Unique presentation of bilateral patellar tendon rupture in a patient with renal failure: a case report
2 Orthopedic Senior Registrar, King Fahad Military Medical Complex, Dhahran, Saudi Arabia
3 Orthopedic Consultant, King Fahad Military Medical Complex, Dhahran, Saudi Arabia
4 Medical intern, Imam Abdulrahman Bin Faisal University, Dammam, Saudi Arabia
5 Medical intern, AlJouf University, Aljouf, Saudi Arabia
Received: 10-Aug-2018 Accepted Date: Sep 25, 2018 ; Published: 02-Oct-2018
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: The presence of a bilateral patellar tendon rupture is an extremely rare occurrence. Only a very limited number of cases have been reported worldwide. When it does occur, it is usually associated with systemic diseases such as rheumatoid arthritis, systemic lupus erythematosus, hyperparathyroidism, and renal failure. Our case report is the first in its unique presentation and second case in the Gulf area. Case presentation: We describe a 48 year old female with end stage renal disease and other comorbidities who presented to the emergency department with bilateral knee pain and swelling after experiencing a fall. A preliminary diagnosis of bilateral patellar tendon rupture was made based on the patient’s complain of bilateral knee pain and physical examination which revealed a palpable infrapatellar pouch, in addition to the patient’s inability to actively extend the knee. Confirmation of the diagnosis was done by imaging studies which showed patella alta, and complete tendon ruptures bilaterally. This patient was managed surgically with a bilateral patellar tendon repair using a Krachow suture technique. Post-operatively, the patient was discharged and started on a physical rehabilitation program. Conclusion: our patient post operatively had a good outcome with no complications and complaints since this operation which’s not a standard for this kind of unique rupture went smoothly, as a result our patient gained equal full range of motion bilaterally with no stiffness or limitation and gained full recovery, bilateral patellar tendon rupture is not a relatively common condition, but since the timing between presentation and management is the most important factor in determining the outcome, it is important to have a high index of suspicion in order to reach this diagnosis, and effectively manage it as soon as possible.
Keywords
Bilateral Patellar Tendon Rupture, End Stage Renal Disease, Krachow Technique
Introduction
It is well known that Patellar tendon rupture refers to a disruption of the patellar tendon, which originates from the patella and inserts into the tibial tuberosity. Bilateral patellar tendon rupture is rarely seen in clinical practice as well as in literature. Only a very limited number of cases have been reported in the Kingdom of Saudi Arabia. Due to the uncommon nature of this condition, patellar tendon ruptures can be misdiagnosed in up to 38% of cases [1]. The aim of this study is to present this case as a second case occurring in the Gulf area, and to stress on the importance of timely diagnosing and managing similar cases. The first case reported in the gulf area was in Riyadh, and was a case of bilateral simultaneous patellar tendon rupture in a 35 year old healthy male athlete after a sports injury, in the absence of systemic disease or steroid usage. Both tendon disruptions were in the proximal mid substance of the patellar tendon, and underwent successful krachow technique repair [2].
Multiple previous studies have concluded that there is an association between patellar tendon rupture and systemic conditions such as rheumatoid arthritis, Systemic Lupus Erythematosus (SLE), hyperparathyroidism, and renal failure. Corticosteroid injections and previous local injury to the tendon have also been linked to patellar tendon rupture. Although extremely rare, there have been reported cases of patellar tendon ruptures in patients without any known risk factors [2,3]. Patellar tendon ruptures affect males more than females [3], and are much less frequent than ruptures of the quadriceps tendon. In addition, they usually occur in patients less than 40 years of age, with reported cases of bilateral patellar tendon ruptures occurring in as young as a 9, and 12 years old patients [4,5]. This is opposed to quadriceps tendon ruptures, which usually occur in patients above 50 [6]. A similar case of bilateral patellar tendon rupture was reported in a healthy 45 year old male who tripped on a step while unloading heavy boxes. The patient experienced excellent recovery following open repair with additional tension-band-wiring [7]. A 2016 study reported patellar tendon ruptures in two obese patients following total knee arthroplasty, and suggested that extensor mechanism allografts are a suitable alternative treatment in such cases [8]. Other reported cases include a spontaneous bilateral patellar tendon rupture in a patient with systemic lupus erythematosus [9], and rupture following minor trauma in a 38 year old male [10]. Due to the rarity of this condition, emergency physicians should maintain a high degree of suspicion in all patients with concerning clinical and/or radiographic findings [3].
Case Report
We report the case of a 48 year old Saudi female, who is a known case of type 2 diabetes mellitus, hypertension, hypothyroidism and end stage renal disease. She presented to the emergency department complaining of bilateral anterior knee pain and swelling after a simple fall on her knees. She was unable to walk. There was no history of previous trauma to the knee, or similar complaints in the past. The patient was afebrile.
On physical examination, there was moderate effusion of both knee joints, with the presence of an infrapatellar gap and high riding patella bilaterally. The patient was not able to actively extend either knee.
Laboratory findings showed evidence of chronic renal failure; BUN: 21 mg/dl, Creatinine: 688 mg/dl. In addition, a high ALP and an iron profile suggesting anemia of chronic disease were seen. A complete blood count, parathyroid and thyroid hormone levels were normal at the time of presentation.
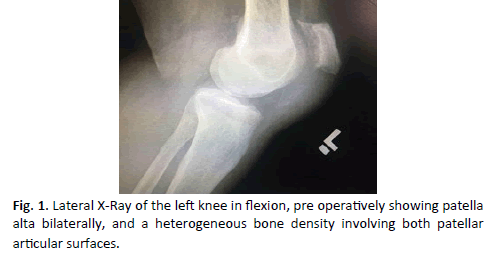
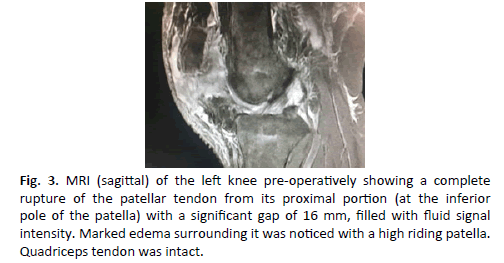
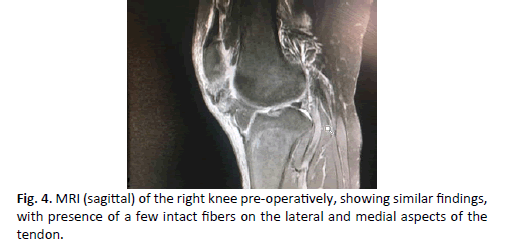
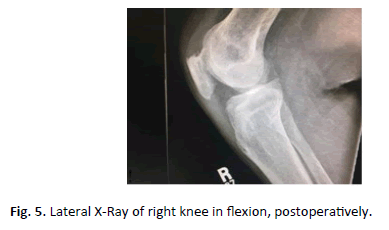
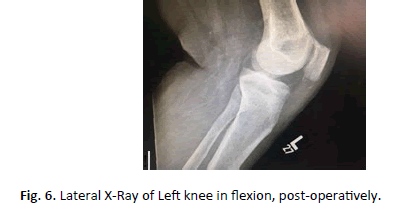
X-Rays were done for both knees in a lateral view with flexion (Fig. 1 and 2). The X-rays showed patella alta bilaterally, and a heterogeneous bone density involving both patellar articular surfaces. Magnetic Resonance Imaging (MRI) of the left knee (Fig. 3), showed a complete rupture of the patellar tendon from its proximal portion (at the patellar attachment) with a significant gap of 16 mm, filled with fluid signal intensity. The right knee (Fig. 4), showed similar findings, except for the presence of a few intact fibers on the lateral and medial aspects of the tendon. Both knees showed marked surrounding edema. Both quadriceps tendons were intact. The patient underwent bilateral surgical repair of the patellar tendons using a Krachow suture technique. Due to the unique nature of each rupture, there were slight differences in the techniques used to repair them. #5 Ethibond was used to repair both sides. On the right side, after identifying & exposing the rupture site, it was found to be complex tear, the middle third of the tendon was avulsed from its’ tibial insertion while the medial & lateral thirds were avulsed from the inferior pole of the patella. An intra-operative decision was made to use Krachow sutures for both the medial & lateral thirds and pass them through two tunnels in the patella. The middle third was also fixed with krachow sutures that were passed through a transverse tunnel in the tibia, (Fig. 5- 8).
Fig.3: MRI (sagittal) of the left knee pre-operatively showing a complete rupture of the patellar tendon from its proximal portion (at the inferior pole of the patella) with a significant gap of 16 mm, filled with fluid signal intensity. Marked edema surrounding it was noticed with a high riding patella. Quadriceps tendon was intact.
On the left side, the standard Krachow suture technique was done, as the patellar tendon avulsion was at the inferior pole of the patella. During the operation, bilateral calcifications of the Patellar tendon and the Quadriceps tendon were noted, which is considered a typical finding of tendinopathy that is associated with renal failure.
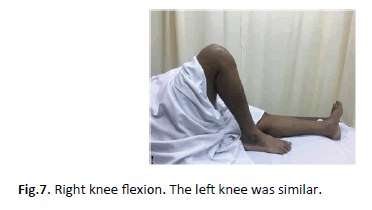
Shown below are pictures taken during her follow up appointment post operatively. The patient had good range of motion, and assessment of her gait revealed no abnormalities.
Her Rehabilitation protocol was bed to wheelchair mobilization from Day 1 with a hinged knee brace that was locked in extension. Passive range of motion exercises were started at 1 month, and by 2 months post operatively active range of motion exercises had been initiated. Weight bearing was also gradually started by 2 months while using a walker frame.
At 3 months follow up she was subjectively doing fine. By then she had started walking with a walker frame. On examination, passive knee flexion was 0–100 degrees, while active knee flexion was 0-80 degrees bilaterally. The Patient is still on regular physiotherapy for Quadriceps strengthening.
Discussion
Rupture of the patellar tendon is not commonly witnessed in clinical practice or reported in previous literature. Its’ exact incidence is unknown, but it less common than other injuries to the extensor mechanism, such as patellar fractures and ruptures of the quadriceps tendon [3]. Before discussing the details of this condition, it is important to revise the extensor mechanism of the leg. This mechanism is achieved by the quadriceps muscle group, quadriceps tendon, the patella, patellar tendon, and the tibial tubercle. Patellar tendon rupture refers to a disruption of the patellar tendon, which originates from the patella and inserts into the tibial tuberosity.
Patellar tendon rupture rarely occurs in a spontaneous manner. It is usually the result of a weakened tendon caused by underlying systemic diseases. These diseases include rheumatoid arthritis, Systemic Lupus Erythematosus (SLE), hyperparathyroidism, and renal failure. In addition, repeated corticosteroid injections and previous local injury to the tendon may cause it to be weakened, resulting in its’ rupture. This rupture is more common in the male gender, and is much less common than ruptures of the quadriceps tendon. Patellar tendon ruptures occur most commonly as a result of minor trauma to the knee while it is in a flexed position, with concomitant contraction of the extensor mechanism.
There are multiple patterns of rupture of the patellar tendon. The most common one is by an avulsion from its’ proximal insertion. Other patterns include midsubstance avulsions, and distal avulsions from the tibial tubercle.
Patients with patellar tendon rupture usually complaint of sudden infrapatellar pain, with or without a popping sensation. In addition, they will have difficulty bearing weight. On physical examination, there will be elevation in the patellar position, localized tenderness of the area, and a palpable infrapatellar gap. Patients will not be able to perform active knee extension.
X-rays are usually required, in antero-posterior, lateral, and skyline or merchant views. They will show patella alta (high riding patella). Other X-Ray changes that have been described include loss of the welldefined linear margin of the patellar tendon, and increased density of the infra-patellar fat pad [3]. The Insall-Salvati ratio in this condition is usually above 1.2 (normal ratio is between 0.8 and 1.2). Other imaging modalities include ultrasonography, which may be used to detect and localize the disruption. In addition, ultrasonography may have a role in assessing the need for surgery, and predicting the response to it [11]. Magnetic Resonance Imaging (MRI) may be used to differentiate between partial and complete ruptures. Magnetic Resonance Imaging (MRI) is the most sensitive method in diagnosing patellar tendon rupture.
Treatment of a ruptured patellar tendon can be done through multiple methods. Non-operative management may be considered in partial tears with an intact extensor mechanism. Non-operative management involves immobilization in a fully extended knee position, followed by progressive weight bearing exercises.
If non-operative management is not successful, surgery must be considered. Surgical management includes either tendon repair or tendon reconstruction. Repair of the tendon is indicated in cases of complete rupture only if it is possible to approximate the tendon at the site of disruption. Reconstruction is considered in cases of severe disruption or degeneration which cannot be repaired or approximated.
Complications of patellar tendon rupture include stiffness, atrophy and decreased strength of the quadriceps muscle. These complications may be prevented by starting early range of motion and quadriceps strengthening exercises.
Conclusion
This case report describes a 48-year-old female with end stage renal disease who presented to the emergency department with bilateral knee pain and swelling with an inability to bear weight after a simple fall. The diagnosis of bilateral patellar tendon rupture was suspected after clinical examination revealed bilateral knee effusions and a palpable infrapatellar gap bilaterally. Confirmation was achieved by imaging through X-Rays of the knee, which showed patella alta, and an MRI scan which showed complete rupture of the patellar tendon starting from proximal portion with marked surrounding soft tissue edema. This case was managed surgically with bilateral patellar tendon repair using a Krachow suture technique. Management of this patient was performed as soon as possible in hopes of achieving the best overall patient outcome.
Only a few previous cases similar to this one have been reported in the past. Due to the uncommon nature of this condition, a high index of suspicious is required to make the diagnosis. The timing of diagnosis and management of this condition is the most important factor in determining whether or not complications will ensue. Management should be achieved in a timely manner to prevent, or limit the degree of quadriceps atrophy, and prevent any contractures from occurring. It is extremely important that surgeons be aware of this injury, and knows when to suspect, how to diagnose, and effectively manage it.
Acknowledgements
We would like to express our gratitude for Dr. Aisha M. Alosail who provided us with her expertise during the review process of this manuscript.
REFERENCES
- Sanchez G., Ferrari M. B., Sanchez A., et al.: Proximal patellar tendon repair: internal brace technique with unicortical buttons and suture tape. Arthrosc Tech. 2017;6(2):e491-e497.
- AlGashim H., AlMoallem H., AlShahrani N., et. al.: Bilateral patellar tendon rupture. Am J Res Commun. 2014;2(2):1-6.
- Sibley T., Algren D. A., Ellison S.: Bilateral patellar tendon ruptures without predisposing systemic disease or steroid use: a case report and review of the literature. Am J Emerg Med. 2012;30(1):e3–261.e5.
- Kim J. R., Park H., Roh S.et. al.: Concurrent bilateral patellar tendon rupture in a preadolescent athlete: A case report and review of the literature. J Pediatr Orthop B. 2010;19(6):511-514.
- Muratli H. H., Çelebi L., Hapa O.,et. Al.: Bilateral patellar tendon rupture in a child: a case report. Knee Surg Sports Traumatol Arthrosc. 2005;13(8):677-682.
- Abduljabbar F. H., Aljurayyan A., Ghalimah B.: Bilateral simultaneous quadriceps tendon rupture in a 24-year-old obese patient: a case report and review of the literature. Case Rep Orthop. 2016;1-6.
- Tarazi N., O’loughlin P., Amin A.: A rare case of bilateral patellar tendon ruptures: A case report and literature review. Case Rep Orthop. 2016;1-3.
- Goldstein Z. H., Yi P. H., Haughom B. D., et. al.: Bilateral extensor mechanism disruption after total knee arthroplasty in two morbidly obese patients. Orthopedics. 2015;38(5): e443.
- Albayrak İ., Küçük A., Arslan Ş., et. al.: Spontaneous patellar tendon rupture in a case followed up for diagnosis of systemic lupus erythematosus. Eur J Rheumatol. 2014;1(4):159–160.
- Webb L. X., Toby E. B.: Bilateral rupture of the patella tendon in an otherwise healthy male patient following minor trauma. J Trauma. 1986;26(11):1045-1048.
- Karlsson J, Kälebo P, Goksör LA, et. al.: Partial rupture of the patellar ligament. Am J Sports Med. 1992;20(4):390-395..





 Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.
Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.