Reconstruction of forearm and elbow defects by pedicled periumbilical perforator based Thoracoabdominal flap : an alternative to free flaps
2 Associate Professor, Department of Orthopaedics. PGIMS Rohtak, India
Received: 18-Mar-2023, Manuscript No. jotsrr-22- 92266; Editor assigned: 21-Mar-2023, Pre QC No. jotsrr-23- 92266 (PQ); Accepted Date: Mar 29, 2023 ; Reviewed: 25-Mar-2023 QC No. jotsrr-23-92266 (Q); Revised: 28-Mar-2023, Manuscript No. jotsrr-23-92266 (R); Published: 31-Mar-2023
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
We evaluated the outcome of thoracoabdominal flap coverage of a large defects in the upper limb, especially around the elbow joint and forearm for its reliability, and early and late post-op outcome in 15 patients. All require this flap for indications, additional procedures, and complications. Injuries to the upper limb are associated with significant soft tissue loss requiring coverage. Local tissue/flap options may not be available to cover the defect necessitating the import of tissue from a distant source as the flap. The mean size of the flap in this study was 56 cm2 (range 20 cm2–150 cm2 ). This flap is based on the perforators of the deep inferior epigastric artery that are maximally centered on the periumbilical region 1. The patients were observed for at least 3 weeks for any flap or donor site complications. The patients were again followed up at 3 months intervals and the donor site scar was also assessed. The flaps survived in all patients except for marginal necrosis in three patients. One of these patients required an additional procedure for coverage. The flap is technically easy to plan and it drapes around upper limb defects, with no significant donor site morbidity. Thus this flap is very useful in coverage of the upper limb and recommended as a first-line flap for coverage of large hand, forearm, and elbow defects. Competent upper limb physiotherapy is recommended to get optimal results.
Keywords
Thoracoabdominal flap, Periumbilical Perforators (PUP), Deep Inferior Epigastric Artery (DIEA), coverage of upper limb defects
Introduction
The upper limb defects on many occasions require a cover with a full-thickness flap [1]. Even in the modern era of micro-vascular surgery, free tissue transfer is an attractive option but the consequences of failure can be devastating [2]. Literature supports outcomes of successful pedicled flaps. Abdominal and groin flaps continue to be the workhorse flaps with composite tissue loss. The groin flap has some limitations; mainly the dependent position of the limb that leads to flap edema and is unable to cover very large defects also. The thoracoabdominal flap being an axial flap has several distinct advantages over the groin flap [3]. The groin flap may be insufficient if large areas need to be covered. So, we were looking for a flap that can cover large defects, involving the elbow, is easy to harvest, and is positioned higher up in the trunk so that the postoperative edema is less [4].
Taylor and Boyd described the vascular territory of the deep inferior epigastric artery in 1975 [1]. As the predominant vascular connections were oriented upward and laterally, they suggested that a thoracoabdominal axis of the flap is the most suitable. It has been used for upper limb and groin reconstruction as a pedicled flap [5, 6]. Hence our study describes our experience with the thoracoabdominal flap.
Materials and Methods
We operated on 15 patients with this flap to reconstruct the upper arm defects. Among these 11 patients. were males and only 4 pt. were females. 10 patients in the 40 years-60 years age group and the rest was in the 22 years40 years age group. We have the defect size varied from 20 cm2 to 150 cm2 . The surgical procedure was assessed for technical ease also
After the surgery, all patients were observed for a minimum period of 3 weeks. Complications including marginal necrosis and complete necrosis of the flap, infection, dehiscence, etc. were noted. Patients were also assessed at a 3 month follow up visit when delayed complications such as complications of immobilization e.g. stiffness, pressure ulcers, etc. were noted. The donor site was observed for complications like infection, dehiscence, unsightly scar, and donor site hernia. At a 3 month follow-up visit, the donor site scar was assessed.
OPERATIVE TECHNIQUE
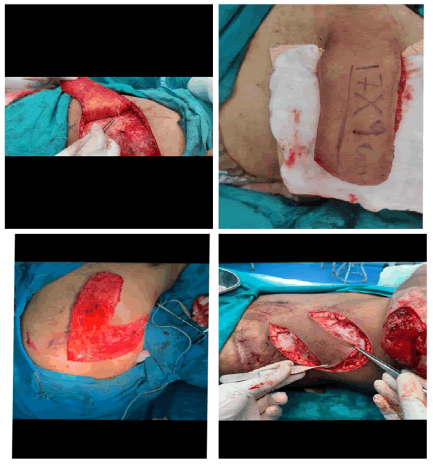
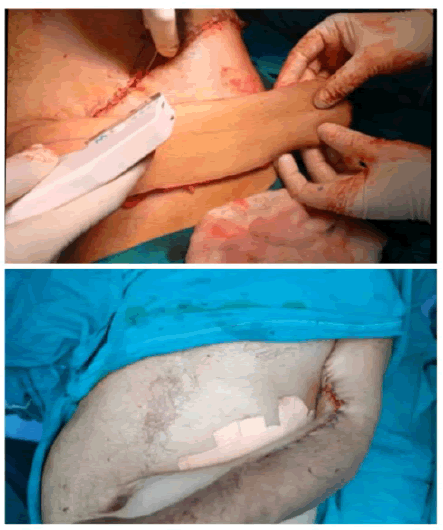
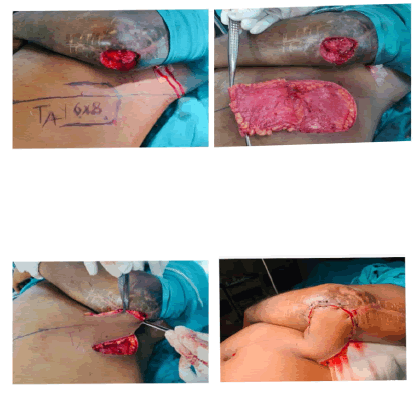
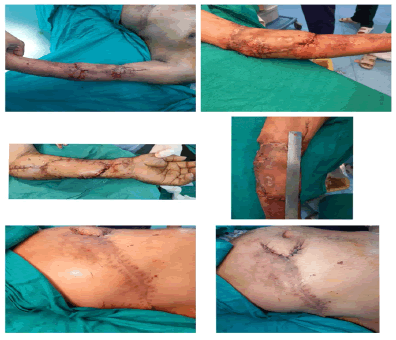
All cases were done under general anesthesia. A sandbag is placed under the ribs on the same side. The flap’s axis was marked as a line extending superiorly and laterally from a point two cm lateral to the umbilicus to the tip of the scapula (Figure 1). Two vertical lines were also marked corresponding to the mid-axillary line and posterior-axillary line. A skin pinch test was done to assess the elasticity of the skin and hence the likely closure of the donor site. The flap is raised from distal (axillary lines as a lateral boundary) to proximal (paraumbilical line as a medial boundary). It is elevated just superficial to the underlying musculature, including not only the subdermal plexus but also the less important vessels within the fat and the flimsy fascia overlying the abdominal muscles (elevated in the subscarpa plane). The dissection ceases at any point in time if the flap is found to be adequate in length (Figure 2).
However, if more length of the flap is required, then the dissection continues medially, the rectus muscle is divided and the flap is thus based on the deep inferior epigastric artery only. The surrounding tissues are undermined and the donor site is closed primarily in all cases (Figures 3, 4). The arm is immobilized on the patient's side with the help of dynaplast tape as shown in Figures 3 and 4. The flap division and final inset were performed 3 weeks later 7. The flaps execution are shown in two patients in Figures 5 and 6.
Results
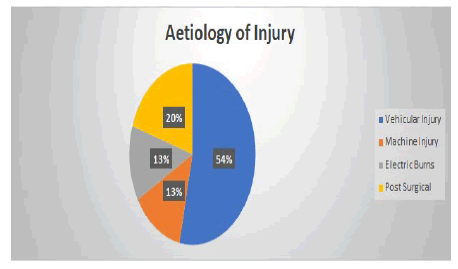
This flap was done on 15 patients. Eleven patients were males and four were females. The age group was 22 years-60 years (Figure 7). Etiology of injury included vehicular accidents in 8 patients, machine injury in 2 patients, electrical burns in 2 patients, and post-surgical in 3 patients. The flap was elevated to the mid-axillary line in 8 patients [7]. In 2 patients, it was raised to the posterior axillary line. The location of the defect included the proximal forearm and elbow region.
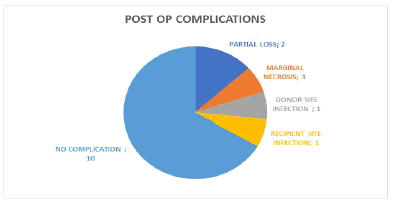
During the initial post-operative follow-up assessment coverage of the wound was satisfactory in all cases, with partial flap loss noted in two cases and marginal necrosis in one case. Partial flap detachment occurred in one case, due to marginal necrosis that required re-suturing. Recipient site infection occurred in one case which was controlled by antibiotics and local wound care (Figure 8). Joint stiffness was seen in all cases during follow-ups but resolved with post-operative physiotherapy.
Donor site infection occurred in one case with partial suture line dehiscence which healed by secondary intention, no split skin grafting was required. The incisional hernia was not seen in any patient during our follow-ups (Figure 9). The flap was technically easy to execute at every step with easy identification of its anatomical landmarks, sub-fascial plane, and draping of the contours of the injured upper limb. The flap was bulky in only one pt. and required a defatting procedure. This flap is usually not bulky as it is transferred from the lateral part of the trunk. Moreover, the majorities of the patients were male farmers or laborers and were quite skinny.
Discussion
A surgical flap is a composite structure of the skin and other tissue. Flap surgery has become one of the most performed surgical procedures in reconstructive surgery. An axial flap is based on a known vessel oriented along the axis of the flap. This flap axiality is imparted by the dominant PUP which arises from the deep inferior epigastric artery as a musculocutaneous perforator. This flap behaves like an axial flap, allowing an advantageous length-to-breadth ratio, and would provide large coverage of soft tissue defects in the upper limb. The versatility of this flap in covering the varied locations extending from the proximal forearm to the elbow to the fingers is due to its axiality imparted by the dominant periumbilical perforator.
The thoraco abdominal flap was first described by Taylor and Boyd [3]. A large flap could be designed in many directions along axis from the umbilicus. The best flap results shown with the flap which was planned along the axis between the umbilicus and the inferior angle of the scapula. The para umbilical perforators could be preserved by including a disc of the anterior rectus sheath together with muscle. Dissection of the vascular pedicle is not necessary for every flap but if required it is performed toward the groin, with or without the rectus muscle. In 1984, Taylor et al. described their clinical experience with 18 patients treated with various combinations of the deep inferior epigastric (thoracoabdominal) flap [8]. We believe that the male preponderance in our study is because males are more exposed to upper limb trauma in our scenario. This is in contrast with the previous study by Yilmaz et al wherein the majority of the patients were females (72.7%) [6]. The operative technique is easy to learn due to its well-defined anatomical landmarks and requires average skill for raising the flap. It is simple, speedy, and safe. Out of the 7 patients whose flaps were elevated to the posterior axillary line, 2 had partial necrosis involving the distal portions. These flaps were re-advanced to provide stable coverage.
This flap is a 'perforator plus’ flap and the base of the flap ontains perforators from the deep inferior epigastric artery that are centered around the periumbilical region [9]. The distal part of the flap is from thoracic skin which is pliable and thin thus extremely suitable for coverage of upper-limb defects. The proximal bulky part tends to settle with time after the final inset. Post-operatively, it did not require strict positioning, the upper limb with the attached flap could be maintained at an elevated level so armrests are in a comfortable position. It also helps in preventing edema and facilitates physiotherapy. It gives more comfort to the patient as compared to the groin flap. In our study, 100% of the flaps were successfully covering the intended areas. Since the majority of our flaps were used for coverage of contaminated wounds, infection was a problem. The pedicle of this flap could neither be tubed nor grafted so discharge from this site was common. However, such complications were usually self-limiting and no flap necrosis was seen.
The donor site closure is done with ease with some tension at the suture line. Donor site closure is possible primarily in all cases.
An unsightly scar in comparison to the groin flap is the main drawback of this flap. In our study, only one patient requested scar revision for cosmetic purposes. The remaining patients were satisfied with the scar. In our study patients were generally unwilling to undergo another surgery for scar revision, as it could be concealed in clothing. All post-operative outcomes are shown in (Figure 9) (after flap detachment).
The groin flap which is based on the superficial circumflex iliac artery is difficult to use for extensive forearm defects due to the inferior and uncomfortable position of the flap. Moreover, the dependent position of the hand harnessed in a groin flap makes it edematous, and post-operative physiotherapy is more cumbersome. The narrow pedicle of the thoracoabdominal flap enables significant comfort for the patient in terms of upperextremity movements. During the waiting period of 3 weeks, the hand is in a better physiologic position than with the groin flap, and early mobilization of the hand is possible with the use of this flap [10].
Conclusion
The thoracoabdominal flap is a useful flap for the coverage of large upper-limb defects especially involving the elbow. A There is no need for extensive dissection and confirm vascular pedicle position and the dissection is quick and systematic. Large flap can be harvested and the donor site closer is possible primarily in the majority of the patients. The hand remains in a comfortable and elevated position postoperatively so there are minimal the groin flap, the majority of our patients accepted the donor scar. This flap becomes the workhorse for upper chances of edema and congestion development. Although the donor site scar is a more visible site in comparison to extremity defects, especially for large defects involving the elbow and forearm, and/or emergency free flap is not possible. It is technically an easy flap and less demanding so it can be raised with ease and speed and it is a reliable flap also due to its pedicled blood supply.
References
- Mishra S, Sharma RK. The pedicled thoraco-umbilical flap: A versatile technique for upper limb coverage. Indian J. Plast. Surg. 2009;42(02):169-75.[Google Scholar]
[CrossRef]
- Taylor GI, Daniel RK. The anatomy of several free flap donor sites. Plast. reconstr. surg. 1975 Sep 1;56(3):243-53.[Google Scholar]
[CrossRef]
- O'Shaughnessy KD, Rawlani V, Hijjawi JB, et al. Oblique pedicled paraumbilical perforator–based flap for reconstruction of complex proximal and mid-forearm defects: a report of two cases J. hand surg 2010;35(7):1105-10.
- Al-Qattan MM, Al-Qattan AM. Defining the indications of pedicled groin and abdominal flaps in hand reconstruction in the current microsurgery era. J. Hand Surg. 2016;41(9):917-27.
- Boyd JB, Taylor GI, Corlett R, et al. The vascular territories of the superior epigastric and the deep inferior epigastric systems. Plast. Reconstr. Surg. 1984;73(1):1-6.
- El-Mrakby HH, Milner RH. The suprafascial course of the direct paraumbilical perforator vessels. Plastic and reconstructive surgery. 2002;109(5):1766-8.
- Ylmaz S, Saydam M, Seven E, et al. Paraumbilical perforator-based pedicled abdominal flap for extensive soft-tissue deficiencies of the forearm and hand. Ann. plast. surg. 2005;54(4):365-8.[GoogleScholar][CrossRef]
- Jones NF, Jarrahy R, Kaufman MR, et al. Pedicled and free radial forearm flaps for reconstruction of the elbow, wrist, and hand. Plastic and reconstructive surgery. 2008;121(3):887-98.[GoogleScholar] [CrossRef]
- Taylor GI, Corlett RJ, Boyd JB, et al. The versatile deep inferior epigastric (inferior rectus abdominis) flap. Br. j. plast.surg. 1984;37(3):330-50..
- Sharma RK, Mehrotra S, Nanda V, et al. The perforator “plus” flap: A simple nomenclature for locoregional perforator-based flaps. Plast. reconstr. surg. 2005;116(6):1838-9.






 Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.
Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.