The role of secondary ossification centers in the management of epiphyseal and apophyseal fractures
Received: 25-May-2017 Accepted Date: Jul 11, 2017 ; Published: 14-Jul-2017
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
The site where bone begins to form in the shaft of a long bone or the body of an irregular bone is called a primary ossification center. The site where bone formation continues after beginning in the long shaft or body of the bone, usually in an epiphysis is a secondary ossification center. A secondary ossification center is the center of bone formation appearing later than the punctum ossificationis primarium, usually in epiphysis. Secondary ossification centers for epiphyses and apophyses go through different stages of growth from the initiation of ossification to complete fusion. This paper will review the development of the secondary ossification centers, the mechanism of injuries, the pathophysiology of physical injuries, clinical diagnosis, investigations, and management. The goal of this review was to illustrate the variance in physeal injuries as they evolve during ossification and fusion. These patterns can be broadly broken down in to pre-ossification, ossification, and pre-fusion. This provides an understanding of particular patterns, mechanisms, diagnosis, and management options.
Keywords
Patellar sleeve injury, Femoral ankle, Medial epicondyle, Tibia tubercle
Introduction
Secondary ossification centers for epiphyses and apophyses go through different stages of growth from the initiation of ossification to complete fusion. This evolution leads to variations in fracture patterns based on mechanism and anatomical location. Consequently, physeal injuries in certain areas can be challenging to evaluate, sometimes leading to incorrect diagnosis and inappropriate management.
These injuries often vary based on location, mechanism, and age. Examples include: non-accidental trauma seen prior to the emergence of secondary ossification centers, young athletes with avulsion injuries prior to fusion across the physis, and transitional ankle injuries that occur during a period of incomplete fusion across the physis. All are examples of variations related to secondary ossification.
This paper will review the development of the secondary ossification centers, the mechanism of injuries, the pathophysiology of physeal injuries, clinical diagnosis, investigations, and management. These will be discussed in three major stages of ossification: pre-ossification, ossification, and pre-fusion. Typical injuries seen involving the secondary ossification will be highlighted in its corresponding stage, with considerations for diagnosis and management included.
General Considerations
At birth, aside from the distal femur epiphysis, all secondary ossification centers (SOCs) consist only of a mass of cartilage. This leads to challenges with visualization as they are not seen plain radiographs [1]. It is through ossification by which we begin to identify these SOCs radiographically.
There are two types of SOCs, the epiphysis and the apophysis. The epiphysis typically forms the end extensions of long bones. Articular cartilage surrounds the epiphysis and typically no attachments for muscles or tendons are seen. The main function is longitudinal growth and facilitation of joint motion [2,3]. The apophysis does not participate in longitudinal growth or joint articulation. The apophysis typically serve as attachments sites for tendons and ligaments, providing function of added force production for movement and stability [1].
Pre-Ossification
As mentioned, the majority of the SOCs are absent at birth, with the exception being the distal femur epiphysis. This poses a problem because often these injuries can be missed or under treated. This is especially important as up to 50% of cases involving the distal humerus and distal femur are related to non-accidental trauma [4]. Other common causes include accidental trauma, falls and motor vehicle collisions.
Distal Humeral Physeal Separation
Mechanism
Distal humeral physeal separation is typically seen in children less than 3 years of age. Often caused by accidental trauma caused by a fall on an outstretched hand or secondary to non-accidental trauma. Usually the mechanism is a hyperextension injury with a rotational force vector [5]. Additionally, these injuries can occur in newborns secondary to difficult deliveries [6]. Although rare, they can often go undiagnosed for prolonged periods of time. Typically, the patient will not move their extremity and has been described as a pseudo paralysis of the limb [7]. The child may likely be irritable depending on the age group, and swelling may be apparent in the limb.
Diagnosis
Difficulty in diagnosis is attributed to the absence of bony landmarks, which may be missed on radiographs. Radiographically it can be difficult to assess as the determination of radiocapitellar alignment is not feasible given the potential absence of the SOC for the radius, ulna and humerus depending on the age [8]. This is especially true in the newborn population. Capitellar SOCs often do not appear until the close to the ninth postnatal month [9], often leading to a misdiagnosis of elbow dislocation. Radiographs will show a loss of relationship between the radioulnar articulation relative to the distal humerus, which can be appreciated in both dislocation and separation. However, radiographs often do not allow for obvious appreciation of the transphyseal separation [6].
Ultrasound imaging better illustrates a physeal separation by identifying a bare area of the distal humerus not covered by epiphyseal cartilage [7]. An important identifier is the posteromedial displacement of the radius and ulna in relation to the distal humerus. Supakul et al. compared radiography vs. ultrasound in diagnosing distal humeral physeal separation. 56% of patients had a missed diagnosis using radiographs, while ultrasound diagnosed a distal humeral physeal separation in 75% patients. Additionally, ultrasound identified bucket handle fractures in 31% of the patients vs. 12.5% with radiographs [7].
MRI has also been indicated in diagnosing distal humeral physeal separation in newborns. Its advantage is clearer depiction of cartilage, bone, and soft tissue and images produced in multiple long axis [6]. Additionally, MRI is considered less painful to the patient and manipulation of the extremity during radiography and ultrasound can be avoided. Potential drawbacks for MRI are the expense and need for the sedation to prevent movement in the scanner [6].
Management
Early identification, reduction and immobilization are the primary goals of treatment. On occasion, a closed reduction with sedation with or without placement of pin fixation is required. Proper identification of these injuries is important to avoid adverse outcomes. Cubitus varus deformity is a common complication with a reported prevalence anywhere from 25% to 75% [10]. Abe et al. looked at 21 cases of distal humeral physeal separations over a long-term follow-up. 15 cases of residual cubitus varus deformity were noted post treatment. In their cohort, 9 patients went on to have osteotomies to correct the deformity [5]. Similarly, De Jager et al. found 3 of 10 patients in their review of distal humeral physeal separation in children ages 10 months to 4 years to have 5 to 10 deg. of residual cubitus varus. Early detection can prevent these undesirable outcomes [11].
Ossification
Distal and Medial Clavicle Physeal Fractures
Physeal injuries involving the clavicle are a less common subset of injuries that occur through the hypertrophic zone after formation of the SOCs. Injuries to the distal and medial clavicle physis are commonly misdiagnosed as acromioclavicular and sternoclavicular dislocations respectively. The distal clavicle physis typically does not fuse until around 18 years of age [12], while the medial clavicle physis is last the physis to fuse in the body, usually around 25 years of age [12]. The distal clavicle physeal mimics an AC joint injury with displacement of the distal clavicle in a superior and posterior direction [12]. However, the coracoclavicular ligaments are not injured, but instead there is a disruption of the physis. With medial clavicle physeal injuries, there is an unprotected area of the physis [12]. The robust sternoclavicular ligaments attach directly to the epiphysis, leaving the physis without capsular protection and susceptible to injury [12].
Mechanism
Both direct and indirect forces to the shoulder cause injuries to the distal clavicle physis. Medial sided injuries should be more concerning for associated sternal injuries by clinicians as they often represent a higher mechanism of injury. Medial sided injuries can displace both anteriorly and posteriorly depending on the direction of force applied. Typically, this is seen with higher energy falls or motor vehicle collisions.
Diagnosis
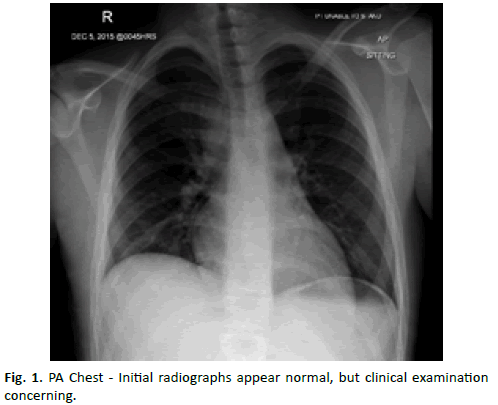
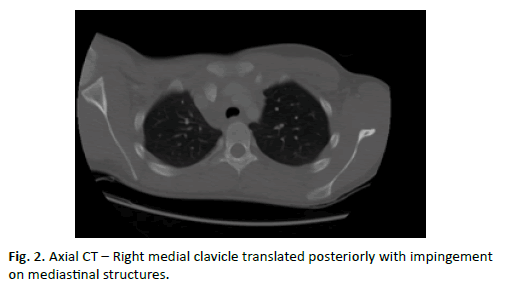
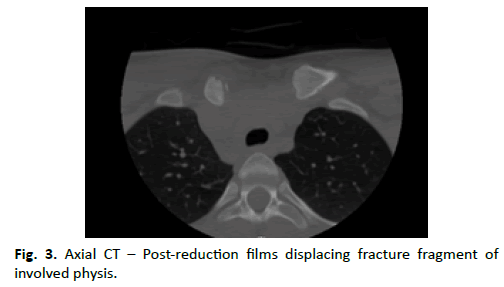
The promptness of diagnosis is especially important with medial injuries given its close proximity to the mediastinum and its contents. For medial clavicle injuries, pain and swelling will be common. Patients may also present with stridor or shortness or both if the direction of physeal displacement is posterior [12]. Radiographs are often obtained first, with upshot cephalad views of the clavicle acquired as well to augment visualization [12]. However, because of the concern displacement in medial injuries, adjuvants such as CT are often obtained. CT provides the most detail regarding fracture morphology, degree of displacement, and imaging of the adjacent intrathoracic structures [12]. Figure. 1 displays a PA view of the chest, which does not visualize the injury; however Figures. 2 and 3 representing select CT cuts further characterize the injury not readily visible on plain radiographs.
Distal clavicle injuries present similar to AC joint mid-shaft clavicle fractures. Pain, swelling, and a palpable prominence may all be seen on physical examination [2]. Additionally, a careful examination of the overlying skin is necessary to rule out open or impending open injuries. Radiographs are usually the only imaging modality indicated here. Again, AC dislocations have similar appearance with or without significant displacement, but here the physis is disrupted.
Management
With distal clavicle physeal injuries the typical management is non-operative with symptom management. However, if there is displacement through the platysma and clavipectoral fascia and the clavicle lies subcutaneous, operative management is recommended [13]. Typically, if there is no significant displacement non-operative management yields favorable results [13].
Medial clavicle physeal injuries are typically more worrisome because of its close proximity to the mediastinal structures [2,12]. With non-displacement injuries, symptom management is indicated. With displaced fractures however, in particular posterior, often a closed reduction under sedation is required initially. If irreducible, an open reduction and internal fixation which yields good results [12].
Medial Epicondyle Fractures
Fractures around the pediatric elbow are often difficult to interpret because of the numerous SOCs present. SOCs typically appear in a predictable manner but inevitably overlap amongst their appearance occurs. The medial epicondyle is considered an apophysis, as it does not contribute to longitudinal growth [14]. The medical epicondyle SOC typically appears between 3-6 years of age for girls and 5-7 years of age for boys [12]. The medial epicondyle is the last SOCs of the elbow to fuse, typically occurs around 15 years of age for girls and 18 years of age for boys [12]. After the emergence of the SOCs, the medical epicondyle is particularly susceptible to injury between the ages of 9-14. Medial epicondyle fractures occur in conjunction with elbow dislocations up to 60% of the time [14]. Additionally, perceived isolated elbow dislocations can miss associated medial epicondyle fractures and more importantly incarcerated fragments, which typically occur 15-25% of the time [14].
Mechanism
Both direct trauma and indirect avulsion mechanism have been described. Often these issues are caused by a fall on a outstretched hand with the position of the elbow in valgus, hyperextension and supination [14]. Clinicians have described a pull by the flexor-pronator mass in the pure avulsion injury, while others comment on the pull by the ulnar collateral ligament with associated dislocations [14].
Diagnosis
Patients typically present with swelling, pain, tenderness and decreased range of motion. A careful neurovascular examination is critical, in particularly the ulnar nerve needs to be assessed for any sort of dysfunction as it can be injured or entrapped with fracture dislocations.
AP, lateral, and 45-degree internal oblique radiographs are recommended for diagnosis. If a fragment appears at the level of the joint line it should be considered incarcerated until proven otherwise [15]. Incarcerated fragments typically lie between the trochlear and semilunar notch of the olecranon [12]. Figures. 4A and 4B illustrate a elbow fracture dislocation with associated medial epicondyle avulsion in a 9 year old boy. Additional signs of fracture include loss of sclerotic margins of apophysis and increased radiolucency in area of apophyseal line [16]. Maximum displacement is best visualized on internal oblique films, with excellent inter and intraobservations in quantifying displacement [14,16]. In cases in which one cannot be certain whether there is an incarcerated fragment after closed reduction, CT or MRI remains viable options.
Treatment
Current treatment is focused on urgent reduction fracturedislocations and ensuring the joint surface is free of incarcerated fragments. The decision for non-operative vs. operative treatment has been evaluated in a number of studies and the indications have evolved over time. One of the traditional indications for operative management was amount of displacement. However, Farsetti et al. discovered comparable long-term results with nonoperatively treated fractures displaced between 5-15 mm compared to operative fixation. Current indications for operative management are incarcerated fragments, entrapped and dysfunctional ulnar nerve, and marked instability [17].
Operative treatment typically yields higher union rates over nonoperative management [18]. However, many studies have found no significant functional difference with between operative and non-operative groups. Alternatively, cases involving incarcerated fragments typically led to more perceived instability, radiographic deformity need for re-operation, up to 18% [15].
Pre-Fusion
Near the end of the growth the initial proliferating chondrocytes in the germinal and proliferating zones mature and decrease in number. This is more commonly seen in males, and marks the timing of oncoming fusion [1]. This is the weakest stage of the physis, and renders it most susceptible to injury [19].
Tibia Tubercle Fractures
The proximal tibia has unique anatomical considerations that predispose to certain injury patterns and populations. The proximal tibia epiphysis and tibia tubercle apophysis have a very close association. Each possesses a SOC, which fuse in a predictable manner. The proximal tibia epiphysis fuses from a posteriormedially to anterior-lateral direction, while the distal tibia apophysis fuses from a proximal to distal direction [20,21]. This creates a relatively weak zone distal in the tibia tubercle apophysis, which may propagate into the proximal tibia epiphysis depending on patient factors and energy of injury.
Mechanism
Fractures of the tibial tubercle typically occur in adolescent athletes between 12-15 years of age. This is more commonly in males and represents less than 1% of pediatric fractures [19]. Knee flexion during quadriceps contraction or quadriceps contraction with an ipsilateral fixed can both can cause an avulsion moment through the tibia tubercle apophysis. These are typically seen during jumping activities, but other high-energy sports such as football, soccer, and running can predispose to this injury. Osgood Schlatter Disease (OSD) has been suggested as a potential risk factor for tibia tubercle avulsion injuries. However. Pretell-mazzini et al. found no statistical significance for presence of OSD with tibia tubercle avulsion injuries [19].
Diagnosis
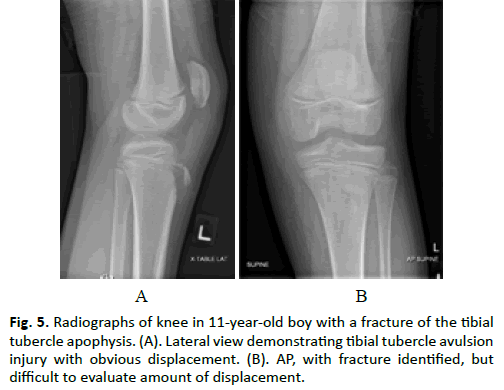
The mainstay of diagnosis remains clinical examination and radiographs. Vascular injuries, particularly the recurrent branch of anterior tibia artery, can cause compartment syndrome with a reported incidence of up to 10% [21]. Therefore, detailed neurovascular examination is paramount. Ogden was the first to categorize these based on fracture location using radiographs [22]. Classically three types were described: fracture of the apophysis near insertion of patellar tendon, fracture proximal to the junction with proximal tibia epiphysis, and fracture extension into proximal tibia epiphysis. Figures. 5A and 5B display a tibial tubercle avulsion fracture in the 10-year-old boy. Notice the injury is difficult to identify on AP, but readily visible on the lateral radiograph. Additionally, studies have shown radiography alone can underrepresent the degree of injury, which has led advocates pushing for advancing imaging in the form of CT and/or MRI [21]. Pandya et al. found up to 80% of their patients had a greater severity of injury identified on CT [21].
Management
Ogden type 1 can typically be managed non-operatively with a period of immobilization and long-leg casting [19]. Ogden types III are typically considered operative candidates. Ogden type II injuries can be managed both non-operatively and operatively depending on the amount of displacement. Operative techniques are typically open procedures with hardware fixation [21]. Open techniques allow for inspection of the articular surface and meniscus. Functional outcomes are very favorable in this cohort of patients, with either operative or non-operative management. Frey et al. reported on 19 of 20 patients returning to sport around 3.9 months post operatively with no functional deficit [23]. Similarly, Pandya et al. reported all patients achieved radiographic union with only 5.5 describing functional deficits [21].
Transitional Ankle Injuries
The transitional ankle injuries, Triplane and Tillaux fractures have typical fracture patterns based on amount and pattern of physeal closure. These injuries typically occur 18 months prior to fusion because of asymmetric physeal closure [24]. Fusion across the distal tibia starts centrally, proceeds anteromedial to posteromedial and finishing laterally. Thus leaving the lateral aspect of the physis weaker and susceptible to injury while the anteromedial epiphysis is stabilized by the presence of Kump’s medial hump [25].
Mechanism
Triplane and Tillaux fractures are typically seen in males and females between the ages of 12 and 16 [26]. The mechanism is an external rotation applied to the foot in the supinated position [26]. Unlike the adult counterparts, failure occurs through the physis. Triplane fractures have extension in the metaphysis while the Tillaux fractures are confined to the epiphysis, often as a result of avulsion to the anterior tibiofibular ligament.
Diagnosis
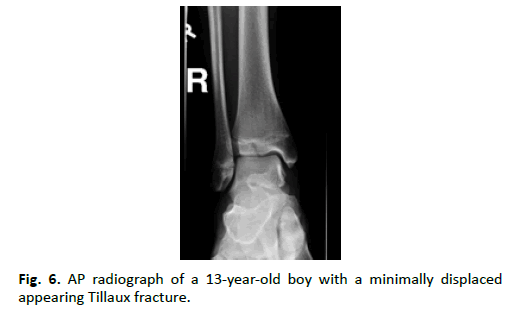
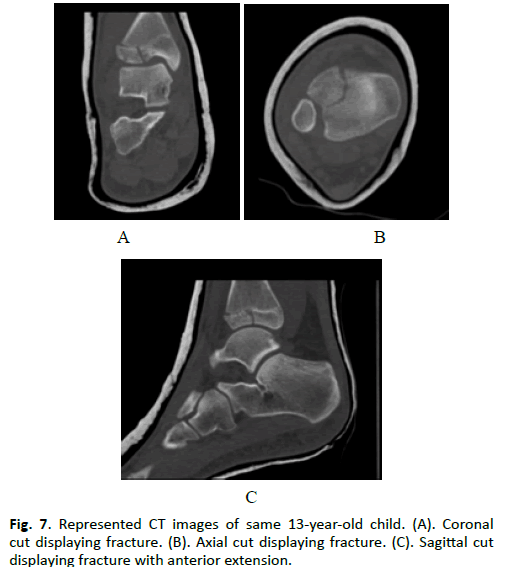
Presence of swelling, ecchymosis, tenderness, and refusal to weight bear should lead clinicians to obtain diagnostic imaging. Radiographs can effectively demonstrate the significant of the injury, however, they are often misdiagnosed using the Salter- Harris classification. Often Triplane fractures are diagnosed as Salter Harris Type IV, however they do not follow the typical convention of this classification, as they are multiplanar. Triplane and Tillaux share a similar a fracture line in the sagittal plane through the epiphysis, which are appreciated on AP radiographs [26]. This fracture propagates through the physis axial plane. Additionally, Triplane fractures extend into the metaphysis in the coronal plane and are appreciated on lateral radiographs. No extension of the fracture fragment posteriorly in the coronal plane distinguishes the two. This gives the Triplane fracture a classic characteristic look of a Salter-Harris III on the AP, and a Salter- Harris II on the lateral radiographs. Figure. 6 displays the AP fracture pattern on radiographs of a 13-year-old sustaining an ankle injury while skateboarding. Fracture fragmentation and displacement may not be readily appreciated on radiographs Adjuvant imaging with CT can be used to further delineate fracture pattern and presence of joint incongruity [27]. Figures. 7A, 7B, and 7C further characterize the same child’s fracture fragment on CT. Intra-articular displacement in particular can be underrepresented on radiographs. Eismann et al. indicated CT was more sensitive at identifying >2 mm articular step deformities. This altered treatment plans from non-operative to operative in 27% of cases. Additionally, choice of fixation was also influenced in up to 41% of cases [28].
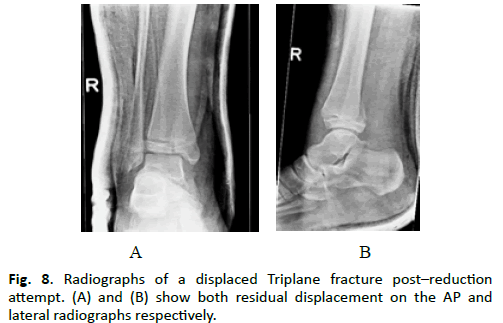
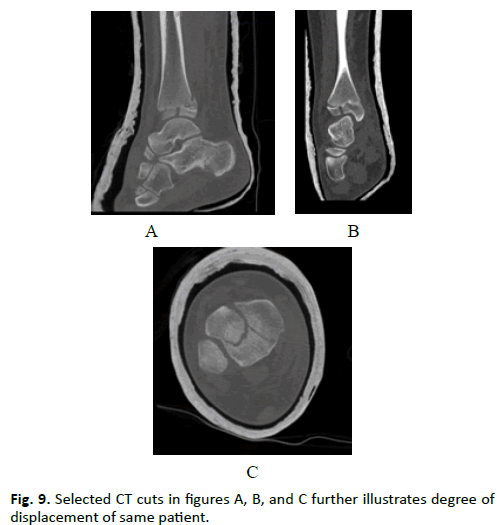
Management
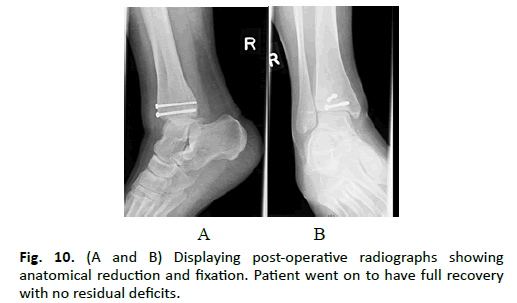
Non-operative management may be utilized for non-displaced fractures or those that were reduced by closed means. Typically, cross-sectional imaging is acquired to further intra-articular incongruity. Residual displacement of >2 mm of the intraarticular surface has been deemed unacceptable. Patients with >2 mm of residual displacement have been found to present with radiographic arthritic changes as early as 6 to 9 years post injury [25]. This residual displacement is often asymptomatic initially, but altered contact points can lead to poorer long-term outcomes [26]. Figures. 8A and 8B illustrate post reduction views of a 14-year-old boy with a Triplane with residual displacement. Figures. 9A, 9B, and 9C display the representive CT images of same patient. Various surgical techniques have been described based on surgeon preference. Choudry et al. concluded closed reduction with percutaneous fixation yielded good to excellent short and midterm results as long as the residual displacement was less than 2.5 mm [26]. Kim et al. showed good to excellent long-term results for those managed with open reduction and internal fixation [29]. Figures. 10A and 10B display post-operative images. The patient had a full recovery with no long-term sequel. Jennings et al. advocate for the use of arthroscopic assisted approaches. Their long-term results were comparable to that of traditional ORIF without need for open arthrotomy [30]. Regardless, the final goal remains the same, achieve near anatomic reduction, with <2 mm of incongruity. To obtain, various options can be utilized depending on surgeons preferred approach or experience.
Apophyseal Avulsions
As mentioned previously, the apophysis is a unique structure that develops parallel or oblique to the axis of the long bone. With the major function being the attachment of musclutendinous structures, which provide motion and stability [1]. The adolescent population is particularly at risk as the strong SOCs are contradicted by the weak physis [1]. In particular the weakest point is the zone of provisional calcification of the hypertrophic zone (1).
These injuries can account for 10% to 24% of athletic injuries in children and adolescents [31,32]. For the most part, apophyseal avulsions injuries are typically seen around the hip and pelvis [33], with injuries to the ischial tuberosity, anterior inferior iliac spine, and anterior superior iliac spine commonly seen [14]. These patients are at risk until fusion occurs across the physis. Typically, fusion takes place late in the teenage years and sometimes not until the mid-twenties [33].
Mechanism
Males are typically at higher risk for these injuries in the adolescent population [34]. The physis represents the weakest structure from osseous attachment to musculotendinous junction. Injury occurs when a strong eccentric load applied to the apophysis by the musculotendinous attachment. These injuries are commonly seen in sports as there is an incongruity between load tolerance and strain on the non-fused apophysis [35]. In the mature population, this similar mechanism would simply lead to ‘strains’ as the fused apophysis creates an area of stability.
Diagnosis
These injury patterns are challenging to diagnose and as they mimic soft tissue injuries seen in adult populations. This often leads to a misdiagnosis of muscle strain [33]. A careful history and physical examination is paramount in identifying these injuries.
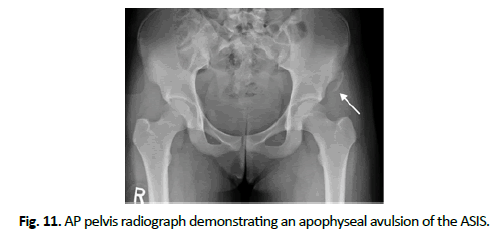
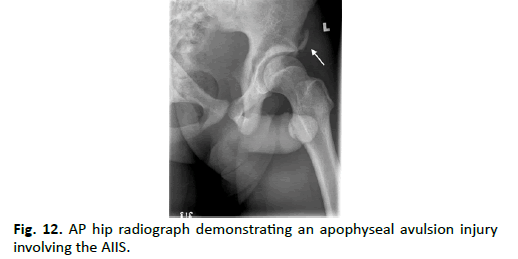
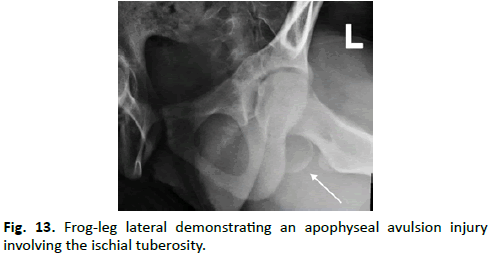
Patients typically present with localized pain and swelling to the area of injury [36]. Additionally, weakness or pain is often seen with active movement involving the injured apophysis. A concern with these injuries is misdiagnosis, which can lead to treatment delays and negative impacts on the patient. Plain radiographic are typically the first line of imaging. Three different patients with represented images all complained of discomfort around the hip. Figure. 11 displays an ASIS avulsion in a 13-year-old girl. Figure. 12 displays an AIIS avulsion in a 15-year-old boy, and Figure. 13 displays an ischial tuberosity avulsion in a 14-year-old girl. Imaging adjuncts including ultrasound and MRI can be used for uncertain diagnoses or high clinical suspicions without radiographic identification [37].
Management
The majority of these injuries can be treated non-operatively with symptom management. This typically entails a short period of protected weight bearing, usually 2 or more weeks, and avoidance of activities that cause discomfort [12]. Usually the patient can return to activities at around 6 to 8 weeks if symptom free. Indications for surgery are typically chronic disability and pain with failure of non-operative management, development of exostosis [38], or displacement of fragments > 2 cm [33]. Fracture displacement greater than 2 cm is considered a relative indication for surgical management. However, current literature is trending away from operative management. Kautnzer et al. compared outcomes of nonoperative vs. operative management of ASIS avulsion injuries. No significant difference was seen in achieving pre-injury function or long-term outcomes. Operatively treated injuries did show a faster return to pre-injury level but this was not significant [39]. In addition, a mildly elevated increase in heterotopic ossification was seen in the operative group but this was not statistically significant.
Patellar Sleeve Injuries
The patella begins to ossify at the age of 3 with the emergence of multiple SOCs around 5 to 6 years of age [40]. The pattern of ossification begins centrally and spreads peripherally [12,40]. Because of this ossification pattern, the peripheral rim is the most susceptible to injury because of the relatively weak cartilaginous tissue. Injury occurs when the cartilage sleeve is separated from the main ossified nucleus of the patella [12]. Interestingly, the cartilaginous sleeve is pulled off from nearly the entire circumference of the patella [40].
Mechanism
These injuries are typically see in adolescents between 8-16 yrs. of age, with males three times more likely than females. Sleeve fractures usually result from an indirect mechanism with a strong rapid contraction of the quadriceps on a flexed knee.
Diagnosis
The clinical presentation is sudden onset of pain following a powerful contraction of the quadriceps. Pain, swelling and ecchymosis are a common presentation. Most patients will be unable to extend the knee as the extensor mechanism is disrupted. Additionally, a palpable gap around the lower pole of the patella is appreciated [40]. In this patient population, it can be difficult to readily identify a fracture on radiographs as the cartilaginous sleeve will not be visible. Presence of patella alta and knee lipohemarthrosis will help to identify a sleeve injury on radiographs [12]. Ultrasound is another inexpensive imaging modality than can readily diagnose a sleeve fracture.
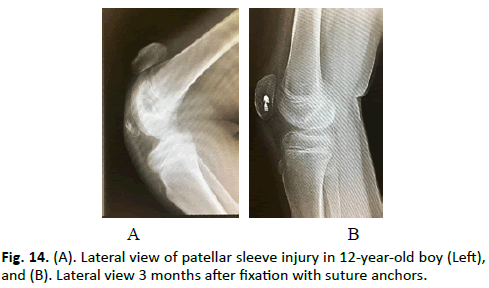
Treatment
Management for these injuries in most part depends on whether or not the extensor mechanism is intact. If it is disrupted, surgical management is the standard of care. Figures. 14A and 14B display the pre-and post-operative images of 12-year-old boy who sustained a patellar sleeve avulsion injury playing soccer. The goals of surgery are to restore patella height and patella tendon length [40]. This is accomplished by an open approach with trans osseous sutures, suture anchors, or a tension band construct [40].
Conclusion
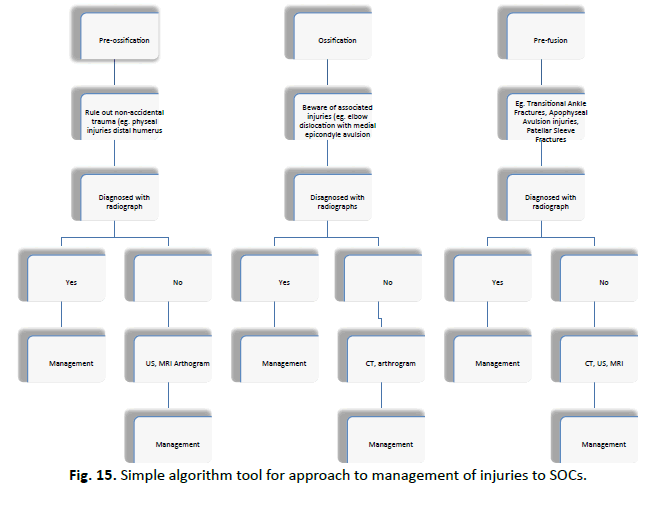
The goal of this review was to illustrate the variance in physeal injuries as they evolve during ossification and fusion. These patterns can be broadly broken down in to pre-ossification, ossification, and pre-fusion. This provides an understanding of particular patterns, mechanisms, diagnosis, and management options. Figure. 15 displays a simple algorithm tool that is utilized at our institution to help guide management for injuries to the SOCs. This is brief overview of the approach we use to teach the residents in and outside the orthopedic program. To date this is the most extensive review on the role of the secondary ossification center and its clinical importance.
REFERENCES
- Kishta W.E., Mansour E.H., Ibrahim M.M.: The accessory soleus muscle as a cause of persistent equinus in clubfeet treated by the Ponseti method: A report of 16 cases. ActaOrthop Belg. 2010; 76: 658-662.
- Ogden J.A.: Distal clavicularphyseal injury. ClinOrthopRelat Res. 1984;188: 68-73.
- Pritchett J.W.: Longitudinal growth and growth-plate activity in the lower extremity. ClinOrthopRelat Res. 1992; 275: 274-279.
- Jones J.C.W., Feldman K.W., Bruckner J.D.: Child abuse in infants with proximal physeal injuries of the femur. 2004; 20: 157-161.
- Abe M., Ishizu T., Nagaoka T., et al.: Epiphyseal separation of the distal end of the humeral epiphysis: a follow-up note. J PediatrOrthop. 1995; 15: 426-434.
- Sawant M.R., Narayanan S., O’Neill K., et al: Distal humeral epiphysis fracture separation in neonates -- diagnosis using MRI scan. Injury. 2002; 33: 179-181.
- Supakul N., Hicks R.A., Caltoum C.B., et al.: Distal humeral epiphyseal separation in young children: an often-missed fracture-radiographic signs and ultrasound confirmatory diagnosis. AJR Am J Roentgenol. 2015; 204: W192-W198.
- Navallas M., DÃÂaz-Ledo F., Ares J., et al.: Distal humeral epiphysiolysis in the newborn: utility of sonography and differential diagnosis. Clin Imaging. 2013; 37: 180-184.
- Gilbert S.R., Conklin M.J.: Presentation of distal humerusphyseal separation. PediatrEmerg Care. 2007; 23: 816-819.
- Tudisco C., Mancini F., De Maio F., et al.: Fracture-separation of the distal humeral epiphysis. Long-term follow-up of five cases. Injury. 2006; 37: 843-848.
- Red F., Children C., Town C., et al.: Jager, e. b. Hoffman. 73: 1991.
- Beaty J.R., James H., Kasser.: Rockwood & Wilkins’ Fractures in children. 6th Edition. 2006.
- Nenopoulos S.P., Gigis I.P., Chytas A.A., et al.: Outcome of distal clavicular fracture separations and dislocations in immature skeleton. Injury. 2011; 42: 376-380.
- Gottschalk H.P., Eisner E., Hosalkar H.S.: Medial epicondyle fractures in the pediatric population. J Am AcadOrthop Surg. 2012; 20: 223-232.
- Dodds S. D., Flanagin B. A., Bohl D. D., et al.: Incarcerated medial epicondyle fracture following pediatric elbow dislocation: 11 cases. J Hand Surg Am. 2014; 39: 1739-1745.
- Pathy E. R., Dodwell R.: Medial epicondyle fractures in children. CurrOpinPediatr. 2015; 27: 58-66.
- Farsetti P., Potenza V., Caterini R., et al.: Long-term results of treatment of fractures of the medial humeral epicondyle in children. J Bone Jt Surg. 2001; 83: 1299-1305.
- Kamath A.F., Baldwin K., Horneff J., et al: Operative versus non-operative management of pediatric medial epicondyle fractures: A systematic review. Journal of Children’s Orthopaedics. 2009; 3: 345-357.
- Pretell-mazzini J., Kelly D.M., Sawyer J.R., et al.: Outcomes and complications of tibial tubercle fractures in pediatric patients: A systematic review of the literature. J PediactricOrthop. 2015; 1: 1-7.
- Smith J.W.: The structure and stress relations of fibrous epiphysial plates. J Anat. 1962; 96: 209-225.
- Pandya N., Edmonds E.: Tibial tubercle fractures: Complications, classification, and the need for intra-articular assessment. J Pediatr. 2012; 32: 749-759.
- Ogden J.A., Southwick W.O.: Osgood-Schlatter’s disease and tibial tuberosity development. ClinOrthopRelat Res. 1976; 116: 180-189.
- Frey S., Hosalkar H., Cameron D.B., et al.: Tibial tuberosity fractures in adolescents. Journal of Children’s Orthopaedics. 2008; 2: 469-474.
- Zamzami M.M.: Ankle injuries in the growing skeleton: A review of the recent literature. Saudi Med J. 2012; 33: 830-840.
- Schnetzler K.A., Hoernschemeyer D.: The pediatric triplane ankle fracture. J Am AcadOrthop Surg. 2007; 15: 738-747.
- Choudhry I.K., Wall E.J., Eismann E.A., et al.: Functional outcome analysis of triplane and tillaux fractures after closed reduction and percutaneous fixation. J PediatrOrthop. 2014; 34: 139-143.
- Rohmiller M.T., Gaynor T.P., Pawelek J., et al.: Salter-Harris I and II fractures of the distal tibia: Does mechanism of injury relate to premature physeal closure? J PediatrOrthop. 2006; 26: 322-328.
- Eismann E.A., Stephan Z.A., Mehlman C.T., et al.: Pediatric triplane ankle fractures: Impact of radiographs and computed tomography on fracture classification and treatment planning. J Bone Jt Surg. 2015; 97: 995-1002.
- Kim J.R., Song K.H., Song K.J., et al.: Treatment outcomes of triplane and tillaux fractures of the ankle in adolescence. ClinOrthop Surg. 2010; 2: 34-38.
- Jennings M.M., Lagaay P., Schuberth J.M.: Arthroscopic assisted fixation of juvenile intra-articular epiphyseal ankle fractures. J Foot Ankle Surg. 2007; 46: 376-386.
- Lambert M.J., Fligner D.J.: Avulsion of the iliac crestapophysis: A rare fracture in adolescent athletes. Ann Emerg Med. 1993; 22: 1218-1220.
- McKinney B.I., Nelson C., Carrion W.: Apophyseal avulsion fractures of the hip and pelvis. Orthopedics. 2009; 32: 42.
- Moeller J.L.: Pelvic and hip apophyseal avulsion injuries in young athletes. Curr Sports Med Rep. 2003; 2: 110-115.
- Singer G., Eberl R., Wegmann H., et al.: Diagnosis and treatment of apophyseal injuries of the pelvis in adolescents. SeminMusculoskeletRadiol. 2014; 18: 498-504.
- Mbubaegbu C.E., O’Doherty D., Shenolikar A., et al.: Traumatic apophyseal avulsion of the greater trochanter: A case report and review of the literature. Injury. 1998; 29: 647-649.
- Coulier B.: Acute avulsion of the iliac crest apophysis in an adolescent indoor soccer. 2015; 99: 20-24.
- Hébert K.J., Laor T., Divine J.G., et al.: MRI appearance of chronic stress injury of the iliac crest apophysis in adolescent athletes. AJR Am J Roentgenol. 2008; 190: 1487-1491.
- Rajasekhar C., Kumar K.S., Bhamra M.S., Avulsion fractures of the anterior inferior iliac spine: the case for surgical intervention. IntOrthop. 2001; 24: 364-365.
- Kautzner J., Trc T., Havlas V.: Comparison of conservative against surgical treatment of anterior-superior iliac spine avulsion fractures in children and adolescents. IntOrthop. 2014; 7: 1495-1498.
- Hunt D.M., Somashekar N.: Review of sleeve fractures of the patella in children. Knee. 2005; 12: 3-7.



 Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.
Journal of Orthopaedics Trauma Surgery and Related Research a publication of Polish Society, is a peer-reviewed online journal with quaterly print on demand compilation of issues published.