Treating post-traumatic lower extremity end neuroma formation: A novelty approach
2 Research Fellow, Presence St. Joseph Hospital/Chicago, IL. Chicago Foot and Ankle Deformity Correction Center, USA
3 Medical Student, Avalon University School of Medicine, Chief Clinical Rotating Student at Adventist Hospital, Hinsdale IL. Research Associate, Chicago Foot and Ankle Deformity Correction Center, Chicago, USA, Email: HamidKhan2@gmail.com
Received: 19-Jun-2017 Accepted Date: Aug 01, 2017 ; Published: 04-Aug-2017
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
A prospective study was performed to gauge the outcomes of a newer and modified approach to the surgical management and treatment of post-traumatic lower extremity end neuroma formation experienced by patients. Chronic peripheral nerve pain of the lower extremity that presents after a traumatic episode or post-surgical procedures continues to be a major concern for physicians and is affecting patients worldwide. This article will demonstrate a unique approach that was utilized in two different patients that suffered from severe peripheral nerve pain due to end-neuroma development involving the deep peroneal nerve (DPN). Patient success was measured based on the extent of pain relief after surgery, the ability to walk, and the duration of time it took for each patient to return to work.
Keywords
Neuroma, Neurectomy, Nerve grafting, Nerve translocation, Nerve repair, Nerve incontinuity
Background
Neuroma, a termed coined in medicine by Odier of Geneva in 1803, is a clinical description of a tumor or mass growing from a nerve usually consisting of nerve fibers [1]. Throughout the years, various tactics for treating neuromas have been executed, these include injections, decompression, external and internal neurolysis, as well as neurectomy (with or without vein or muscle implantation) [2,3]. Neuroma formation caused by the result of direct trauma to the nerve trunk has also been linked to the formation of numerous lower limb injuries [2]. Neurectomy of the affected end-neuroma or neuroma in continuity is one current example of an acceptable treatment option for such cases [4]. Current literature and surgical practices prove muscle implantation after end-neuroma resection provides significant pain relief although high recurrence of the neuroma is still possible [2,4-7]. Although there are various methods of nerve implantation into vein and bone that have been documented, very little data has been published regarding nerve implantation within the deep peroneal nerve into the distal one third of the tibia or ankle area. As with most areas of medicine where numerous options for treatment and management are possible, some methods have proven to be much more successful than others. One such option that has proven successful is the practice of the using a conduit with a nerve human processed allograft implanted into bone and is now being viewed as an effective technique for the management of chronic peripheral nerve pathology [1]. Re-implantation of the end-neuroma resection in the distal one third of the lower limb is no longer used as much due to an increased risk for failure to develop and inadequate muscle mass commonly found within that segment [2,4]. As advancements in medical procedures are made, so are the surgical options for surgeons, this brief case study portrays this very notion. The difference between a simple bone implantation and our surgical approach within this study (a neurectomy of the deep peroneal nerve), is the bridging of the affected nerve segment with allograft and implanting it into the tibia [4]. The outcomes proved to be meaningful and have created a subject for further discussion and studies to be performed.
Materials and Methods
The implantation of AVANCE processed nerve allograft axogens for bridging severed nerves was performed in each of the following cases. The motive for using these allografts is due to its proven structural support in regenerating axons, its ability to revascularize, remodel, and its high success rates as a clinically studied off-theshelf solution for such occurrences [2]. In a multi-center study, there was an 87% meaningful recovery in sensory, mixed and motor nerve gaps seen [4]. Thus, eliminating the need for additional surgical sites. AVANCE nerve allografts were seen as being particularly promising for these patients because the grafts not only offer the benefits of human peripheral nerve micro-architecture and handling but they also aid in preserving extracellular matrix, helping to create a natural healing response [5].
This study focuses on two patients that suffered from failed deep peroneal nerve end-neuroma implantation into muscle at the level above the ankle. In both cases, the end-neuroma was resected and post-surgical follow up visits of over six-month period were scheduled. An anterior tibial muscle segmental flap was performed in both procedures in hopes of providing adequate cushioning and coverage to the proximal native nerve conduit allograft coaptation site. Patient success was measured based on the extent of pain relief after surgery, the ability to walk, and the duration of time it took for each patient to return to work.
Case 1
A 46-year-old male who presents with excruciating pain anterior to right lower extremity. A crushed type injury to the right lower extremity occurred two years prior. At that time, nerve muscle implantation was enacted and results were unsuccessful. Nerve conduction velocity test or (NCV) was performed showing absent velocities at the affected area with abnormal amplitudes of the deep peroneal nerve. Thus, two diagnostic nerve blocks were enacted, confirming deep peroneal nerve involvement at the pain site. Following the execution of the nerve blocks, the patient was able to walk without any pain in his right leg or dorsum of the foot. The patient underwent end-neuroma resection-neurectomy with conduit allograft coaptation and bone implantation to the lateral aspect of the distal tibia.
Case 2
A 42-year-old female complaining of pain in her right lower extremity that she has been experiencing for about twelve months. Approximately one year ago, the patient also stated that she had experienced trauma to her right distal one third lower extremity area. She describes her pain as a nine based on a scale of one (minimum pain) to ten (maximum pain). The patient’s nerve conduction velocity test was abnormal indicating velocity reduction at the distal one third aspect of her right lower extremity. This patient was submitted to the exact same surgical procedure as described in case 1.
Experimental Procedure
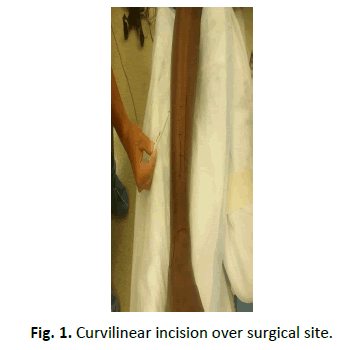
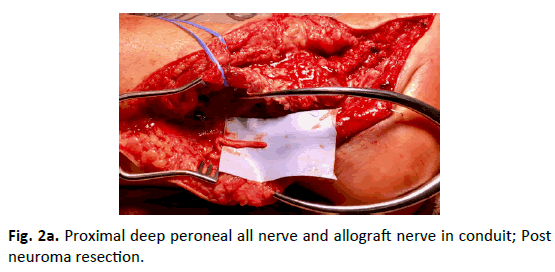
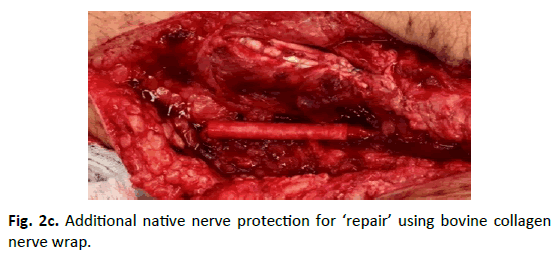
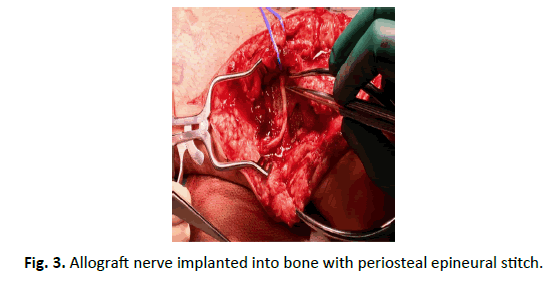
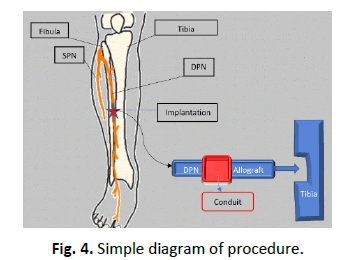
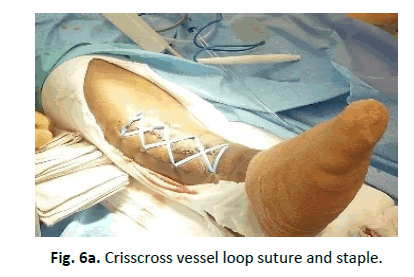
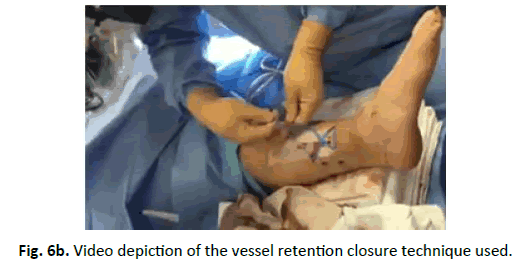
A 7 cm curvilinear incision was performed over the localized damaged nerve (Fig. 1). Dissection of the anterior distal one third of right leg compartment was performed exposing 5.0 cm of the deep peroneal nerve. Once the nerve was identified, a neurectomy of the end-neuroma was performed and under microscope the proximal part of the nerve was coapted into a conduit half-way proximally. An allograft nerve was placed at the other end of the conduit distally bridging both ends inside the conduit while maintaining a 3 mm gap between the allograft and the proximal part of the deep peroneal nerve (Fig. 2). A stitch was placed through the conduit and epineurium on both sides of the conduit with a 9.0 nylon; two stitches on each side and the use of an INTEGRA bovine collagen wrap was also applied. Following the stitching, a 3 mm perforation was performed at the lateral aspect of the tibia. The allograft portion of the nerve was placed into the tibia perforation (Fig. 3) and a muscle flap was dissected from the anterior tibial muscle to be over the implanted nerve (Fig. 4). Skin closure was performed utilizing subcuticular to subcutaneous, subcutaneous to subcuticular technique with 3.0 ethilon. Retention of the skin was made with a crisscross vessel loop suture and staples (Fig. 5). Dressing was applied using 4×4 gauze, vacuum dressing, and a four-inch ace elastic band (Fig. 6). The patient’s first follow-up visit was completed two weeks later.
Discussion
When surgical intervention to the DPN is necessary, nerve implantation into the muscle is a common practice performed [8,9]. Due to the lack of muscle mass at the anterior distal one third of the lower extremity, it is highly recommended that implantation of the nerve into the bone with muscle transfer be performed [3,8]. In these particular cases, we decided to resect the neuroma, connect the native nerve with a conduit, implant an allograft in the area of the distal tibia and cover the segment with the anterior tibial muscle so that it would provide better stability, soft tissue coverage and overall protection. To further understand the benefits of this surgical method it is important to recall that the muscle to tendon ratio in relation to the area involving the ankle joint is quite unbalanced, there is far less muscle and a significantly higher amount of tendon [3]. Therefore, by using muscle implantation following the establishment of the allograft portion of the nerve into the tibia perforation, the nerve is being forced to grow in a pathway that is well controlled, resulting in the decreased likelihood for painful end-neuroma and also significantly reducing the worry for pain to arise post-operatively.
The anatomical position of the DPN not only makes itself vulnerable to injury but the accompanying symptoms associated with injury play a vital role in assessing what options are best for each patient [9]. These symptoms include foot drop, loss of sensation to the leg and foot, excruciating pain, weakness of the ankle and foot, and loss of muscle mass to the leg which is caused when the muscle’s nerve stimuli is affected [3,8,9]. In some cases, these symptoms tend to disappear as the nerve recovers [10]. However, it is still important to understand that surgery to the DPN is vital for cases in which complete independent recovery is not possible [6,7].
After a year of excruciating pain to their right legs, the above patients underwent DPN surgery. Two weeks following the surgery, each patient was assessed for pain and wound healing. There were no signs of infections, the edges of the wound were well coapted and the patients reported no pain in their right leg. The patients were also asked to describe their pain on a scale of one (minimum pain) to ten (excruciating pain) while taking a few steps with the support of a walker and in both cases, patients reported not having any pain. By their third post-op visit, both patients continued to deny any pain while walking with the assistance of a walker.
In virtue of these results, it can be noted that DPN surgery with conduit graft and bone implantation is an excellent technique for neuromas, especially if it is located at the distal one third of the leg; an area that lacks muscle and is very tendinous [3,8]. Other approaches that could have been used include decompression of the nerve or neurolysis of the nerve, both of which have been well documented [11-13].
Conclusion
Due to a high incidence of neuroma caused by trauma and the increased occurrence of these neuromas within the DPN, specifically at the distal one third anterior muscle compartment of the lower extremity, a standard for newer treatment protocols and methods of management needed to be assessed. We believe this new microsurgical approach performing a neurectomy with conduit allograft repair and bone implantation will yield better outcomes in the treatment of peripheral nerve pathology. Based on our 2 case studies and the immediate lack of pain related to this procedure. Clearly, this method demonstrates an effective and excellent alternative for neuromas found within this anatomical location and it is of great importance that this procedure and the relative material in its association continued to be practiced and studied in further detail.
REFERENCES
- Boldrey E.: Amputation neuroma in nerves implanted in bone. Ann Surg. 1943; 118: 1052-1057.
- Dellon A.l.: Treatment of the painful neuroma by resection and muscle implantation. Plastic reconstructive surgery. 1986; 77: 427-436.
- Campbell, William W.: Evaluation and management of peripheral nerve injury. Clinical Neurophysiology. 2008; 119: 1951-965.
- Brooks D.N., Weber R.V., Chao J.D., et al.: Processed nerve allografts for peripheral nerve reconstruction: A multicenter study of utilization and outcomes in sensory, mixed and motor nerve reconstructions. Microsurg. 2012; 32: 1-85.
- Johnson P.J., Newton P., Hunter D.A., et al.: Nerve endoneurial microstructure facilitates uniform distribution of regenerative fibers: A post hoc comparison of midgraft nerve fiber densities. J Reconstr Microsurg. 2011; 27: 83-90.
- Mass Daniel P., Michael C Ciano., Tortosa R., et al.: Treatment of Painful Hand Neuromas by Their Transfer into Bone. Plastic and Reconstructive Surgery. 1984; 74: 182-185.
- June W, Chiu DTW. Painful Neuromas. Annals of Plastic Surgery. 1999; 43: 661-667.
- Koch H, Hass F.: Treatment of painful neuroma by resection and nerve stump transplantation into a vein. Ann Plast Surg. 2003;51: 45-50.
- Rodriguez E.: Internal neurolysis and grafting of the superficial Peroneal Nerve in the treatment of nerve injury using advance nerve graft. Ortho and Rheum Journal. 2015; 1: 1-3.
- Kenneth J.L., Calisman M, Tsai T.: Results of Surgical Treatment of painful neuromas of the hand. The Journal of Hand Surgery. 1982; 7: 190-193.
- Dellon AL.: Treatment of symptoms of diabetic neuropathy by peripheral nerve decompression. Plast Reconstrb Surge. 1992; 89: 689-697.
- Dellon AL.: Decompression of peripheral nerves for symptoms of diabetic neuropathy: pain management considerations. The Pain Clinic. 2001; 3: 11-16.
- Dellon AL.: Entrapment of the deep peroneal nerve on the dorsumof the foot. Foot and Ankle. 1990; 11: 73-80.





 Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.
Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.