a transpositional flap using the Peroneal brevis with a distal pedicle as an alternative treatment plan for skin and soft tissue defects [11]. With the rich vascularity of the Peroneus brevis muscle, the rotation of arc and size of the muscle have been found to be a dependable option for limb salvage for lower extremity wounds [12]. Over the years, Peroneus brevis have been reclassified from a Type II muscle to a Type IV muscle with multiple segmented vascular pedicles [10].
Yang et el. performed a cadaveric series, exhibiting the average length of the Peroneas brevis to be 25 cm. Dissection should be performed to 6 cm proximal to the fibular tip in order to preserve the most distal pedicle [13]. The most distal pedicle of the Peroneus brevis has also been shown to be three fingerbreadths proximal to the tip of the fibula [11]. Not only have Peroneal transpositional flaps been useful in the distal lower extremity, but its applications in the knee are indicated [14].
It has been shown that cultures of greater than 105 organisms per gram of tissue cannot sustain a skin graft or flap. Debridement of soft tissue should be aided by quantitative cultures before definitive soft tissue coverage [15]. Subsequent debridement may lead to larger wound deficits. Muscle flaps are ideal for this purpose as they are pliable, contours to the defects, fills dead spaces, and enhances local delivery of antibiotics. In addition, muscles have shown to be superior to fasciocutaneous tissue in providing local blood supply.
Conclusion
Our case series presented three patients with chronic ulcerations in various locations, from the plantar heel to distal foot amputations. All three cases failed treatment modalities such as multiple surgical debridements, negative wound pressure therapies, and advanced wound care products. We present transpositional muscle flaps as an alternative limb salvage application. Our case series yielded an excellent outcome in patients with soft tissue deficits and underlying osteomyelitis [16]. This procedure has shown to be reliable with favorable results and the importance of resolution of inflammatory lab values monitored monthly until healed wound all at 2 months. Transpositional P. brevis and Soleus muscle flaps are suitable procedures in the limb salvage treatment plan for chronic lower extremity wounds with underlying osteomyelitis or exposed hardware.
REFERENCES
- Hong J.P.: The use of supermicrosurgery in lower extremity reconstruction: the next step in evolution. Plast Reconstr Surg. 2009;123:230-235.
- Thordarson D., Patzakis M., Holtom P., et al: Salvage of the Septic Ankle with Concomitant Tibial Osteomyelitis. FAI. 1997;18(3):151-156.
- Fitzgerald RH., Ruttle PE., Arnold PG., et al.: Local muscle flaps in the treatment of chronic osteomyelitis. J Bone Joint Surg (Am.) 198567:175.
- Mathes SJ., Alpert BS., Chang N.: Use of the muscle flap in chronic osteomyelitis: Experimental and clinical correlation. Plast Reconstr Surg. 1982;69:815-829.
- Yazar S., Lin C., Lin Y., et al.: Outcome comparison between free musle and free fasciocutaneous flaps for reconstruction of distal third and ankle traumatic open tibial fractures. Plastic and reconstructive surgery. 2006;117:2468-2475.
- Paagakos P., McDonald P., Norem N., et al.: De-epithelialized fasciocutaneous turnover flap for recurrence calcaneal cound with osteomyelitis. JFAS. 2014;53:83-87.
- Mukherjee M.K., Parwaz A. Perforator flap: A novel method for providing skin cover to lower limb defects. Med Journal Armed Forces Indian. 2012;68:328-334.
- Bach A., Leffler M., Kneser U., et al.: The versatility of the distally based Peroneus brevis muscle flap in reconstructive surgery of the foot and lower leg. Ann Plast Surg. 2007;58:397-404.
- Eren S., Ghofrani A., Reifenrath M.: The distally pedicled Peroneus brevis muscle flap: a new flap for the lower leg. Plast Reconstr Surg. 2001;107:1443-1448.
- Yang Y.L., Lin T.M., Lee S.S., et al.: The distally pedicled Peroneus brevis muscle flap anatomic studies and clinical applications. J Foot Ankle Surg. 2005;44:259-264.
- Lorenzetti F., Lazzeri D., Bonini L., et al.: Distally based Peroneus brevis muscle flap in reconstructive surgery of the lower leg: postoperative ankle function and stability evaluation. J Plast Reconstr Aesthet Surg. 2010;63:1523-1533.
- Rodriguez E.R., Weiland J., Manson TS., et al: Peroneus brevis Muscle Flap with use of INTEGRA® Wound Matrix and a split thickness skin graft in the Treatment of Full Thickness Ulcerations: Case Reports and Technique Guide. Ortho & Rheum Open Access J. 2015;1:1-5
- Wagner T., Hupkens P., Slater N., et al. The proximally base long peroneal muscle turnover flap: a novel salvage flap for small to medium-sized defects of the knee. Journal of Plastic, Reconstructive & Aesthetic Surgery. 2016;69:533e537.
- Chang N., Mathes SJ.: Comparison of the effect of bacterial inoculation in musculocutaneous and random pattern flaps. Plastic Reconst Surg. 1982;70:1-10.
- Chang N., Mathes S.J.: Comparison of the effect of bacterial inoculation in musculocutaneous and random pattern flaps. Plastic Reconst Surg. 1982;70:1-10.
- Gonzalez M., Weinzweig N.: Muscle flaps in the treatment of osteomyelitis of the lower extremity. Journal of Trauma Injury, Infection, and Critical Care. 2005;58:1019-1023.








 Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.
Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.