Severity of flatfoot and hallux valgus deformities: Is there a correlation?
Received: 07-Apr-2023, Manuscript No. jotsrr-23-94840; Editor assigned: 09-Apr-2023, Pre QC No. jotsrr-23-94840 (PQ); Accepted Date: Apr 22, 2023 ; Reviewed: 12-Apr-2023 QC No. jotsrr-23-94840 (Q); Revised: 18-Apr-2023, Manuscript No. jotsrr-23-94840 (R); Published: 23-Apr-2023
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Introduction: Hallux Valgus (HV) is a dynamic foot deformity. The biomechanical factors are not completely understood. Recently, a relation between medial foot arch collapse, with subsequent foot pronation and excessive pressure on the first metatarsophalangeal joint, and HV deformity has been investigated. Therefore, in this study we aim establish a relation between the severity of HV and flatfoot deformities.
Methods: We retrospectively reviewed the preoperative upright foot radiographs of patients submitted to HV surgical correction and measured the Intermetatarsal (IM), HV, Meary’s and Medial Arch (MA) angles. Re-intervention cases were excluded.
Results: 131 feet from 120 patients were evaluated. There was a moderate, positive correlation between IM and Lateral Meary’s angles and also between IM and MA angles. As expected, IM and HV angles were strongly correlated, as were MA and Lateral Meary’s angles. In addition, flatfoot prevalence varied significantly according to HV severity.
Discussion: There isn’t a clear consensus on this matter in current literature. The authors did not find strong recommendations in favour of treating both deformities simultaneously in order to prevent progression or recurrence of any of them. Standard weight bearing radiographs are important to achieve a global foot evaluation and diagnose associated deformities and to establish an adequate surgical strategy.
Conclusion: Our findings support a moderate association between the severity of HV and flatfoot deformities. Regarding treatment strategies, larger biomechanical and clinical randomized controlled studies are needed to establish more reliable conclusions.
Keywords
Hallux valgus, flatfoot, foot deformities, pes planus
Introduction
Hallux Valgus (HV) is a common dynamic deformity of the foot, whose etiology and pathogenesis still remain unclear and are thought to be multifactorial.
HV is a complex triplanar deformity, characterized by first ray instability which leads to dorsomedial deviation and pronation of the first metatarsus, associated with bunion formation [1].
Flatfoot deformity occurs with loss of the hindfoot medial arch, and although often asymptomatic, sometimes can be associated with pain and important loss of function [2-3].
Over the years, a relationship between medial arch collapse and hindfoot valgus, characteristic of flatfoot, with subsequent foot pronation and excessive pressure on the first metatarsophalangeal joint, and HV deformity has been investigated [1,3]. The Grand Rapids arch collapse model describes a link between HV and flatfoot, due to hypermobility of the first ray which leads to bunion formation and medial arch collapse [4]. Moreover, in 1974, Inman stated that flatfoot is a major cause of hallux valgus [5].
However, Mann and Coughlin suggest there is but a minor association, while other authors deny any relation between these deformities whatsoever [6, 7].
Therefore, in this study we aim establish a relation between the severity of HV and flatfoot deformities.
Methods
In a retrospective observational study, we evaluated all patients submitted to hallux valgus correction surgery between 2016 and 2017 at a single center. All patients with previous surgical foot procedures and/or foot fractures, except for phalangeal fractures, were excluded. All subjects underwent preoperative upright foot radiographs and the following angles were measured [3,8-10]:
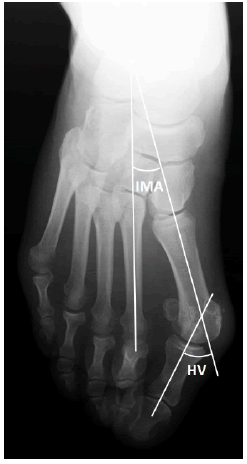
•Intermetatarsal (IM) angle: formed between the intersection of 2 lines drawn along the longitudinal axes of the first and second metatarsals (Fig. 1).
•Hallux Valgus (HV) angle: given by the intersection of a line drawn along the longitudinal axis of the first metatarsal and a line drawn along the longitudinal axis of the proximal phalanx (Fig. 1).
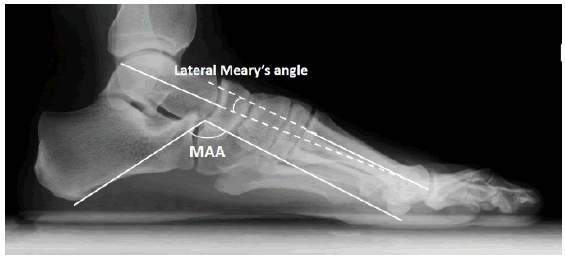
•Lateral Meary’s angle: obtained by measuring the angle between a line traced along the central longitudinal talar axis and a second line through the anatomic axis of the first metatarsal (Fig. 2).
•Medial arch (MA) angle (also called Costa-Bartani angle): formed between a line drawn from the lowest point of the sesamoid to the lowest point of the talonavicular joint and a line passing from the lowest point of the talonavicular joint to the lowest point of the calcaneus (Fig. 2).
For the current work, the radiological definition of flatfoot of a Lateral Meary’s angle>9º was considered [11, 12].
The authors defined 3 groups of patients according to HV severity: mild HV defined by HV angle <13º, moderate HV between 13º and 15º, and HV angles >15º were included in the severe HV group.
For statistical analysis, Statistical Package for the Social Sciences (SPSS) ®, IBM, Chicago, Illinois, USA, version 22.0 was used. Results were considered statistically significant for p<.05, with a confidence interval of 95%.
For all continuous variables, measures of the mean and Standard Deviation (SD) were obtained and preliminary analyses were performed to ensure no violation of the assumptions of normality, linearity and homoscedasticity. For correlation between angles, Pearson productmoment correlation coefficient was used and for comparison between groups, Chi-squared test for independence and one-way betweengroups Analysis of Variance (one-way ANOVA), its corresponding effect size measures (Cramer’s V and eta squared) and Tukey (Honestly Significant Difference) HSD test for post-hoc comparisons were used.
Results
Out of 183 feet, after applying the exclusion criteria, a total of 131 feet from 120 patients were evaluated.
Patients’ mean age was 51.5 years (SD=13.91). The average HV and IM angles were 30.82º (SD=8.91) and 13.01º (SD=3.32), respectively. Concerning pes planus evaluation, Meary’s and MA angles were 8.77º (SD= 4.87) and 126.21º (SD=6.49), respectively (Table 1).
Table 1. Foot radiographic evaluation
| n = 131 | Mean (SD) |
|---|---|
| Hallux Valgus Angle | 30.82º (8.91) |
| Intermetatarsal Angle | 13.01º (3.32) |
| Lateral Meary’s Angle | 8.77º (4.87) |
| Medial Arch Angle | 126.21º (6.49) |
After applying Pearson product-moment correlation coefficient, we found a moderate, positive correlation between IM and Lateral Meary’s angles (r=0.314, n = 131, p < .0005) and also between IM and MA angles (r= .299, n=131, p<.001). Thus, larger IM angles were associated with higher MA and Lateral Meary’s angles. As expected, IM and HV angles (r =0.524, n = 131, p< .0001) showed a strong, positive correlation, as did MA and Lateral Meary’s angles (r = .644, n = 131, p < .0001).
In addition, pes planus prevalence varied significantly according to HV severity (Table 2). A Chi-square test for independence indicated a positive association with a moderate effect size between HV severity and flat foot prevalence, χ2 (2, n=131) = 9.188, p< .05, Cramer’s V= 0.265.
Table 2. Pes planus prevalence according to HV severity
| Intermetatarsal angle | Lateral Meary’s angle Mean (SD) | Pes planus prevalence (%) |
|---|---|---|
| Mild: <13° | 7.07° (3.83) | 0.25 |
| Moderate: 13-15° | 10.39° (5.60) | 0.488 |
| Severe: >15° | 9.67° (4.72) | 0.533 |
A one-way ANOVA was conducted to explore the impact of HV deformity severity on Lateral Meary’s and MA angles. There was a statistically significant difference in Lateral Meary’s and MA angles for the three HV severity groups: Welch’s F (2, 65.127) = 7.761, p< .001 and F (2, 128)=7.063, p < .05, respectively. Furthermore, the actual difference in mean scores between the groups was notable, as the effect sizes, calculated using eta squared, were 0.11 and 0.10 (moderately large), respectively. Post-hoc comparisons using the Tukey HSD test indicated that the mean Meary’s and MA angles for the mild HV group (mean =7lll l.07, SD = 3.83 and mean=124.00, SD=5.29, respectively) were significantly different from the moderate HV (mean=10.39, SD=5.60 and mean=127.98, SD=7.10, respectively) and severe HV (mean = 9.67, SD =4.72 and mean =128.23, SD=6.60, respectively) groups. Moderate HV group did not differ significantly from severe HV group.
Discussion
The intra and inter observer reliability and validity of the parameters measured in the present study have been considered exceptionally reliable, with intraclass correlation coefficients ranging from 0.73-0.98 [10,13, 14]. In literature, there are numerous indexes to evaluate flatfoot deformity. Nevertheless, some authors have stated that lateral Meary’s angle is constant irrespective of the different pes planus patterns, reflecting only the severity of the overall medial-arch sag [11].
Kim et al. studied the relationship between HV and hindfoot alignment in the paediatric population (patients with open physes), and showed moderate correlations between Lateral Meary’s angle and HV angle (r=0.210, P = .007) and IM angle (r=0.373; P <.001). Despite being a different age group, the results are similar to the ones obtained in our study [10].
Our results, are also in agreement with the findings of Cheney et al. who evaluated the severity of HV deformity in patients with flatfoot [15]. Indeed, they found a correlation between the severity of the flatfoot and the severity of the bunion deformity defined by the sesamoid position, HV angle and IM angle.
Although not completely established in literature, some authors have hypothesised a biomechanical mechanism to explain the relation between the two deformities. Continuous ligamentous stretching of medial arch’ support, with progression to spring ligament complex attenuation, leads to an unstable medial column and subsequent hindfoot valgus. As the first ray becomes more mobile, primarily in the dorsomedial plane, the sesamoids become increasingly displaced, which leads to the third plane of metatarsus deformity, that is pronation. This rotational deformity seems to correlate with first ray instability combined with medial arch collapse [1,16]. Recent findings suggest that the first metatarsalcuneiform angle, which represents motion/instability and orientation of this joint, and naviculocuboid overlap were increased in patients with HV, when compared with controls which further corroborates this hypothesis. In light of these findings, King et al. recommend a clinical and radiological (weightbearing) evaluation of first ray mobility in all patients with HV [10,17, 18].
An association between HV and flatfoot deformity is of major importance because it may have essential clinical implications. Faldini et al. have reported favorable radiological and functional outcomes when treating simultaneously the HV and flat foot deformity in thrirtytwo children, combining subtalar arthroereisis and a distal metatarsal osteotomy [19].
Takao et al. performed a proximal oblique-domed first metatarsal osteotomy in order to correct both HV and flatfoot deformities in the same procedure, with significant radiological improvements postoperatively [20]. Others have associated a medial sliding calcaneal osteotomy to correct flatfoot deformity in patients submitted to HV correction surgery, and report no HV recurrence [21].
Studies that evaluate the simultaneous treatment options of HV and flatfoot deformities are limited in literature, most of which with few patients. Therefore, the authors did not find strong recommendations in favour of treating both deformities simultaneously in order to prevent progression or recurrence of any of them.
The present work suggests an association between HV and flatfoot deformities, although a causal relation isn’t confirmed at this stage. We can however recommend a global analysis of weightbearing radiographs and a careful physical examination, in order to diagnose concomitant deformities which may alter the surgical strategy.
Conclusion
In conclusion, we believe there is an association between HV and flatfoot deformities in the adult age. Standard weight bearing radiographs are important to achieve a global foot evaluation and diagnose associated deformities and to establish an adequate surgical strategy.
We believe our findings may have clinical significance and be a warning for the importance of searching for associated deformities, which may modify subsequent treatment and improve clinical outcomes.
Hence, biomechanical and clinical randomized controlled studies with larger populations are needed to establish more reliable conclusions, with higher statistical power.
References
- Blackwood S, Gossett L. Hallux valgus/medial column instability and their relationship with posterior tibial tendon dysfunction. Foot ankle clin.. 2018;23(2):297-313. [Google Scholar] [Cross ref]
- Taha AM, Feldman DS. Painful flexible flatfoot. Foot ankle clin.. 2015;20(4):693-704. [Google Scholar] [Cross ref]
- Lin YC, Kwon JY, Ghorbanhoseini M, et al. The hindfoot arch: what role does the imager play?. Radiol. Clin.. 2016 ;54(5):951-68. [Google Scholar] [Cross ref]
- Burkard D, Patton D, Padley M, et al Statistical Validation of the Grand Rapids Arch Collapse Classification. Foot Ankle Orthop.. 2019;4(2):2473011419834531. [Google Scholar] [Cross ref]
- Inman VT. Hallux valgus: a review of etiologic factors. Orthop. Clin. N. Am.. 1974;5(1):59-66. [Google Scholar] [Cross ref]
- Mann RA, Coughlin Jj. Hallux valgus—etiology, anatomy, treatment and surgical considerations. Clin. Orthop. Relat. Res. 1981;157:31-41. [Google Scholar] [Cross ref]
- Kilmartin TE, Wallace WA. The significance of pes planus in juvenile hallux valgus. Foot & ankle. 1992;13(2):53-6. [Google Scholar] [Cross ref]
- Lamm BM, Stasko PA, Gesheff MG, et al. Normal foot and ankle radiographic angles, measurements, and reference points. j. foot ankle surg.. 2016;55(5):991-8. [Google Scholar] [Cross ref]
- Lo HC, Chu WC, Wu WK, et al. Comparison of radiological measures for diagnosing flatfoot. Acta Radiologica. 2012;53(2):192-6. [Google Scholar] [Cross ref]
- Kim HW, Park KB, Kwak YH, et al Radiographic assessment of foot alignment in juvenile hallux valgus and its relationship to flatfoot. Foot Ankle Int.. 2019;40(9):1079-86. [Google Scholar] [Cross ref]
- Bourdet C, Seringe R, Adamsbaum C, et al. Flatfoot in children and adolescents. Analysis of imaging findings and therapeutic implications. Orthop. Traumatol.: Surg. Res. 2013;99(1):80-7. [Google Scholar] [Cross ref]
- Keats TE SC. Atlas of Radiologic Measurements. Philadelphia: Mosby; 2001.
- Lee KM, Chung CY, Park MS, et al. Reliability and validity of radiographic measurements in hindfoot varus and valgus. JBJS. 2010 ;92(13):2319-27. [Google Scholar] [Cross ref]
- Lee KM, Ahn S, Chung CY, et al. Reliability and relationship of radiographic measurements in hallux valgus. Clin. Orthop. Relat. Res. 2012;470:2613-21. [Google Scholar] [Cross ref]
- Cheney N, Rockwell K, Long J, et al Is a Flatfoot Associated with a Hallux Valgus Deformity?. Foot Ankle Orthop. 2017 ;2(3):2473011417S000133. [Google Scholar] [Cross ref]
- Chan F, Bowlby MA, Christensen JC. Medial column biomechanics: nonsurgical and surgical implications. Clin. podiatr. med. surg.. 2020 ;37(1):39-51. [Google Scholar] [Cross ref]
- Hatch DJ, Smith A, Fowler T. Radiographic relevance of the distal medial cuneiform angle in hallux valgus assessment. J. Foot Ankle Surg.. 2016 ;55(1):85-9. [Google Scholar] [Cross ref]
- King DM, Toolan BC. Associated deformities and hypermobility in hallux valgus: an investigation with weightbearing radiographs. Foot ankle int.. 2004;25(4):251-5. [Google Scholar] [Cross ref]
- Faldini C, Nanni M, Traina F, et al. Surgical treatment of hallux valgus associated with flexible flatfoot during growing age. Int. orthop.. 2016;40:737-43. [Google Scholar] [Cross ref]
- Takao M, Komatsu F, Oae K, et al. Proximal oblique-domed osteotomy of the first metatarsal for the treatment of hallux valgus associate with flat foot: effect to the correction of the longitudinal arch of the foot. Arch. Orthop. Trauma Surg.. 2007;127:685-90. [Google Scholar] [Cross ref]
- Choi JY, Yoon HH, Suh YM, Suh JS. Surgical correction of hallux valgus complicated with adult-type pes plano-valgus. J. Orthop. Surg.. 2017 ;25(1):2309499016684320. [Google Scholar] [Cross ref]



 Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.
Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.