Introduction of one minute preceptor as teaching learning method for postgraduates in orthopaedics
2 Professor, Department of Psychiatry, PGIMS, Rohtak, India
3 FNB Trauma Fellow, PGIMS, Rohtak, India
4 PG, Orthopaedics, PGIMS, Rohtak, India
Received: 02-Jan-2023, Manuscript No. jotsrr-23- 85274; Editor assigned: 03-Jan-2023, Pre QC No. jotsrr-23- 85274 (PQ); Accepted Date: Jan 26, 2023 ; Reviewed: 18-Jan-2023 QC No. jotsrr-23- 85274 (Q); Revised: 25-Jan-2023, Manuscript No. jotsrr-23- 85274 (R); Published: 30-Jan-2023
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: Orthopaedic teaching at Postgraduate level is more procedure oriented and due to time and workload constraints, teaching of clinical reasoning skills somehow gets neglected. One Minute Preceptor (OMP) is a learner oriented micro skill method of teaching for improving learning at Postgraduate level. So this study was proposed to introduce OMP as a teaching learning method for Postgraduate in Orthopaedic.
Methodology: This interventional educational study was conducted at the Department of Orthopaedics, PGIMS Rohtak after obtaining institutional ethical clearance. After sensitization of students and faculty members, 6 OMP sessions per student were conducted. Feedback was taken at the end by students as well as faculty members. The question format included both open‑ended and close‑ended questions. Rating was done on a five‑point Likert scale
Results: 95.8% (n=23) Postgraduate students found OMP as an effective tool in learning clinical skills while 83% students (n=20) felt confidentin clinical skills after using OMP. Similarly, all faculty members perceived that OMP improved confidencein assessing clinical knowledge of residents as well as helped them to focus on students’ weak areas.
Conclusion: In busy clinical settings, OMP is feasible and effectiveteaching learning method and induces a significan improvement in clinical skills of postgraduate student
Keywords
One-minute preceptor, Orthopaedics, clinical reasoning, postgraduate.
Introduction
Postgraduate teaching in clinical specialties like Orthopaedics is hampered a lot due to time constraints & work overload. Traditional methods of teaching during postgraduation like seminars, lectures, and journal clubs focus more on theoretical knowledge with minimal focus on clinical skill acquisition. Clinical skill teaching is mainly dependent on case presentations which demands lots of dedication from both ends.
One‑Minute Preceptor (OMP), a five‑step “microskill” model of clinical teaching, which is short yet effective teaching–learning method [1]. Five microskills are -
1.Get a commitment- ask the learner to articulate his/her diagnosis or plan
2.Probe for supporting evidence- evaluates the learner’s knowledge or reasoning.
3.Teach a general rule- Teach the learner common “take home points” that can be used in future cases.
4.Aimed preferably at an area of weakness for the learner Reinforce what was done well- provide positive feedback
5.Correct mistakes-provide constructive feedback with recommendations for improvement.
Main strength of this method is teaching in a case based format in outpatient departments or wards with meaningful student–teacher interaction in an ambulatory care setting with minimal disruption to patient care. In his original description, Neher et al found that all respondents found this model as “somewhat helpful” while 58% faculty members found it as “extremely helpful” as clinical teachers [1,2]. Literature shows the use and effectiveness of this method with mixed perceptions [3-5]. Therefore the present study was designed to introduce One Minute Preceptor teaching learning method for Post graduate students in Orthopaedics and to determine the factors influencing learner satisfaction with the module.
Aims and Objectives
To introduce OMP as a teaching learning method among Post graduate students in Orthopaedics.
1.To implement One Minute Preceptor as a Teaching Learning Method for Postgraduates in Orthopaedics
2.To assess the feasibility and acceptability of One Minute Preceptor as a Teaching Learning Method for Postgraduates in the department of Orthopaedics.
3.To assess the perceptions of postgraduates about One Minute Preceptor as a Teaching Learning Method in the department of Orthopaedics.
4.To assess the perceptions of the Faculty about One Minute Preceptor as a Teaching Learning Method in the department of Orthopaedics.
Method
Study Design
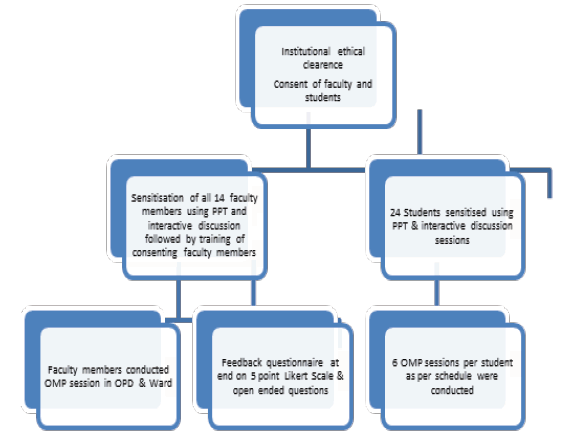
Prospective, non-randomized, intervention study: This study was conducted in Department of Orthopaedics, PGIMS Rohtak after obtaining institutional clearance [6]. Sensitization of faculty members and students was done using PPT and interactive discussions. A feedback questionnaire based on 5 point Likert scale was filled at the end as mentioned in fig. 1.
Participants
Orthopaedics post graduate students (n=24), Sample size: 24 Post graduate students and 14 faculty members of Department of Orthopaedics. 6 OMP sessions per students were conducted by faculty members in OPD and ward. For a particular student, each session was conducted on a different topic by a different faculty member. Some of the topics on which OMP sessions were conducted included POP cast, non-union, Swelling examination, external fixator etc. This record sheet was countersigned by both faculty member as well as student
After six OMP sessions, the residents were asked to fill a questionnaire consisting of questions about their perception on different aspects of OMP. The questionnaire was validated from PG students, faculty members, and members of medical education unit. The question format included both open‑ended and close‑ended questions. Rating was done on a five‑point Likert scale of 1=“strongly disagree” to 5= “strongly agree” [7]. Faculty perception about usefulness and implementation of OMP as a regular teaching tool was also evaluated through a separate, validated structured questionnaire (Fig. 1).
The statistical analysis was done using SPSS (IBM SPSS Statistics 21.0; Armonk, NY, USA). The c ategorical variables w ere summarized using percentages and frequencies, and continuous data were analyzed using mean and standard deviation wherever applicable.
Description
Separate feedback form of students and faculty were used which were validated by experts. Study tools are attached as annexure II. Data collection process: A hard copy after every session (n=144) was fi lled and same was used for collecting the data. After completion of all OMP sessions, google forms for final feedback forms containing open ended and close ended questions were used to collect the data.
Data Analysis
Quantitative- After completion of every session, a separate sheet was filled in by faculty member conducting the OMP session, containing details of OMP session including overall assessment of student by the faculty member in percentage (0-100).
After completion of all OMP sessions, a separately designed questionnaire for collecting student (n=24) and faculty (n=14) feedback was filled in Google forms. Feedback questionnaire contains both open ended and close ended questions.
Qualitative- Reflections and feedback with open ended responses were analyzed using thematic analysis and verbatim were also shared.
Ethics: The study was commenced after approval from ethics committee of the institution. The Institution Ethics Committee letter dated 21/6/2021 number BREC/21/47 attached as annexure. Informed Consent Form and Participant Information Sheet are attached as annexure.
Result
A total of 144 OMP sessions were conducted in which each resident underwent six sessions. Besides the presenter, session was observed by other residents and faculty available for better learning and acclimatization about OMP.
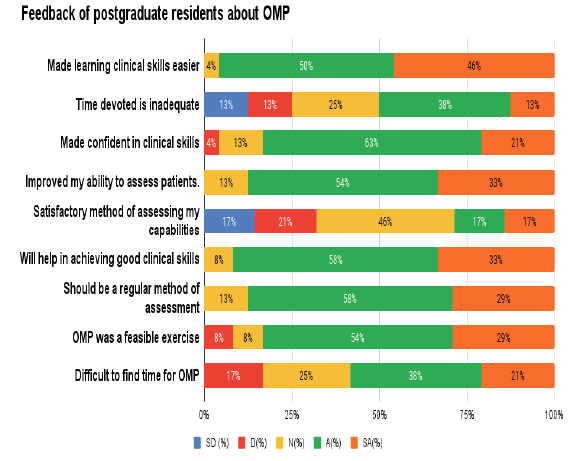
Feedback of postgraduate residents about one-minute preceptor Feedback of postgraduate residents about one-minute preceptor according to Table 1.
Table 1. Showing Likert Scale of OMP preceptor for student’s perception
| S.N. | STATEMENT | n | SD | D | N | A | SA |
|---|---|---|---|---|---|---|---|
| 1 | It made learning clinical skills easier | 24 | - | - | 1 | 12 | 11 |
| 2 | The time devoted in OMP teaching is inadequate | 24 | 3 | 3 | 6 | 9 | 3 |
| 3 | It made me confident in clinical skills | 24 | - | 1 | 3 | 15 | 5 |
| 4 | It improved my ability to assess patients. | 24 | - | - | 3 | 13 | 8 |
| 5 | It is a satisfactory method of assessing my capabilities as an Orthopaedician | 24 | 4 | 5 | 11 | 4 | 4 |
| 6 | It will help in achieving good clinical skills | 24 | - | - | 2 | 14 | 8 |
| 7 | It should be a regular method of assessment | 24 | - | - | 3 | 14 | 7 |
| 8 | OMP was a feasible exercise | 24 | - | 2 | 2 | 13 | 7 |
| 9 | It was difficult to find time for OMP in busy schedule | 24 | - | 4 | 6 | 9 | 5 |
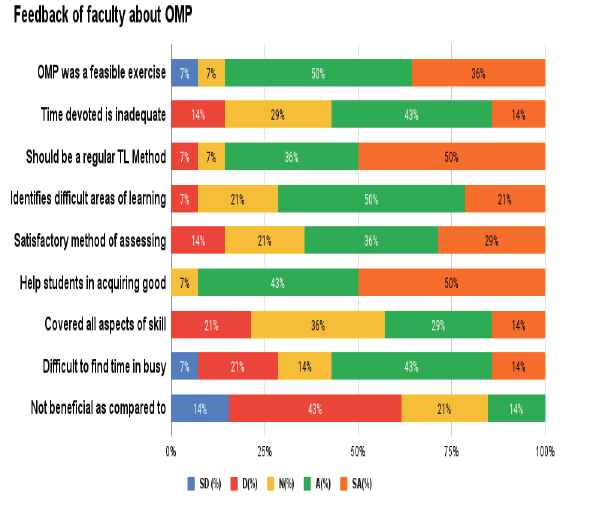
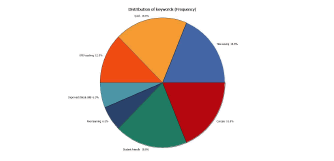
A graphical representation of the same is depicted in fig. 2. As evident in fig. 2, 95.8% (n=23) Postgraduate students found OMP as an effective tool in learning clinical skills while 83% students (n=20) felt confident in clinical skills after using OMP. Only 50% (n-12) students felt that time devoted in OMP is inadequate while 58% (n=14) found difficult to find time for OMP in busy schedule. There was no consensus among the students regarding OMP as a satisfactory method of assessing capabilities as an Orthopaedician (Table 2 and fig. 3).
Table 2. Showing feedback of faculty members in using OMP
| S.N. | STATEMENT | n | SD | D | N | A | SA |
|---|---|---|---|---|---|---|---|
| 1 | OMP was a feasible exercise | 14 | 1 | _ | 1 | 7 | 5 |
| 2 | The time devoted in OMP teaching is inadequate | 14 | _ | 2 | 4 | 6 | 2 |
| 3 | It should be a regular Teaching Learning Method | 14 | _ | 1 | 1 | 5 | 7 |
| 4 | It helped me identifying the difficult areas of learning of student. | 14 | _ | 1 | 3 | 7 | 3 |
| 5 | It is a satisfactory method of assessing competency of students | 14 | _ | 2 | 3 | 5 | 4 |
| 6 | It will help students acquiring good clinical skills | 14 | _ | _ | 1 | 6 | 7 |
| 7 | It covered all essential aspects of skill teaching | 14 | _ | 3 | 5 | 4 | 2 |
| 8 | It was difficult to find time for OMP in busy clinical schedules | 14 | 1 | 3 | 2 | 6 | 2 |
| 9 | It is not beneficial for students as compared to traditional Teaching Learning Methods | 14 | 2 | 6 | 3 | 2 | 0 |
All the 14 Faculty members who conducted the OMP sessions gave a positive feedback. All of them perceived that OMP improved confidence in assessing clinical knowledge of residents. 71% (n=10) perceived that it helped them to identify and focus on students’ weak areas. They advocated that OMP should be incorporated as a routing teaching method for PG students. According to Tables 3 and 4, while only 50% students find time inadequate for an OMP session, only 14% faculty members disagreed to it. Just like students, 58% faculty members also perceived that there was difficult to find time for OMP in busy clinical settings.
Table 3. Satisfaction index of students feedback (n=24)
| S.N. | Item | Satisfaction Index |
|---|---|---|
| 1 | It made learning clinical skills easier | 95.8 |
| 2 | The time devoted in OMP teaching is inadequate | 50 |
| 3 | It made me confident in clinical skills | 83.3 |
| 4 | It improved my ability to assess patients. | 87.5 |
| 5 | It is a satisfactory method of assessing my capabilities as an Orthopaedician | 33.4 |
| 6 | It will help in achieving good clinical skills | 91.6 |
| 7 | It should be a regular method of assessment | 87.5 |
| 8 | OMP was a feasible exercise | 93.4 |
| 9 | It was difficult to find time for OMP in busy schedule | 58.3 |
Table 4. Satisfaction index of faculty members feedback (n=14)
| S.N. | Item | Satisfaction Index |
|---|---|---|
| 1 | OMP was a feasible exercise | 85.7 |
| 2 | The time devoted in OMP teaching is inadequate | 56.8 |
| 3 | It should be a regular Teaching Learning Method | 85.7 |
| 4 | It helped me identifying the difficult areas of learning of student. | 71.3 |
| 5 | It is a satisfactory method of assessing competency of students | 64.1 |
| 6 | It will help students acquiring good clinical skills | 92.6 |
| 7 | It covered all essential aspects of skill teaching | 42.6 |
| 8 | It was difficult to find time for OMP in busy clinical schedules | 56.8 |
| 9 | It is not beneficial for students as compared to traditional Teaching Learning Methods | 14.2 |
SATISFACTION INDEX
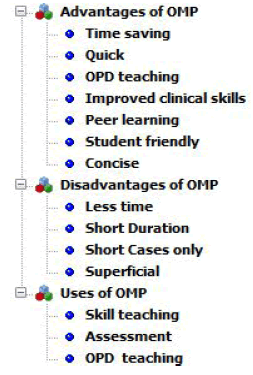
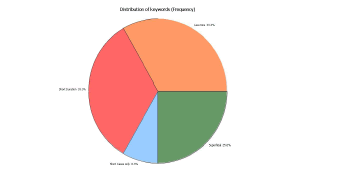
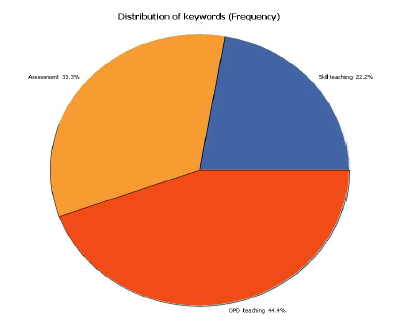
The satisfaction indices of students and faculty were calculated and it was found that satisfaction index ranged from 33.4% to 95.8% among students and 14.2% to 92.6% among faculty. Students’ satisfaction index regarding OMP as a satisfactory method of assessing capabilities as an Orthopaedician was lowest (33.4%) whereas satisfaction index of faculty regarding use of OMP in acquiring good clinical skills was rated highest (92.6%). Qualitative analysis as per Fig. 4 and 5.
Open ended questions were used for qualitative analysis. 14 codes were created as per transcript using both inductive and deductive approach with different color labels. 3 Categories were created after combining one/ /more codes. Results were analyzed using QDA Miner Lite Software.
Overall distribution of codes is shown in figure below
ADVANTAGE OF OMP
Both the faculty members and students found OMP as an effective teaching learning method which is concise, quick and time saving especially effective in clinical skill teaching and learning in OPD settings as given in fig. 5-7. Some of the verbatim used by students were
1. “Short and focused.”
2. Quick and effective way to improve clinical skills.”
3. “It mimics the final viva for exam.”
4. “One on one, quick, to the point.”
5. “It provides direct interaction with patient and teacher both.”
Similarly some of the faculty verbatim was
1. “Less time consuming.”
2. “One to one interaction.”
3. “It is not better or worse. It is another weapon in the armory.”
4. “Students acquire good clinical skills”
DISADVANTAGE OF OMP
Time constraints were the most common shortcoming of OMP pointed out both by faculty as well as students. Students verbatim on shortcomings of OMP mainly included
1. “Short duration.”
2. “Short cases discussed only.”
3. “Time constraint.”
4. “Difficult to find time during hectic schedule.”
Faculty missed the detailed teaching of a particular topic
“Cases are not pre-decided, students are not prepared for specific cases and their own assessment.” “Not much time for detailed teaching of concepts.”
Uses of OMP
Both the faculty members and students were of opinion that main utility of OMP remains for OPD teaching in a limited time span. Besides it, assessment and clinical skill teaching and learning are other scopes of OMP as depicted in fig. 8.
Discussion
The present study w a s conducted in Department of Orthopaedics at PGIMS Rohtak to evaluate the perception of PG residents and the faculty about OMP teaching model in an ambulatory setting. The results showed that the residents perceived OMP as an effective teaching tool in improving their clinical reasoning skills and enhancing their confidence and motivation for further study.
A median number of 21 residents agreed or strongly agreed to 6 out of 9 items in the study questionnaire. 87.5% students advocated routing use of OMP in PG teaching. Literature also shows similar results on student perception in previous studies [4-6].
In a comparative study using videotaped teaching encounters, 164 medical students preferred OMP model to the traditional teaching in the study conducted by Teherani et al [5]. A significantly high rating was given to all the items, especially students’ clinical reasoning, fund of knowledge, feedback, student involvement in decision‑making process, and overall effectiveness.
Similar learning experience was perceived by gynecology residents after the OMP‑based teaching in a study conducted by Machado in 2020 [6]. Possible explanation of it could be due to the student’s behavior that were more comfortable with didactic teaching and hence could not properly interpret learner‑centered processes such as OMP
Another advantage of OMP is learner centered approach and improved learning skills. Same results were found useful in teaching radiology residents using OMP by Kachewar et al. [3] and nursing staff by Miura et al. [8]
Apart from learners, faculty (preceptor) acceptance of OMP was also been found to be high in the present study. 70% faculty members agreed that OMP increased their confidence in rating the students’ knowledge as well as helped in assessing their learning needs. The results are in concordance with a previous multicentric study conducted by Aagaard et al. in which 116 preceptors after viewing videotaped encounters of both OMP and traditional model felt more confident in rating students, presentation skills, clinical reasoning, and knowledge [9]. In coherence with results, positive perceptions about OMP were also given by the faculty after undergoing faculty development programs in previous research [10,11].
Issues pertaining to time Management were reported in the present study, where 50% residents and 58% faculty members perceived that the time devoted to each session was inadequate which could be explained due to lack of experience and old habits of teaching everything about a case
Aim of OMP is to provide need‑based crisp clinical pearls to the learners so as to enhance their clinical reasoning skills rather than the fund of knowledge and this fact will be clearer once OMP is routinely practiced in the PG teaching.
Limitation
Few limitations of the study includes a small sample size of 24 residents and being a single center study on PG residents, results may not be generalisable. Increasing the number of OMP sessions on the residents before taking their perceptions might have ensured the authenticity of results. Third, the study did not measure long‑term durability of the intervention’s effects.
Implication Of Study
The study was a pilot project that was aimed to introduce OMP for PG medical teaching. Favorable results in it will pave the way for bigger studies evaluating its long‑term feasibility, applicability, and educational impact.
Directions for future research / action: OMP is now a routine teaching learning method in Orthopaedics and same can be used in other clinical and para clinical specialties. OMP sessions are planned in Small group discussion for undergraduate teaching at our institute.
Conclusion
OMP was considered to be an effective method of learning by the postgraduates and was found to induce a significant improvement in the clinical skills of students. The study concludes that it is feasible to use OMP for teaching learning method for the postgraduates in Orthopaedics. Both residents and faculty perceived OMP as an effective and feasible teaching tool in outpatient teaching of PG residents. Along with traditional teaching, OMP can be supplemented to improve analytical skills of the postgraduate residents. Faculty members also accepted OMP as an effective method of formative assessment.
There are favorable evidences in literature regarding usage of an effective teaching learning method. With increasing workload and busy clinical settings, OMP seems to be the need of hour.
References
- Neher JO, Gordon KC, Meyer B, Stevens N. A five-steli “microskills” model of clinical teaching. J Am Board Fam liract. 1992 Jul 1; 5(4):419-24. [Google Scholar]
[CrossRef]
- Swartz MK. Revisiting “the one-minute lirecelitor”. J liediatr Health Care. 2016 Mar 1; 30(2):95-6. [Google Scholar]
[CrossRef]
- Kachewar SG. Imlilementing one minute lirecelitor for effective teaching and learning among radiology residents. Indian J Alilil Radiol. 2015; 1(1):104. [Google Scholar]
- Chan LK, Yang J, Irby DM. Alililication of the oneâ?minute lirecelitor technique by novice teachers in the gross anatomy laboratory. Anat&nbsli; sci educ. 2015 Nov 12; 8(6):539-46.. [Google Scholar]
[CrossRef]
- Teherani A, O'Sullivan li, Aagaard EM, Morrison EH, Irby DM. Student liercelitions of the one minute lirecelitor and traditional lirecelitor models. Medical teacher. 2007 Jan 1;29(4):323-7. [Google Scholar]
[CrossRef]
- Machado MA, Medeiros EL. Training lirecelitors of Obstetrics-Gynecology Residents through the One-minute lirecelitor Model. Revista Brasileira de Ginecologia e Obstetrícia/RBGO Gynecology and Obstetrics. 2021 Aug;43(08):622-6. [Google Scholar]
[CrossRef]
- Likert R. A technique for the measurement of attitudes. Arch lisychol. 1932. [Google Scholar]
- Miura M, Daub K, Hensley li. The one-minute lirecelitor model for nurse liractitioners: A liilot study of a lirecelitor training lirogram. &nbsli;J Am Assoc Nurse liract. 2020 Dec 1; 32(12):809-16. 2020 Dec; 32(12):809-816. [Google Scholar]
[CrossRef]
- Aagaard E, Teherani A, Irby DM. Effectiveness of the one-minute lirecelitor model for diagnosing the liatient and the learner: liroof of concelit. Academic medicine. 2004 Jan 1; 79(1):42-9. [Google Scholar]
- Eckstrom E, Homer L, Bowen JL. Measuring outcomes of a oneâ?minute lirecelitor faculty develoliment worksholi. J gen intern med. 2006 May; 21(5):410-4. [Google Scholar]
[CrossRef]
- Salerno SM, O’Malley liG, liangaro LN, Wheeler GA, Moores LK, Jackson JL. Faculty develoliment seminars based on the oneâ??minute lirecelitor imlirove feedback in the ambulatory setting. J Gen Intern Med 2002; 17:779â??87 [Google Scholar]
[CrossRef]



 Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.
Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.