Total humerus replacement for Ewing sarcoma in adolescent patient: a case report in Vietnam.
2 Saint Paul Hospital, Vietnam, Email: MANHNGUYENHUU2@aol.com
3 Vietnam National Cancer Hospital, Vietnam
Received: 06-May-2020 Accepted Date: May 25, 2020 ; Published: 03-Jun-2020
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Introduction: The humerus is a relatively common location of malignant bone tumor in general and Ewing sarcoma in particular. However, total humerus replacement after humeral tumor resection is still a fairly rare and challenging surgery for surgeons. Case presentation: A 14-year-old man was diagnosed with Ewing sarcoma. The patient underwent a total humerus replacement and neoadjuvant chemotherapy before and after the surgery. At 6 months post-operative, he was able to return to normal activities with good hand and elbow functions, although limited shoulder movement. MSTS score was 76.7%. There were no significant complications as well as local recurrence or metastasis. Conclusion: Total humerus replacement surgery for the patient of Ewing sarcoma of the humerus had initial positive results. However, the patient needs to follow up longer to evaluate the complications related to the prosthesis as well as the recurrence and metastasis of the tumor.
Keywords
Ewing sarcoma, Total humerus replacement, Bone cancer
Introduction
Proximal Ewing sarcoma is a common type of bone cancer in children and teenagers, accounting for about 16% of all primary bone cancer cases [1]. The common site of this disease is in the diaphysis of the long bones. Ewing sarcoma of the humerus accounts for about 6% of cases. The treatment of Ewing sarcoma usually combines chemotherapy, surgery and radiotherapy [2,3]. Multi-agent chemotherapy regimens proved effective and the patient’s survival rate increased. Therefore, surgery today tends to be aimed at preserving and restoring function for limbs rather than amputation as in the past [4]. Total Humerus Replacement (THR) is a less-common procedure. There have been some reports of THR for humeral bone cancer showing encouraging results [5-8]. We would like to introduce the first case of THR in Vietnam to treat Ewing sarcoma in an adolescent patient.
Case Presentation
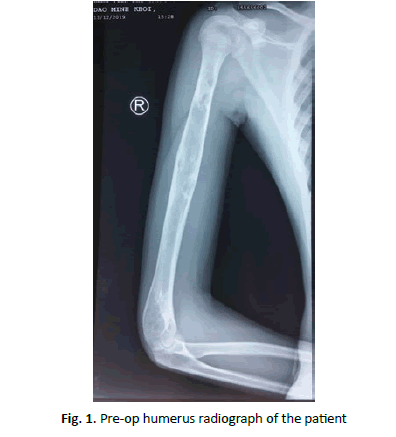
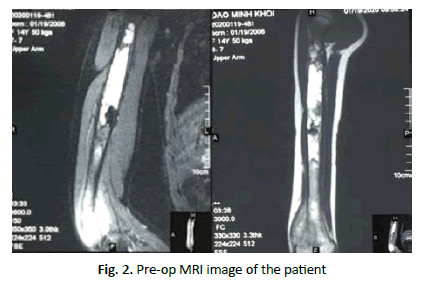
In November 2018, a 14-year-old man was admitted to the hospital due to persistent pain in right arm. The patient was examined and diagnosed with Ewing sarcoma at a pediatric hospital. He was then treated with 4 cycles of chemotherapy and then was assigned to forequarter amputation, but the patient’s family did not agree to this surgery. In December 2019, the patient came to our hospital with painful swelling of the right arm area from the middle third to the distal of humerus. The right elbow movement was limited. Movements of the hands and fingers were normal. There were no signs of tumor metastasis. The patient’s radiography showed an osteolytic lesion in the right humerus, lasting from proximal third to the distal humerus. The MRI image demonstrated that the lesion spread almost to the entire humerus and had invaded the soft tissue around the lateral site of the distal humerus. The biopsy confirmed the diagnosis of Ewing sarcoma of the humerus (Fig. 1 and 2).
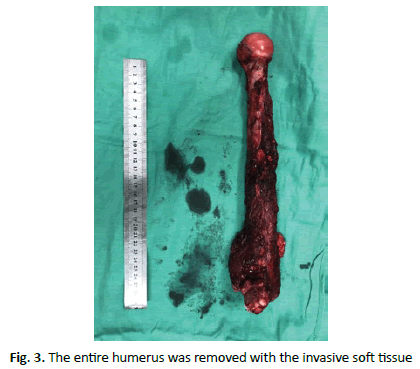
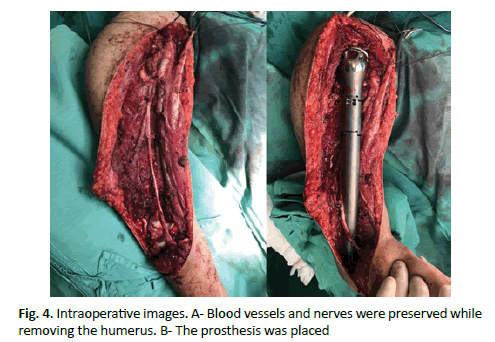
The patient then underwent surgery to remove the tumor with the entire humerus and followed by total humerus replacement. We used an extensive deltopectoral approach to the shoulder which was connected with the anterolateral approach to the humerus and the lateral approach to the elbow. This incision went through the previous biopsy scar. The major blood vessels, rotator cuff, deltoid, biceps and triceps tendons as well as the main nerves (median nerve, radial nerve and ulnar nerve) were carefully extracted and preserved. The invasive soft tissue on the lateral site of distal humerus was removed completely and intact without breaking the tumor. The resection margin was confirmed safe with intra-operative frozen section. To reconstruct the humerus, we used a total humerus prosthesis with the upper part being a humeral head and the lower part being a hinged total elbow component. The deltoid, long head of biceps tendon and rotator cuff were attached to pre-designed holes of the prosthesis (Fig. 3).
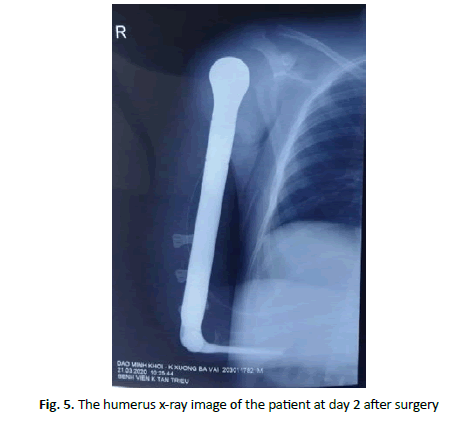
The second day after surgery, the patient’s finger function was almost normal. The patient was also able to move the elbow gently. The immediate post-op X-ray showed the position of the prothesis was very good. As soon as the patient’s incision was healed without any complications, he was continued with post-op chemotherapy. At 6 months after surgery, we have not detected any signs of local recurrence and metastasis or complications. The patient had a good movement of the elbow and the hand. The active shoulder elevation and abduction were 20°and 15°, respectively. The active shoulder internal and external rotation were 20° and 10°, respectively. MSTS score was 23 (76,7%). The patient was very satisfied with the surgery (Fig. 4 and 5).
Discussion
Treatment of Ewing sarcoma, as well as other primary bone cancers in adolescents and children, remains a challenge for surgeons and oncologists. Forequarter amputation may be considered as the first treatment option in cases where it is necessary to completely remove the humerus to ensure cancer safety [4]. However, amputation is rarely accepted by the patient and his family, and it will have severe psychosocial consequences for the patient’s life. The introduction of better diagnostic imaging methods, more effective chemotherapy, greater understanding of anatomy as well as continuous refinement of surgical techniques along with advancements in prosthesis design and materials had made limb preservation more and more feasible, even in cases where the tumor spread throughout the bone [9-14].
The survival rates of patients with limb salvage surgery and those with amputation surgery were similar, although the local recurrence rates were higher [15]. Limb salvage surgery should not affect the patient’s prognosis while optimizing the postoperative function of the limb [16].
Our patients received 4 cycles of chemotherapy before surgery. Chemotherapy has been shown to increase the survival rate of patients after surgery by reducing the rate of recurrence and metastasis [17]. Chemotherapy also helps to reduce tumor size and localize the tumor, making its boundaries clearer. This makes it easier to remove the tumor and thus increase the success rate of the surgery [18]. After surgery, the patient continued to receive early chemotherapy, as soon as the incision was well healed. In a study of 703 patients of bone cancer, Imran et al. concluded that patients who started to resume chemotherapy within 21 days after surgery had a higher survival rate. The authors suggest that starting chemotherapy within 21 days after surgery helps maintain the overall dose intensity [19].
Total humerus replacement is a rare procedure, so there are very few reports of the results of this surgery. Puri et al. reported results of THR in 20 patients (9 cases of osteosarcoma, 8 cases of Ewing sarcoma, and 3 of chondrosarcoma) with an average follow-up time of 41 months. The 5-year survival rate was 52%, the local recurrence rate was 26.3% and the MSTS score was 22. At 5 years postoperative, the implant survival rate was 95% [5].
Also, Natarajan et al. reported the surgical outcomes of 11 patients who underwent THR. The authors reported good and excellent results of 90.9%. The 5-year survival rate was 77.9%. The patients in this study had very limited active shoulder range of motion, but the elbow and hand movements were relatively good, with an MSTS score of 80% [6].
Suhel Kotwal et al. report the results of THR in 20 patients with humeral malignant tumor with an average follow-up time of 42.9 months. The average MSTS score was 71.5%, the active shoulder elevation and abduction were 15° and 12.5°, respectively. The 10-year survival rate was 70% [7].
In THR surgery, almost all surgeons use an extensive deltopectoral approach that connects to the anterolateral approach to the humeral shaft. When approaching the elbow, some authors extended the incision posteriorly, followed by the posterior approach to the elbow [18], while others use the anterior approach to the elbow [7]. Our patient had a tumor that invaded the surrounding soft tissue at the lateral site of the distal humerus, so we extended the incision laterally to the lateral approach of the elbow to make it easier to remove the entire tumor. The advantage of this incision is not to damage the elbow extension mechanism, so the movement of the elbow after surgery recovered well. Revealing and preserving the radial nerve was also relatively easy. However, its disadvantage is that it is difficult to reveal the medial neurovascular bundle (brachial artery, median nerve, and ulnar nerve).
At 6 months after surgery, the patient was able to move the elbow and fingers relatively well. However, the active movement of the shoulder was very limited, although we have tried to preserve and reattach the deltoid and rotator cuff to the prosthesis. Other authors had similar results of poor recovery of the shoulder [5-7]. It is important to advise patients and families about the potential of significant loss of shoulder activities as well as the rehabilitation of the shoulder will take more time and effort. Also, patients need to learn how to use the scapular movement to compensate for the lack of shoulder joint function [7].
This is the first case of total humerus replacement performed in Vietnam. So we have a lot of technical difficulties and little experience with this type of surgery, while the neurovascular anatomy of this area is very complicated. Moreover, the invasive soft tissue made the surgery even more difficult.
The limit of this case presentation is a short follow-up time. The patient should be monitored longer to assess the recurrence or metastasis of the tumor, the function of the patient’s arm as well as the survival of the implant.
Conclusion
The total humerus replacement surgery for Ewing sarcoma showed very satisfactory initial results. Although the active movement of the shoulder was limited, the patient was able to move the fingers and elbow well. This is the first case of total humerus replacement in Vietnam. It promises to open up a brighter future for patients of humeral bone cancer, when the surgery not only preserves the limb after safely removing the tumor, but also recreates the aesthetic and function for the patients.
REFERENCES
- Goldman L., Schafer A.I.: Goldman's Cecil Medicine (24th ed.), Elsevier Saunders. 2012;1326.
- Arndt C.A., Crist W.M.: Common musculoskeletal tumors of childhood and adolescence. N Engl J Med. 1999;341:342-352.
- Bielack S.S., Kempf-Bielack B., Delling G., et al.: Prognostic factors in high grade osteosarcoma of the extremities or trunk: an analysis of 1,702 patients treated on neoadjuvant cooperative osteosarcoma study group protocols. J Clin Oncol. 2002;20:776-790.
- Segal O., Kollander Y., Gosheger G.: Total Femur Replacement Using a Humeral Reconstruction Component in a 36-month-Old Ewing Sarcoma Patient. Isr Med Assoc J. 2019;12:833-834.
- Puri A., Gulia A.: The results of total humeral replacement following excision for primary bone tumour. J Bone Joint Surg Br. 2012;94:1277-1281.
- Natarajan M., Sameer M., Kunal D., et al.: Custom-made endoprosthetic total humerus reconstruction for musculoskeletal tumours. International Orthopaedics. 2012;36:125-129.
- Kotwal S., Moon B., Lin P., et al.: Total Humeral Endoprosthetic Replacement following Excision of Malignant Bone Tumors. Sarcoma. 2016;6318060.
- Wafa H., Reddy K., Grimer R., et al.: Does total humeral endoprosthetic replacement provide reliable reconstruction with preservation of a useful extremity? Clin Orthop Relat Res. 2015;473:917-925.
- Allison D.C., Carney S.C., Ahlmann E.R., et al.: A meta-analysis of osteosarcoma outcomes in the modern medical era. Sarcoma, 2012;704872.
- Ayoub K.S., Fiorenza F., Grimer R.J., et al.: Extensible endoprostheses of the humerus after resection of bone tumours. J Bone Joint Surg Br. 1999;81:495-500.
- O'flanagan S.J., Stack J.P., McGee H.M., et al.: Imaging of intramedullary tumour spread in osteosarcoma: a comparison of techniques. J Bone Joint Surg Br. 1991;73:998-1001.
- Onikul E., Fletcher B.D., Parham D.M., et al.: Accuracy of MR imaging for estimating intraosseous extent of osteosarcoma. AJR Am J Roentgenol. 1996;167:1211-1215.
- Grimer R.J., Taminiau A.M., Cannon S.R.: Surgical outcomes in osteosarcoma. J Bone Joint Surg Br. 2002;84:395-400.
- Ozaki T.: Diagnosis and treatment of Ewing sarcoma of the bone: a review article. J Orthop Sci. 2015;20:250-263.
- Rougraff B.T., Simon M.A., Kneisl J.S., et al.: Limb salvage compared with amputation for osteosarcoma of the distal end of the femur. A long-term oncological, functional, and quality-of-life study. J Bone Joint Surg Am. 1994;76:649-656.
- Sewell M.D., Spiegelberg B.G., Hanna S.A., et al.: Total femoral endoprosthetic replacement following excision of bone tumours. J Bone Joint Surg Br. 2009;91:1513-1520.
- Malawer M.M., Link M.P., Donaldson S.S.: Sarcomas of bone. Cancer: Principles Pract Oncol. 1993;2:1794-893.
- Prabowo Y., Reksoprodjo A.Y.: Modified total humeral replacement on unusual osteosarcoma of the humerus: A case report. IJSCR. 2019;58:132-137.
- Imran H., Enders F., Krailo M., et al.: Effect of time to resumption of chemotherapy after definitive surgery on prognosis for non-metastatic osteosarcoma. J Bone Joint Surg Am. 2009;91:604-612.



 Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.
Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.