Role of vertebroplasty for treatment of spinal compression fracture in spinal tumors
2 Aljahra hospital, Ministry of health, Kuwait, Email: dr.tanbolism@gmal.com
3 Professor of orthopaedic surgery, Cairo university, Egypt
4 Professor of orthopaedic surgery, Cairo university, Egypt
5 Assistant Professor of orthopaedic surgery, Cairo university, Egypt
Received: 06-Feb-2023, Manuscript No. jotsrr-23-88744; Editor assigned: 07-Feb-2023, Pre QC No. jotsrr-23-88744 (PQ); Accepted Date: Feb 20, 2023 ; Reviewed: 13-Feb-2023 QC No. jotsrr-23-88744 (Q); Revised: 18-Feb-2023, Manuscript No. jotsrr-23-88744 (R); Published: 21-Feb-2023
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
The spine is one of the essential structures in the human body, and it is the third most common site of abnormal cell proliferation, therefore, prompt evaluation and appropriate management of spinal pain and dysfunction is important. Spinal tumors may cause a variety of symptoms depending on their type, location, and rate of growth. Vertebroplasty is a minimally invasive, radiologically guided procedure that consist of percutaneous injection of a surgical cement into a vertebral body. In this study a total of 20 patients with 49 vertebral compression fractures underwent vertebroplasty at our institution. The aim of this study is to evaluate the role of vertebroplasty in management of o vertebral compression fractures in spine tumors, analysing the clinical and radiographic outcomes using the VAS and the DOI scores. The results were decreasing in VAS score from 8.65 to 1.8, and ODI score was 84.2, decreasing to 17.4 at the last follow-up visit.
Keywords
malignant bone tumors, hemangioma, osteochondroma, osteoid osteomas
Introduction
The spine is a mechanical entity. The spine can be considered a flexible multi-curved column. The shape is important in absorbing energy and protecting against impact. The spine has four major interrelated somewhat disparate functions: support, mobility, protection, and control. The spine supports the internal organs, the upper and lower extremities, the trunk, the head and external load moments [1].
Mobility is required for the many physical tasks of daily living, which tend to complicate the spine structure. The basic functional unit of the spine is termed the motion segment. The spine architectures also serve to protect the spinal cord and nerves. The facet joints are essential to the control of normal motion, and they also serve as a constraint because of their orientation. Thus the motion of each segment is controlled actively by muscles and passively by ligaments [1]. In a normal erect spine, there are four sagittal curves that balance one another: cervical lordosis, thoracic kyphosis, lumbar lordosis and the sacral kyphosis. Kyphotic deformities occur when either of these elements is disrupted [2].
The vertebral body is the primary anterior structure resisting anterior compressive forces. Any factor that compromise the integrity of the vertebral body. E.g., osteoporosis, tumor, infection, or trauma, will have a tendency to promote Kyphotic deformities [1,2]. Compression fracture is the common failure mode of vertebral disc complex in severe axial loading [3-6].
When considering oncologic conditions, the spine is the third most common site of abnormal cell proliferation, therefore, prompt evaluation and appropriate management of spinal pain and dysfunction is important [3].
The tumors involve the bony vertebral column and are usually metastatic. The most common metastatic spinal tumors in women are from the breast and lung while in men, they are most often from the prostate and lung [7]. Tumors arising from bone and cartilage cells do occur in the spine, although with less frequency. Osteogenic sarcoma, lymphoma, multiple myeloma are a malignant bone tumors. Hemangioma, osteochondroma and Osteoid osteomas are benign [8,9].
Of all primary spinal tumors, the majority (50%) involves the thoracic spinal canal, while the remainder affects the lumbosacral spine and cervical spine (30% and 20% respectively). Most spinal tumors present insidiously with symptoms including pain, unilateral motor weakness, sensory loss, and autonomic dysfunction [10].
The philosophy of management of patients with bone metastasis is by nature palliation. This encompasses preservation of function, pain control, spinal stability and, if possible, preventing the development of further pathological fracture [9]. The major indication for percutaneous vertebroplasty is the treatment of symptomatic osteoporotic or neoplastic vertebral body compression fracture(s) refractory to medical therapy [10].
Percutaneous vertebroplasty is a minimally invasive, radiologically guided procedure that consists of percutaneous injection of surgical cement (usually Polymethylmethacrylate PMMA) into a vertebral body. First described by Galibert [11], to treat a C2 hemangioma, it has been used to treat a variety of other pathologies because of its ability to reduce pain and to strengthen and stabilize the bone [12].
Method
We performed a prospective analysis of 20 patients treated with vertebroplasty at our institution. They had VCFs at levels C3 to L5 due to osteolytic lesion arising from primary spinal tumors and secondary metastatic tumors. There were 49 VCFs in these 20 patients.
The goals of this study were to determine the safety and effectiveness of vertebroplasty in improving vertebral body height, decreasing pain, and improving function. The study included 20 patients (12 male, 8 female) with a follow up of 12 months. The median age was 57years (range 33 years – 75 years). Subjects were excluded if they had associated spinal stenosis, neurologic deficit, an active infection, and severe comorbidities such as uncorrected coagulopathy
Preoperatively all the patients were evaluated using a standardized sheet and the findings were tabulated as preoperative clinical and radiological data. Physical examination combined with lateral radiographs, magnetic resonance imaging and computerized tomography were used to diagnose vertebral body compression fractures.
From Twenty patients, diagnosis was painful vertebral Haemangioma in 3 cases (15%), multiple myeloma 8 cases (40%), metastatic breast 4 cases (20%), metastatic bronchogenic carcinoma 3 cases (15%), nonhodgkin lymphoma 1 case (5%), adenocarcinoma of unknown origin one case (5%).
Inclusion Criteria
1. Patients with low back pain due to osteolytic lesions.
2. Acute vertebral fractures in malignant vertebral primary tumors (e.g myeloma) or metastases.
3. Painful or aggressive hemangiomas
Exclusion criteria
1. Vertebral fractures due to osteoporosis, or high energy trauma
2. Neurological deficit, radicular pain, spinal cord compression, or canal compromised
3. Patients taking uninterruptible anticoagulation therapy
4. Sepsis
All patients were treated by percutaneous Vertebroplasty under local infiltration (14 cases) or general anaesthesia (6 cases).
Procedure
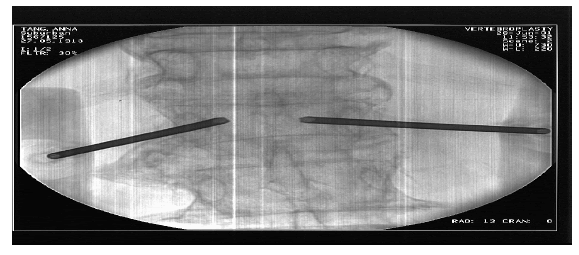
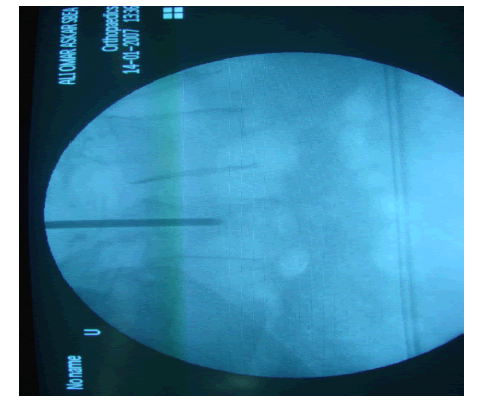
Localize the vertebral body level prior to prepping the skin, anesthetize skin and subcutaneous tissues down to the level of the periosteum. Use transpedicular approach Needle Insertion: Locate bony landmarks and advance needle to desired location within the vertebral body using imaging guidance (Figure 1).
Transpedicular Approach
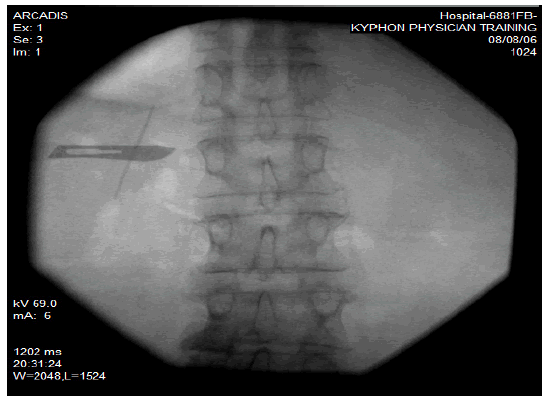
Use fluoroscopy to locate the pedicle cutaneously. Place a small incision lateral and superior to the cutaneous pedicle location. This will allow proper convergence through the tissues to the pedicle entry point (Figure 2).
The pedicle is punctured in its most lateral portion using disposable Jamshidi-type needle.
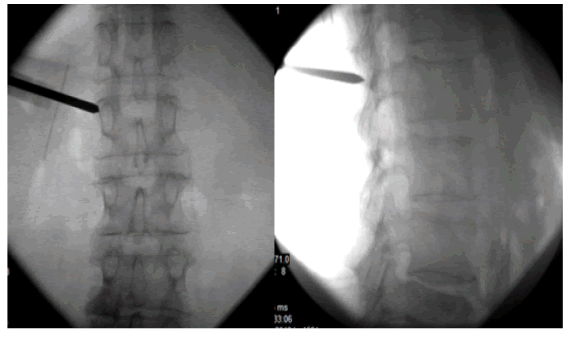
Switch to a lateral view to verify needle trajectory and position (Figure 3). Return to AP view and advance the tip of the needle past the posterior cortical margin (Fig. 4).
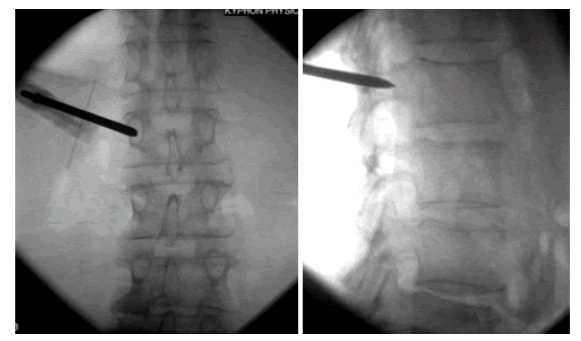
Optimal needle placement in the anterior third of the vertebral body. Rotate the handle of the introducer tool counterclockwise and pull straight out to remove inner stylet (Figure 5).
Cement Mixing & Injection
Meticulous fluoroscopic monitoring during the injection process. Liquefied cement is injected into the vertebral body.
Termination Of Injection
1. Cement in posterior 1/3 vertebral body on lateral projection.
2. Cement extruding into epidural, foraminal or paraspinal veins.
3. Significant disk space penetration
4. Posterior 1/3
Results
A total of 20 patients with 49 VCFs underwent vertebroplasty at our institution from Feb 2014 to Jun 2015. The study population included (12) male (60%) and (8) female (40%). The median age of the patients was 57 years (range 33 years – 75 years). The follow up period was 12month.
The causes of injury were either simple fall on the ground in (7) patients (35%), (2) patients (10%) gave a history of lifting heavy object preceding their feeling of pain and (11) patients (55%) developed sudden onset of pain without precipitating incident.
4 patients (20%) presented with a history of fracture of less than 10 days whereas (11) patients (55%) gave a history of fracture from 10 days - 30 days. (2) Patients (10%) presented with a history of fracture from 30-40 days. Note that in (3) patients (15%), the exact age of fracture couldn’t be estimated.
In (5) patients (25%), one level fracture were treated, in (5) patients (25%) two levels were treated. In (1) patient (5%), three levels were treated. In (6) patients (30%), four level fracture were treated and in (3) patients (15%) five levels were treated. There were 12 patients (60%) had Primary malignant tumor,5 patients (25%) had metastatic origin. The remainder 3 patients (15%) were assumed to have haemangioma.
Note that the largest concentration of fractures was in the thoracolumbar junction where T12 revealed (7) fractures (13.7%), L1 sustained (9) fractures (17.6%) and L2 revealed 9 fractures.
(17.6%). L3 revealed 7 fractures (13.7% and L4 revealed 7 fractures (13.7%).
(6) Interventions (30%) were performed under intubation and (14) patients (70%) were operated on with local anaesthetics in combination with IV sedation.
All patients had mobilized within the first 48 hrs after su rg ery. (14) Patients (70%) were hospitalized for 1 days – 3 days. and (6) patients (30%) stayed for a maximum of 10 days.
The Clinical Outcomes
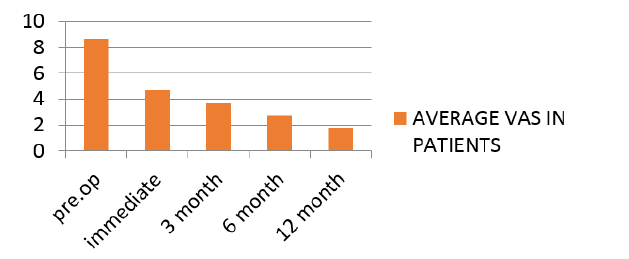
The mean visual analogue scale preoperative was 8.65, decreasing to 4.7 after the procedure and 1.8 at the last follow-up visit (Figure 6).
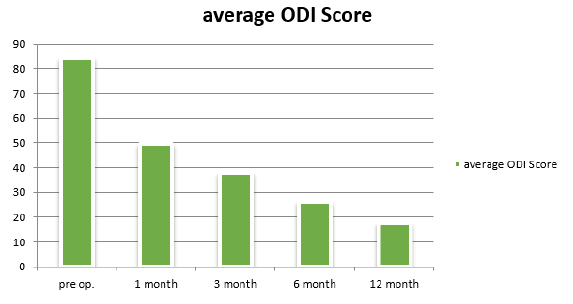
The average ODI score preoperative was 84.2, decreasing to 49.65after one month and 17.4 at the last follow-up visit (Figure 7)
COMPLICATIONS
Operativecomplications: The operation was done in 20 patients; we noted no general complications, particularly no pulmonary emboli caused by acrylic cement.
Cement Leakage: From twenty patients underwent PV, extra- osseous cement leakage occurred in 35% (7 patients) of total population included in our study, in 65 % no leakage occurred (13- patients). Leakage occurred in 7 cases (35%) probably due to less anatomical barriers caused by tumor extension. Cement may leak into a large variety of anatomical compartments, four sites were reported in our study including:-
1. Intervertebral disc (2 cases)
2. Venous cement leakage:
• Paravertebral veins (2 cases) & Epidural veins (one case)
1. Needle track (one case).
2. Paravertebral soft tissue (4 cases).
4 patients developed post-operative nerve root symptoms (L3, L4 radiculopathy) caused by cement leakage. In two cases the symptoms disappeared overnight after treatment with intravenous steroids. The second two cases resolved after 2 months.
Complications related to original disease 4 patients died from the original malignant disease:
1. M.myeloma: 3 cases after 4M, 9M% one year following the procedure.
2. Bronchogenic carcinoma one case after one year.
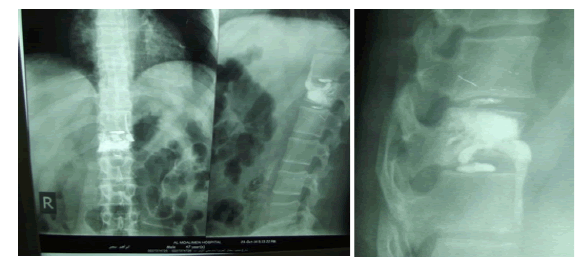
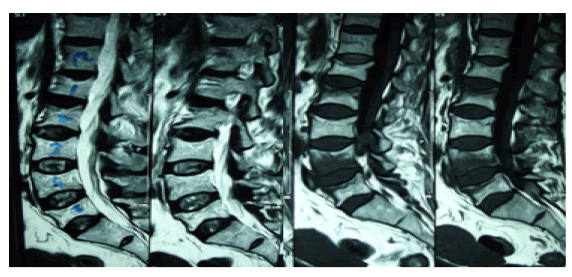
CASE NO. 1
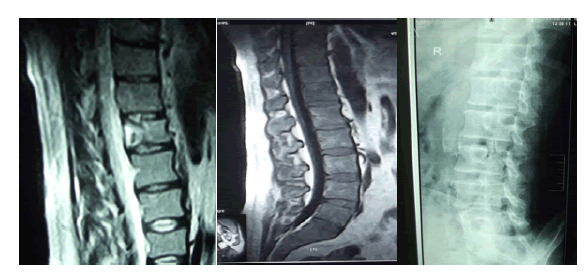
Male patient 47 years old, low back pain after lifting heavy object since 10 days back, multiple myeloma with fracture d12. The preoperative vas 8 and odi 80. Vertebrplasty done VAS was 3 and 1 after 12 months. ODI 34 postoperative and 1 after 12 m. Disc leakage with no complication (Figure 8,9).
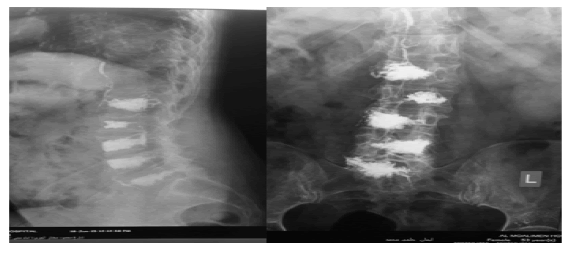
CASE NO. 2
Female patient 52 years old, complaining of low back pain since 3 week with no obvious cause. Her diagnosis was non-hodgkin lymphoma on chemotherapy with wedge fracture of L1 till L5
Preop. VAS 9 & ODI 90. Vertebrplasty L1 to L5 done the VAS changed (Figure 10,11).
Discussion
Pathological Vertebral Compression Fracture (VCF) due to spinal tumors can cause severe complications, including intractable pain, deformities of the vertebral bodies, and neurological complications, and is therefore associated with increased morbidity and mortality [13-15]
Percutaneous vertebroplasty is an effective, minimally invasive procedure that is used to relieve pain and stabilize spine fractures caused by severe osteoporosis or tumors Metastasis [16]. Vertebral tumors are often asymptomatic; however, the presence of a pathologic fracture secondary to vertebral destruction, or the development of spinal instability from such a fracture, may be the origin of pain and neurological symptoms [17]. The t reatment o f t hese p atients i s controversial and must be integrated into the overall management of the cancer patient. Conventional therapy for painful spinal metastasis consists of bedrest, bracing, radiation therapy and pain medication [18]
Chronic pain, usually following multiple vertebral fractures, tends not to respond to the management strategies used for acute pain. The source of chronic pain after vertebral compression fracture is not thought to be the vertebra itself, but is believed to relate predominantly to strain on muscles and ligaments secondary to kyphosis [19].
ercutaneous vertebroplasty consists in percutaneous injection under fluoroscopy guidance of PMMA through a needle into a weakened vertebral body. This procedure tries to solve the problem in the management of a selected group of patients with a metastatic disease that lacks a clear treatment option at this moment. In most patients in our group, surgery was not considered because of the extension of the disease and a short life expectancy. The procedure allowed the patients to stand without pain, to decrease the dose of morphinics and to leave hospital promptly [20].
PV has demonstrated an immediate analgesic efficacy in 90% of the patients in our series. An excellent result (with a VAS of 3 or less) was obtained in 67% of the cases. The results were stable over time. These data are similar to other previously reported results [14, 16, 21, and 22]
The key to safe performance of PV is recognizing that therapeutic response is not related to the degree of filling, but is related to the risk of complications. It is important to understand that there is no relationship between the degree of vertebral body filling and the likelihood of achieving pain relief in these patients [14,21]. Pain relief after PV was rapid and evident within the first week after the procedure. The pain relief was sustained for up to 12 months after the procedure. The majority of patients also reported a return to pre-fracture functional levels. This effect was shown by at least a 4-point decrease in the VAS pain score in 16 (80%) patients achieved dramatic post-operative improvement whereas, in three cases, significant improvement was noted at 6 months follow- up.
The rapid and marked improvements in quality of life scores (ODI score) in this study the average preoperative ODI score was 84.2, decreasing to 49.65 at 1 month postoperatively, and improving to 37.8 and 17.4 at 3-month and last follow- up, respectively.
From our point of view, the most important finding is that 80% of non-ambulatory patients became ambulatory after the PV procedure. These results are very nearly similar to those reported in the literature for patients treated with radiotherapy or surgery [23-24]. However, complication rate and in-hospital days compare favourably with other surgical reports [25].
Conclusion
Our study demonstrates that PV is a successful technique for pain management and consolidation of pathologic vertebral bodies leads to substantial functional improvement with a very low rate of complications. The most critical elements for successful vertebroplasty are: proper patient selection, correct needle placement, good timing of cement injection, strict fluoroscopic control of injection, and operator’s experience
References
- Berlemann U, Franz T, Orler R, Heini PF. Kyphoplasty for treatment of osteoporotic vertebral fractures: a prospective non-randomized study. Eur Spine J. 2004;13:496-501.
- Garfin SR, Yuan HA, Reiley MA. New technologies in spine: kyphoplasty and vertebroplasty for the treatment of painful osteoporotic compression fractures. Spine. 2001; 26(14):1511-5.
- Spinazze S, Caraceni A, Schrijvers D. Epidural spinal cord compression. Critical reviews in oncology/hematology. 2005; 56(3):397-406.
- Binning MJ, Gottfried ON, Klimo P, Schmidt MH. Minimally invasive treatments for metastatic tumors of the spine. Neurosurgery Clinics. 2004; 15(4):459-65.
- Fourney DR, Schomer DF, Nader R, et al. Percutaneous vertebroplasty and kyphoplasty for painful vertebral body fractures in cancer patients. J Neurosurg: Spine, 2003; 98(1):21-30.
- Barr J. Re: Percutaneous Vertebroplasty for Pain Relief and Spinal Stabilization (Spine 2000; 25: 923–8). Spine. 2000; 25(22):2969.
- Lussier D, Huskey AG, Portenoy RK. Adjuvant analgesics in cancer pain management. The oncologist. 2004; 9(5):571-91.
- Prasad D, Schiff D. Malignant spinal-cord compression. lancet oncol. 2005; 6(1):15-24.
- Cole JS, Patchell RA. Metastatic epidural spinal cord compression. The Lancet Neurology. 2008; 7(5):459-66.
- Gayed I, Vu T, Johnson M, et al. Comparison of bone and 2-deoxy-2-[18F] fluoro-D-glucose positron emission tomography in the evaluation of bony metastases in lung cancer. Molecular Imaging & Biology. 2003; 5(1):26-31.
- Grados F, Depriester C, Cayrolle G, et al. Long-term observations of vertebral osteoporotic fractures treated by percutaneous vertebroplasty. SAS Journal. 2009; 3(3):118-22.
- Fourney DR, Schomer DF, Nader R, et al. Percutaneous vertebroplasty and kyphoplasty for painful vertebral body fractures in cancer patients. J Neurosurg: Spine. 2003; 98(1):21-30.
- McGraw JK, Cardella J, Barr JD, et al. Society of Interventional Radiology Standards of Practice Committee. Society of Interventional Radiology quality improvement guidelines for percutaneous vertebroplasty. J Vasc Interv Radiol. 2003; 14(9):S311-5.
- Cotten A, Dewatre F, Cortet B, et al. Percutaneous vertebroplasty for osteolytic metastases and myeloma: effects of the percentage of lesion filling and the leakage of methyl methacrylate at clinical follow-up. Radiology. 1996; 200(2):525-30.
- Lieberman I, Reinhardt MK. Vertebroplasty and kyphoplasty for osteolytic vertebral collapse. Clin Orthop Relat Res. 2003; 415:S176-86.
- Barr JD, Barr MS, Lemley TJ, et al. Percutaneous vertebroplasty for pain relief and spinal stabilization. Spine. 2000; 25:923-8.
- Cook DJ, Guyatt GH, Adachi JD, et al. Quality of life issues in women with vertebral fractures due to osteoporosis. Arthritis Rheum: Off J Am Coll Rheumatol. 1993; 36(6):750-6.
- Yimin Y, Zhiwei R, Wei M, et al. Current status of percutaneous vertebroplasty and percutaneous kyphoplasty–a review. int med j exp clin res. 2013; 19:826.
- Fourney DR, Schomer DF, Nader R, et al. Percutaneous vertebroplasty and kyphoplasty for painful vertebral body fractures in cancer patients. J Neurosurg: Spine. 2003; 98(1):21-30.
- Jones JO, Bruel BM, Vattam SR. Management of painful vertebral hemangiomas with kyphoplasty: a report of two cases and a literature review. Pain physician. 2009; 12(4):E297.
- Cortet B, Cotten A, Boutry N, et al. Percutaneous vertebroplasty in patients with multiple metastases or multiple myeloma. Rev Rhum Engl Ed 64:177–183
- Martin JB, Jean B, Sugiu KS, et al. Vertebroplasty: clinical experience and follow-up results. Bone. 1999; 25(2):11S-5S.
- Chataigner H, Onimus M. Surgery in spinal metastasis without spinal cord compression: indications and strategy related to the risk of recurrence. Eur Spine J. 2000; 9(6):523-7.
- Weigel B, Maghsudi M, Neumann C, et al. Surgical management of symptomatic spinal metastases: postoperative outcome and quality of life. Spine. 1999; 24(21):2240.
[Google Scholar] [CrossRef]
- Pascal-Moussellard H, Broc G, Pointillart V, et al. Complications of vertebral metastasis surgery. Eur Spine J. 1998; 7:438-44.



 Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.
Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.